Open treatment
1. Emergency treatment
Emergency treatment in orbital fractures is always indicated in the following situations:
- Partial or complete visual loss due to direct or indirect optic nerve trauma
- Severely increased intraocular pressure
- Acute space-occupying lesion creating increased intraorbital pressure (eg, retrobulbar hematoma, orbital emphysema)
- A severe shift of orbital content
- Severe entrapment of eye muscle (particularly in pediatric patients, “trapdoor”)
Globe rupture and intraocular trauma
These injuries require ophthalmological intervention.
Retrobulbar hematoma
A pressure increase in the periorbital region due to a retrobulbar hematoma can cause significant injury such as the creation of compartment syndrome with injury of the neurovascular structures and the possibility of vision loss.
Read more details about retrobulbar hemorrhage here.
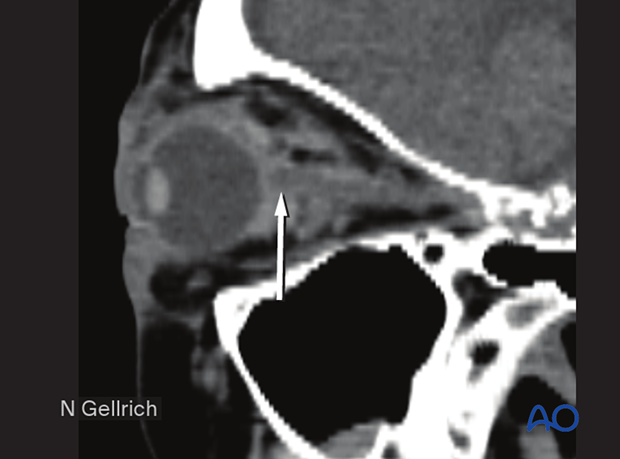
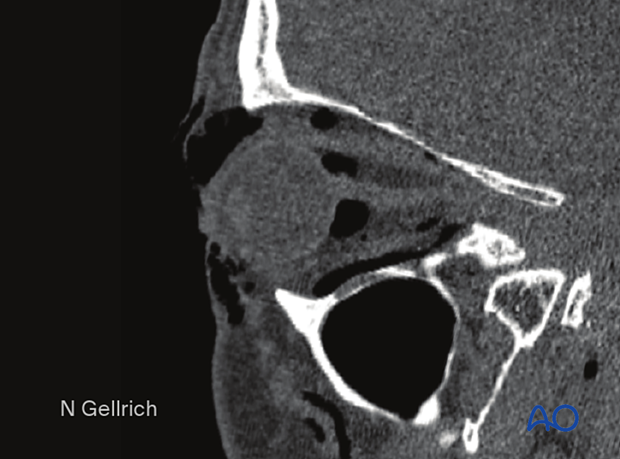
This CT scan sagittal view shows a small retrobulbar hematoma.
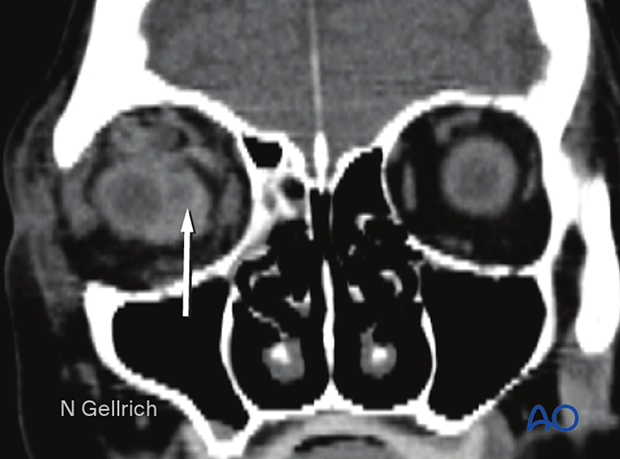
Coronal view of the same retrobulbar hematoma.
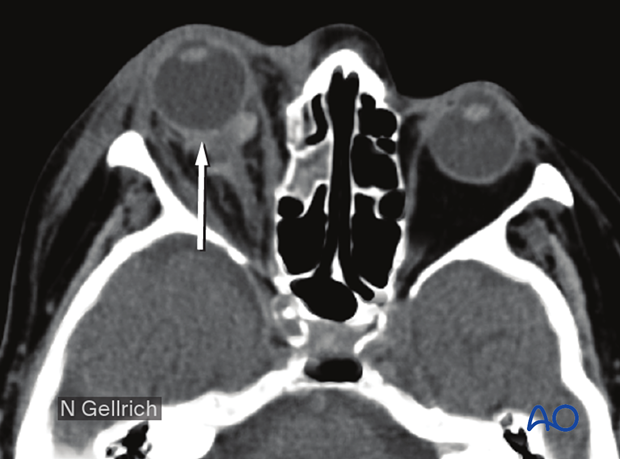
Axial view of the same retrobulbar hematoma.
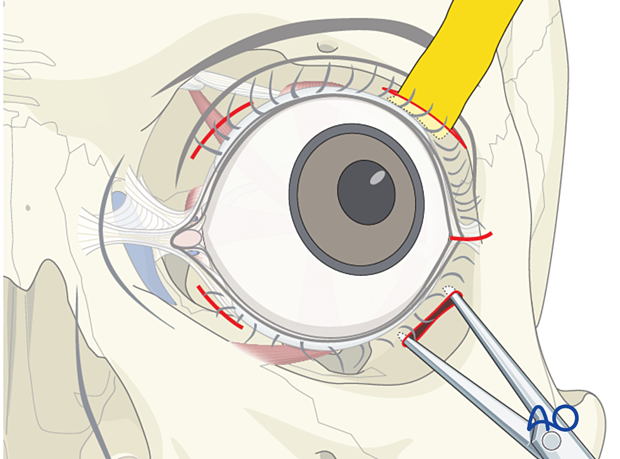
If a retrobulbar hematoma leads to a tense, proptotic globe with acute visual disturbances, emergency decompression should be initiated. This situation requires urgent decompression, such as cantholysis, removal of implanted reconstructive material, and/or evacuation of a loculated hematoma under general or local anesthesia.
Transcutaneous transseptal incisions help evacuate the hematoma and relieve excess periorbital pressure. Alternative methods such as transconjunctival pressure release, lateral canthotomy, and inferior cantholysis may also be considered according to patient condition.
An exception may be pulsatile exophthalmos which can be a sign of a carotid-cavernous sinus fistula. A fistula of this nature requires appropriate preoperative imaging and planning.
Emphysema
Severe emphysema might significantly raise intraorbital pressure. If this compromises visual function or endangers the orbital contents, orbital decompression must be considered.
Patients with signs of intraorbital emphysema are given antibiotics and decongestive nasal drops.
To avoid additional emphysema due to acute pressure rise, patients with sinus fractures in the periorbital region should not blow their nose. They should also be instructed to sneeze with an open mouth to minimize the increase of intranasal/intrasinus pressure.
Usually, there is no need for emergency treatment of orbital floor/medial wall fractures unless there is severe ongoing hemorrhage in the orbital cavity, the paranasal, or nasal cavity, or fractures which create muscle ischemia.
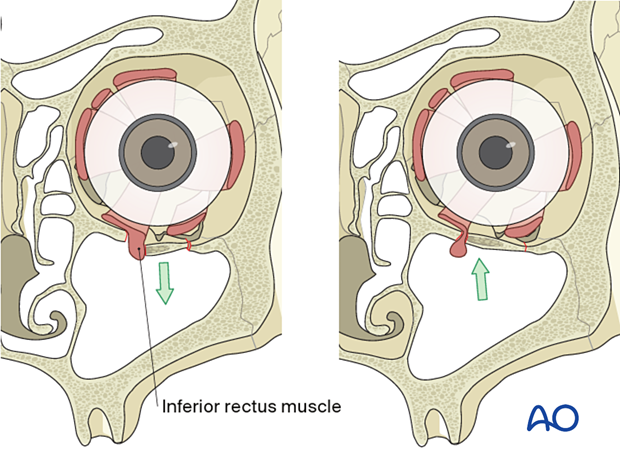
In younger patients there is a danger of necrosis of the entrapped rectus muscle due to the so-called "trapdoor" phenomenon. In such cases, immediate release of entrapped tissues is necessary.
More information on the trapdoor phenomenon can be found in the orbital reconstruction treatment for orbital floor fractures in the Surgery Reference pediatric trauma section.
Bone fragments affecting the optic nerve
Special attention should be given to the posterior third of the orbit, the superior orbital fissure, and the optic canal. Fractures and hematoma formation in these anatomical areas can be associated with superior orbital fissure syndrome and optic nerve injury.
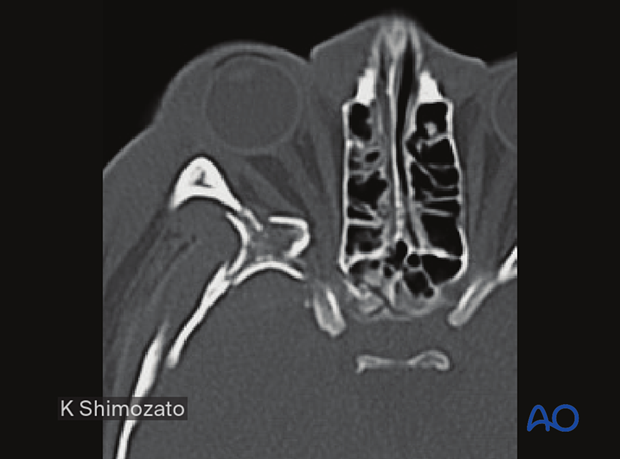
In this image the axial CT scan in the plane of the optic nerve shows multiple fractures of the lateral orbital wall and the greater wing of the sphenoid of the right side. Compression or displacement (stretching) of the optic nerve may be produced.
Displaced fracture fragments in the posterior third of the orbit may create nerve compression.
Severe bleeding
In case of severe nasal, oral, or pharyngeal hemorrhage, the following options should be considered:
- Assessment of current medical treatment for anticoagulation such as Coumadin, aspirin, or other antiplatelet medication
- Compression, either by nasal packing, balloon tamponade, or direct compression
- Electrocautery or ligation if a clear bleeding source can be identified
- Normalization of blood pressure
- Interventional radiologic embolization if simpler methods fail
- In some cases, reduction of fracture displacement may significantly reduce bleeding
2. Choice of reconstruction material
Reduction of the fractured, inferiorly displaced orbital roof fragment may be sufficient to obviate the need for internal fixation hardware.
General considerations
The unique and complex anatomy of the orbit requires significant contouring of the implants to restore the proper anatomy.
Most cases require reconstruction of the orbital roof to support the reduced bone fragments and restore the shape of the orbit. The reason for this is that the bony walls are comminuted, or bone fragments are missing. Therefore, one is reconstructing missing bone rather than reducing bone fragments. This can be accomplished using various materials.
There is hardly any anatomic region in the human body as controversial as this one in terms of appropriate material for use in fracture repair:
- Nonresorbable versus resorbable
- Autogenous/allogeneic/xenogeneic versus alloplastic material
- Standard versus custom-made plates
- Nonporous versus porous material
- Noncoated versus coated plates
Many surgeons recommend using materials that allow anatomical sculpting, which are radiopaque, inert, and won’t migrate.
The use of resorbable materials is not indicated. Use of resorbable materials may lead to secondary changes of the orbital contours over time, which is undesirable.
Modern imaging analysis offers a unique chance to quantitatively assess the surgical result and stability over time. This can provide valuable information for future recommendations.
In the case of an intra- or subcranial approach, fixation of the orbital roof might be accomplished from inside the anterior cranial fossa.
Orbital roof fractures differ from orbital floor and wall fractures due to the pulsating dura that lies above. The pulsating dura and associated micromovements can eventually resorb autogenous or absorbable materials.
Titanium mesh
Advantages include the following:
- Availability
- Stability
- Contouring (aided using a sterile artificial skull)
- Ideal for large defects or three-wall fractures (the prebent plate is limited to medial wall and orbital wall fractures only)
- Radiopaque
- Spaces within the mesh to allow dissipation of fluids and blood
- No donor site needed
- Tissue incorporation may occur
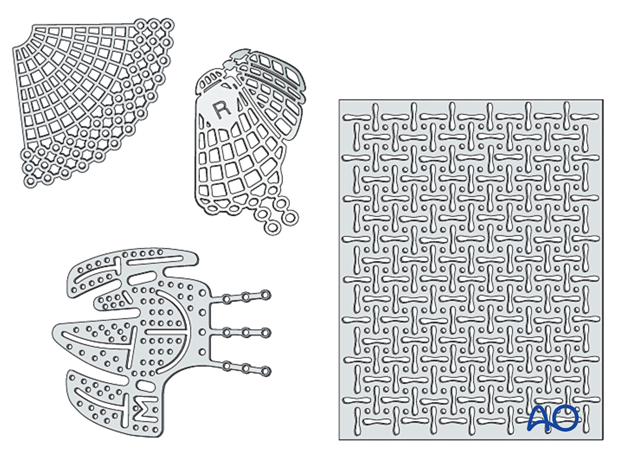
Disadvantages include the following:
- Cost
- Possible sharp edges if not adequately trimmed
Bone graft
Advantages include the following:
- Low material costs
- Smooth surface
- Variability in thickness
- Radiopacity
- Maximal biocompatibility
- Periorbita readily dissects off from the bone in secondary reconstructions
The illustration shows a calvarial bone graft stabilized by a titanium fixation plate.
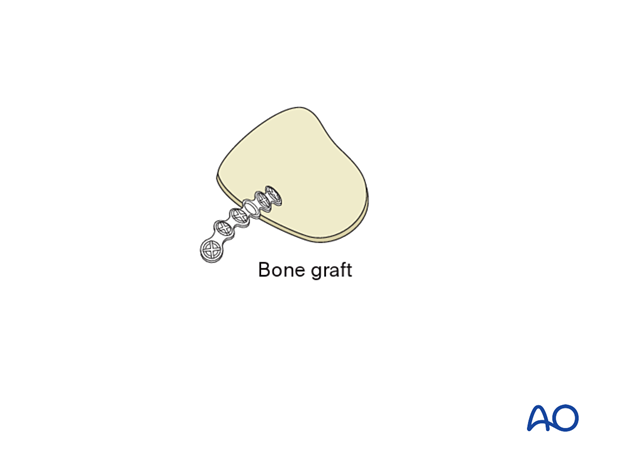
Disadvantages include the following:
- If not stabilized adequately, the bone can resorb
- Additional donor site needed (necessitating extra surgery time for harvest, pain, scar, and possible surgical complications)
- Possible contour and dimensional changes due to remodeling
- Difficult to shape according to patient’s anatomy
Composite of porous polyethylene and titanium mesh
AdvantagesA combination of titanium mesh and porous polyethylene is radiopaque and more rigid than porous polyethylene of a similar thickness. Some surgeons also believe that there is less risk of having retained sharp barbs, which can lead to entrapment of soft tissues during placement. This implant is designed to guarantee retention of a created shape, something which cannot be achieved by regular polyethylene without the memory provided by the titanium.
Other advantages are:
- Availability
- Stability
- Contouring (eased by a sterile artificial skull)
- Adequate in large three-wall fractures (the prebent plate is limited to medial wall and orbital wall fractures only)
- Radiopacity
- No donor site needed
- Tissue incorporation may occur
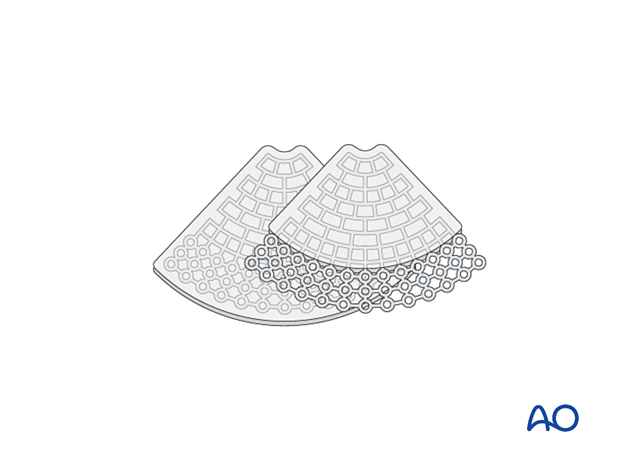
A composite of porous polyethylene and titanium mesh has the following disadvantage:
- Less drainage from the orbit than with titanium mesh
Resorbable materials (thermoplastic and non-thermoplastic)
Advantages include the following:
- Availability
- Handling/contourability (only for thermoplastics)
- Smooth surface and smooth edges
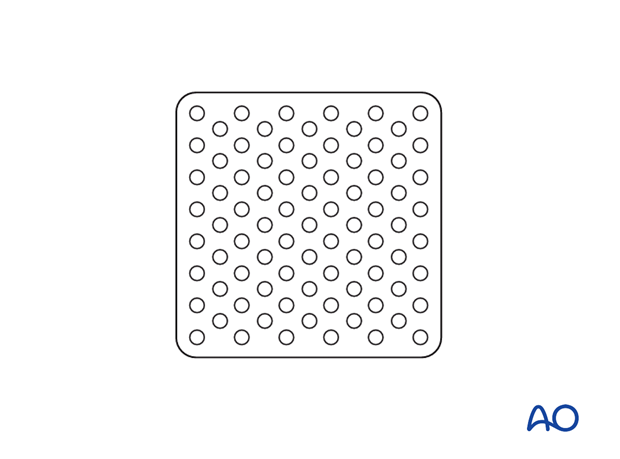
Disadvantages include the following:
- Non radiopaque
- Degradation of material with possible contour changes
- Sterile infection/inflammatory response
- Challenging to shape according to patient’s anatomy (only for non-thermoplastics)
- Non-perforated implants may not allow drainage of fluid or blood from the orbit
- Any material may have sharp edges if not properly contoured
The illustration shows a non-thermoplastic port delivery system (PDS) implant.
Implant fixation
Fixation of orbital reconstruction material varies with the type and nature of the fracture.
Fixation of most materials in the orbital floor is achieved using one or more screws. The diameter depends on anatomical requirements but will typically vary between 1.0 and 1.5 mm. Alternatively, other screw types can be used.
3. Selection of approach
Exposure of orbital roof fractures is performed most commonly via a coronal approach, via existing lacerations, and upper blepharoplasty incisions.
Once the orbital roof is exposed, periorbital dissection is meticulously performed.
Care should be taken at the superior-posterior medial aspect where the optic nerve and the superior oblique muscles can be found.
Additional information about orbital anatomy and dissection can be found in the links below:
- Preoperative considerations
- Anatomy of the bony orbit
- Correlation of surface and cross-sectional anatomy
- Introduction to periorbital dissection
- Orbital floor dissection
- Medial orbital wall dissection
- Lateral orbital wall dissection
- Orbital roof dissection
- Adjunctive access procedures (orbitotomies)
- Retrobulbar hemorrhage
4. Surgical exposure
Periorbital dissection
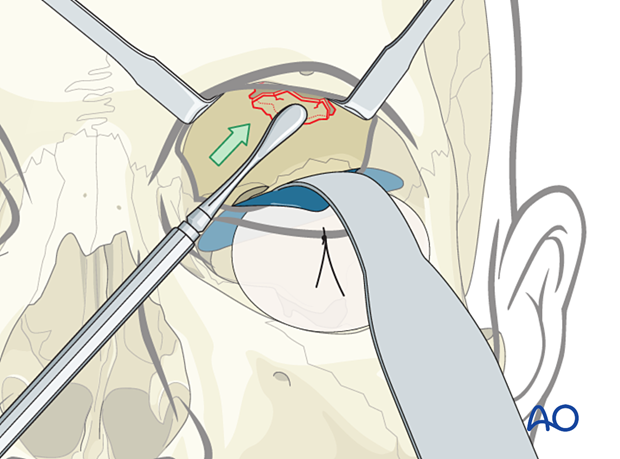
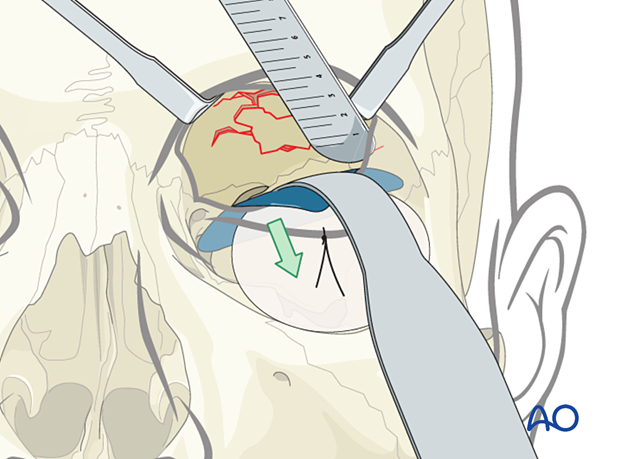
Periorbital dissection is performed after exposure.
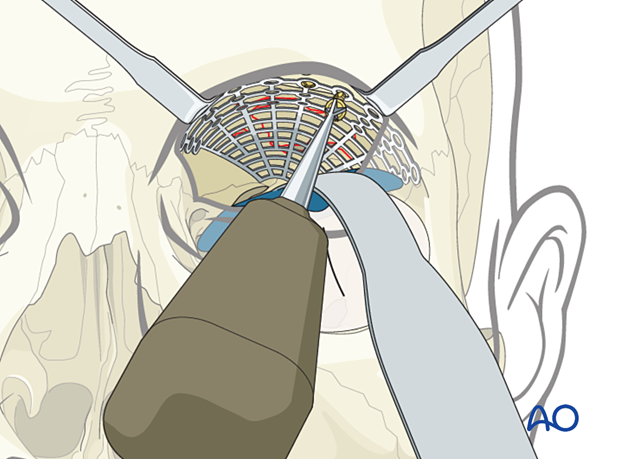
Retraction
Wide exposure and retraction, meticulous hemostasis, and good illumination (headlights, illuminated retractors) are critical to performing this procedure.
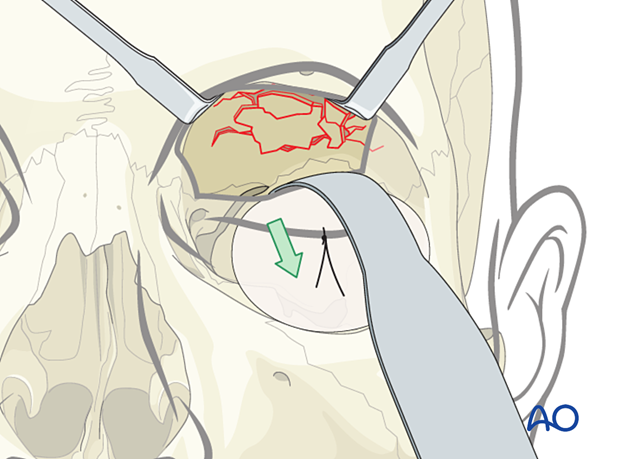
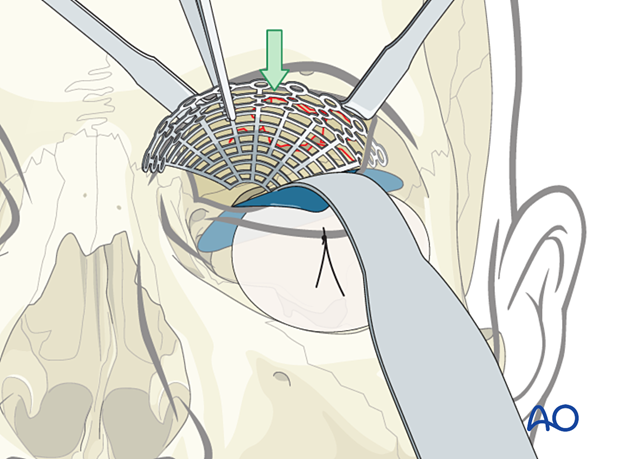
A foil (or sheet of other material) may help with retraction and help to avoid a prolapse of soft tissues, improve visualization, and prevent entrapment of soft tissues during implant placement.
The illustration shows the insertion of a foil above the retractor.
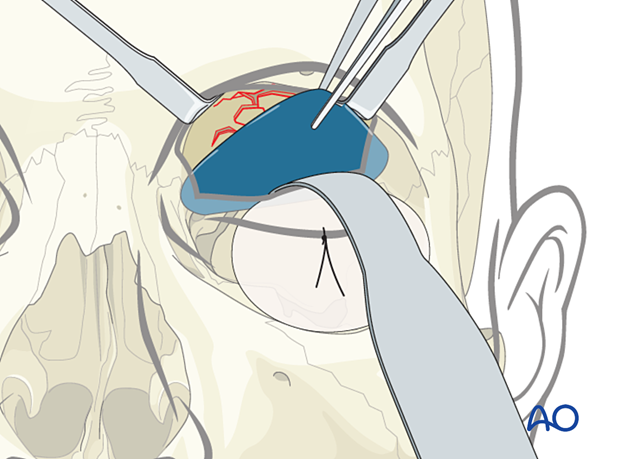
The retractor is removed, placed above the foil, and the orbital soft tissues are adequately retracted.
Helpful devices
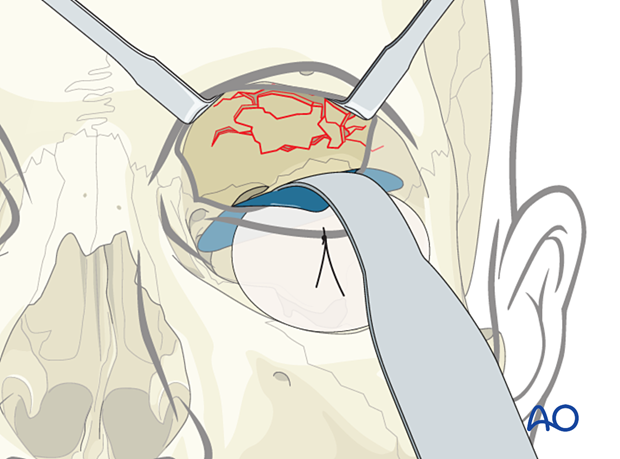
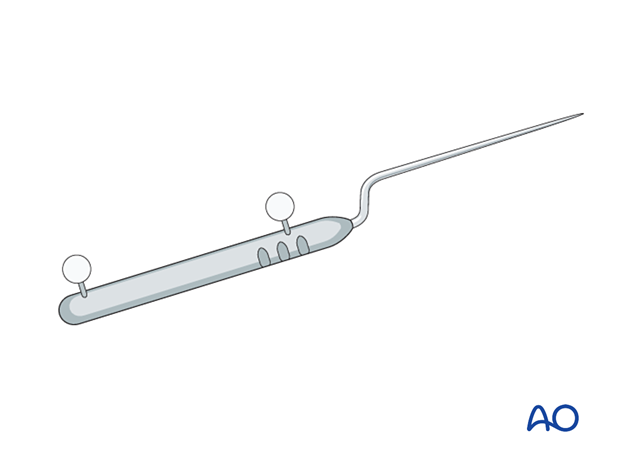
Many devices have been used to facilitate retraction of the orbital contents, including malleable retractors, spoons, and special orbital retractors designed for the globe (as illustrated).
5. Reduction only
In some cases, the orbital roof is reduced, and the fracture segment may be stable. Fixation may not be necessary. In these cases, the patient should have a close clinical and radiographic follow-up.
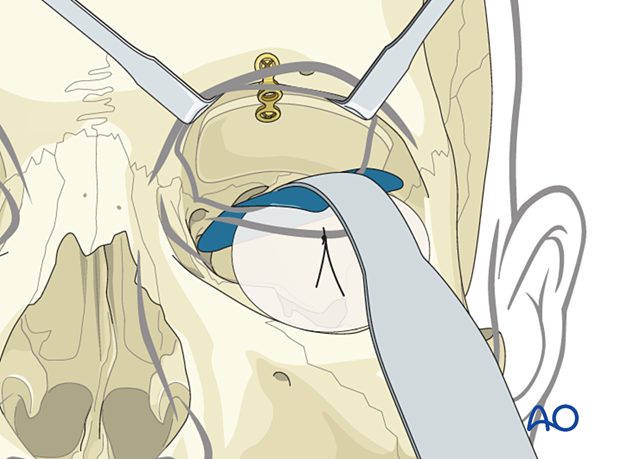
6. Reconstruction
Measurement of defect size and determination of implant size
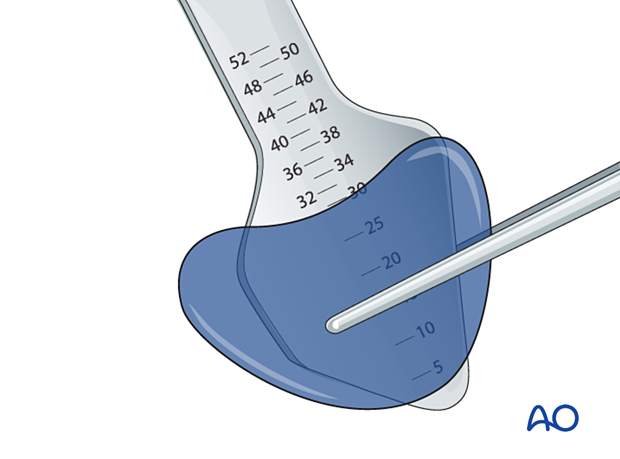
A careful assessment of the defect size should be performed preoperatively with the CT scan and confirmed intraoperatively by measurement.
It is controversial whether or not to extend the anterior part of the mesh over the supraorbital rim because it can cause discomfort and alter the aesthetics of the orbit. Whatever method is chosen (fixation anterior or posterior to the rim), the upper eyelid function must not be compromised.
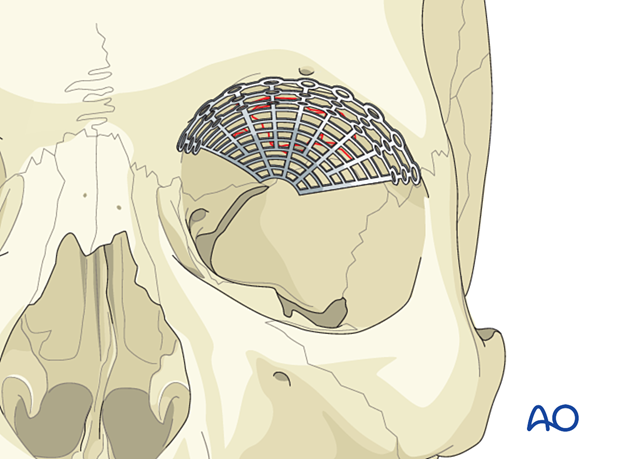
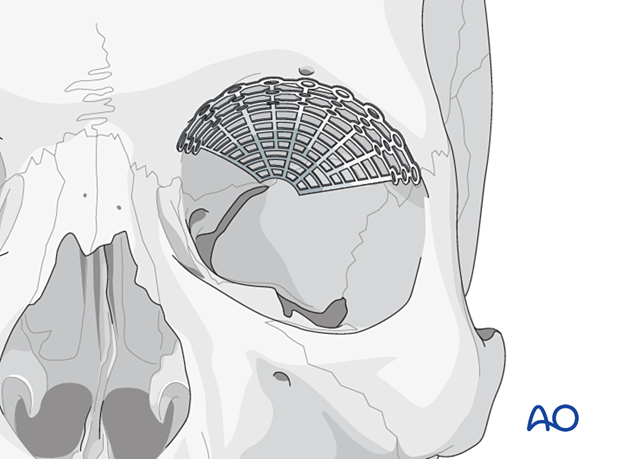
Example of reconstruction with titanium mesh
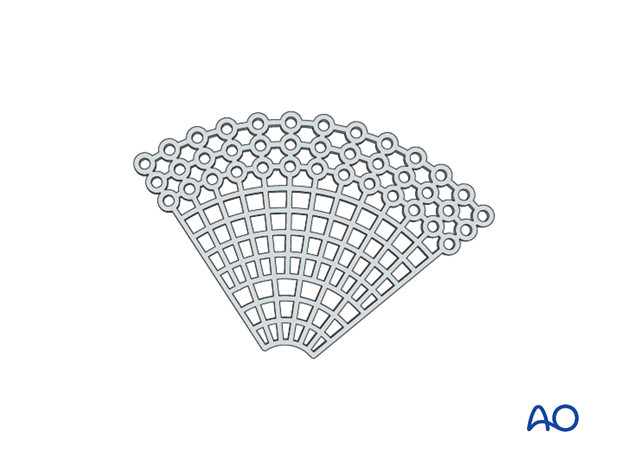
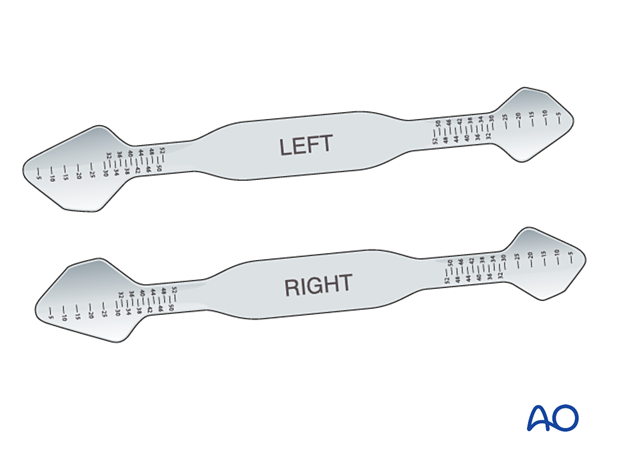
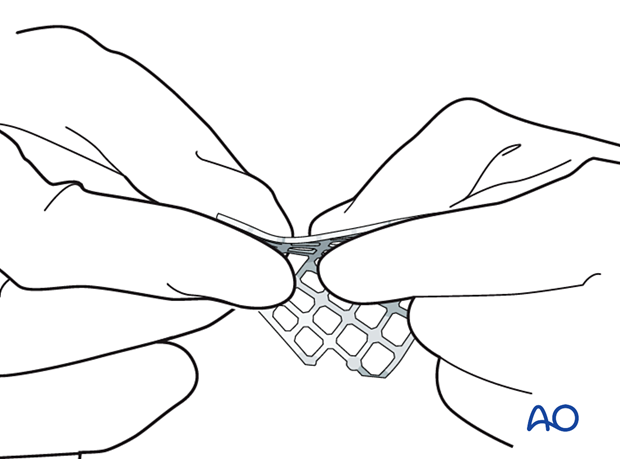
Firstly, the mesh is cut.
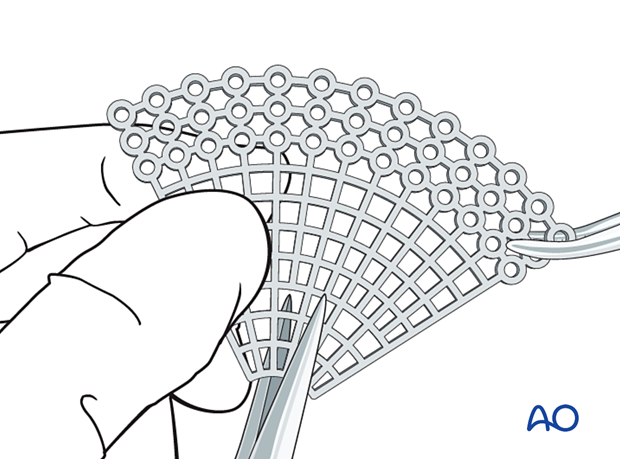
Then all sharp edges of the plate are trimmed off to protect the soft tissues (note the shape of the fan has only a minimum number of screw holes).
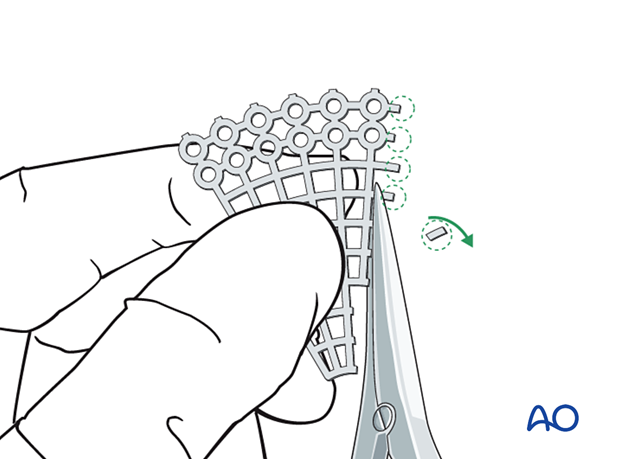
After that, the mesh is contoured to achieve the required shape and accommodate key anatomical structures (nasolacrimal duct, infraorbital nerve, and optic nerve).
It is advisable not to extend the implant further posterior than 5mm anterior to the optic canal entrance (if the posterior support bone of the orbit can be reached).
A sterile artificial skull allows proper anatomical contour of the implant.
- When using a fan-shaped plate, the outer circumference of the mesh is widest in the area of the supraorbital rim. The mesh should be trimmed so that the outer circumference is as small as possible but still provides enough width to cover the defect.
- The necessity for screw fixation varies with the fracture and type of material used.
Restoration of the normal anatomy can be achieved with meticulous shaping, positioning, and fixation of the implant. Care should be taken to ensure that no soft tissue is entrapped during implant placement.
Option: Computer assisted surgery
DICOM data can be used to generate 3D virtual models of the patient’s orbit, and a CAD-CAM custom shaped implant can be fabricated.
Further information about Computer Assisted Surgery can be found here.
Navigation
Additionally, navigation may serve for intraoperative control of implant or fragment position.
Modern 3D C-arm technology will further improve intraoperative quality control of implant positioning. Click here for more information.
Endoscopic visualization
Endoscopic visualization, either through the maxillary sinus or intraorbitally, may additionally confirm implant placement and lack of incarceration of periorbital soft tissue.
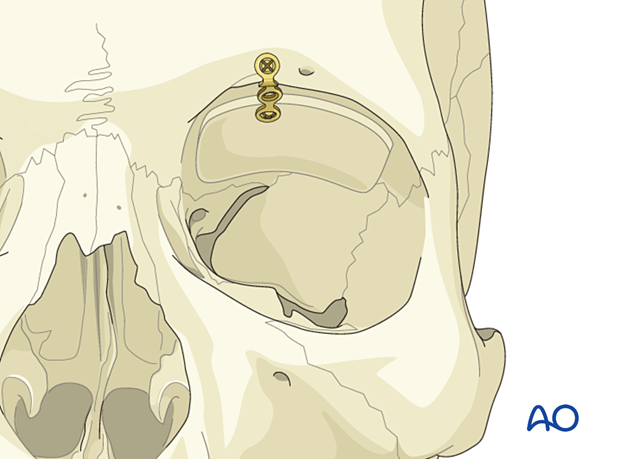
7. Fixation
Mesh fixation
Orbital roof implants must always be stabilized. Fixation is provided by at least one screw. The screw size must be appropriate for the chosen mesh type.
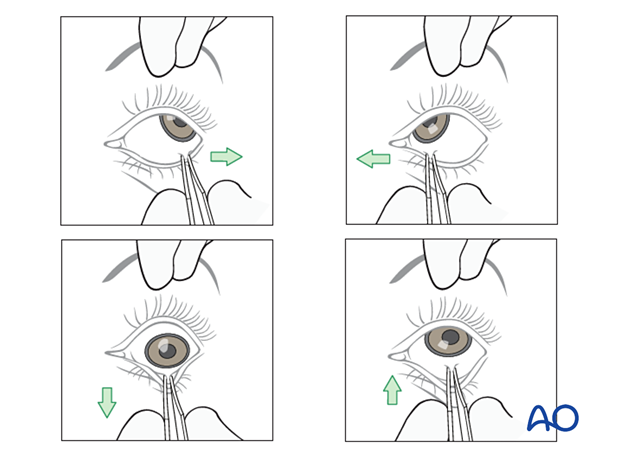
Forced duction test
After the insertion of an implant and before closure, it is imperative to perform a forced duction test and to examine the state of the pupil.
Alternative: Bone graft
If bone is harvested from a donor site, eg, cranial vault (parietal area), iliac crest, mandible, rib, etc, there may be donor site morbidity.
Once the bone is shaped to restore the normal anatomy, it should be rigidly fixed with plates and screws to limit micromovements and possible resorption.
8. Aftercare
Evaluation of the patient’s vision
Patient vision is evaluated on awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination must be performed but this is dependent on the appropriate equipment (VEP).
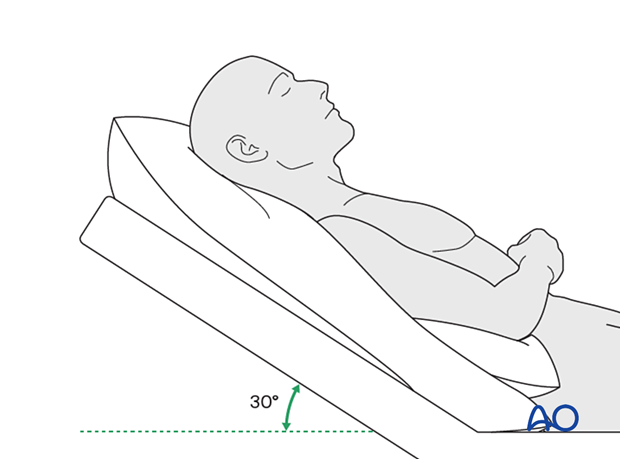
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin for seven days (nonsteroidal anti-inflammatory drugs (NSAIDs) use is controversial)
- Analgesia as necessary
- Antibiotics: many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in the case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field test
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
- If the patient complains of eye pain, evaluate for corneal abrasion
Postoperative imaging
Postoperative imaging must be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Wound care
Ice packs are effective in the short term to minimize edema.
Remove the sutures from the skin after approximately five days if non-resorbable sutures have been used.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
A soft diet can be taken as tolerated until adequate healing of the maxillary vestibular incision.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients that have fracture patterns that include periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Generally, implant removal is not necessary except in the event of infection or exposure.
Follow-up
The patient needs to be examined and reassessed regularly. Follow-up imaging at 3–6 months is helpful to ensure proper pneumatization of the sinuses (particularly, mucocele formation must be ruled out), sealing of the skull base, and stability of fragment position.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins.
Facial fractures may predispose to Eustachian tube dysfunction due to pharyngeal swelling. Forced air insufflation by holding the nose, closing the mouth and attempting expiration and the use of decongestants can relieve middle ear pressure and drum discomfort.
Mild pain on ascent or descent in airline travel may be noticed. Flying in unpressurized aircraft, such as military planes, should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.













