Preoperative considerations
1. Preparation
Preoperative planning of the surgical procedure is essential. Even in emergency scenarios optimal technical conditions must be assured.
Patient positioning is important.
Placement in the supine position with the head elevated (reverse Trendelenburg position) ensures adequate venous drainage and decreases bleeding.
Adequate illumination with a bright headlight and the use of surgical loupes greatly facilitate the procedure.
Basic oculoplastic surgical equipment with the addition of the following specialized instruments is recommended:
- Bayonet-shaped bipolar forceps
- Range of retractors (eg, Green, Mueller-Sewell, etc.)
- Malleable ribbon retractors (spatulas with metric markings of various shape: eg, round, triangular, pointed tip)
- Expandable/double fold ribbon retractors
- Periosteal elevators/dissectors/micro dissectors
- Small sized Titanium hemoclips
- Neurosurgical paddies/cottonoids
- Topical hemostatic agents (eg, epinephrine, gelatin sponge, oxidized cellulose, fibrin glue)
2. Special instrumentation
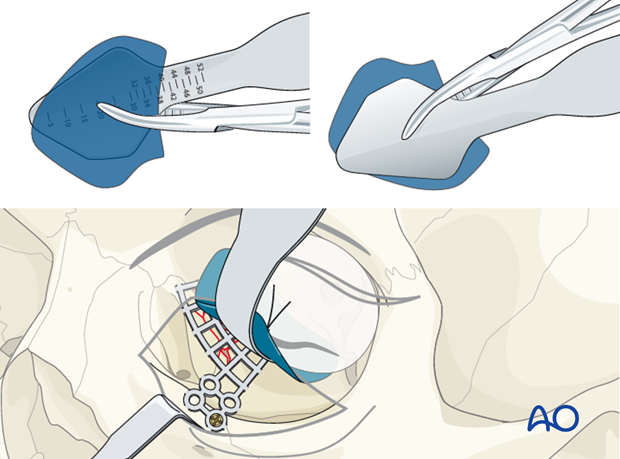
Orbital retractors of various shapes and sizes have been developed to improve orbital retraction and minimize soft tissues or fat prolapse during deep or extended periorbital dissection and insertion of implants used for orbital wall reconstruction.
A flexible polydioxanon (PDS) sheet can be used in conjunction with the orbital retractor to aid in the containment of the periorbital fat and insertion of the implant.
The illustration shows a flexible PDS sheet trimmed to the size of the anatomic dissection and used in conjunction with the retractor blade during fixation of a mesh implant at the infraorbital rim.
3. Endoscopic applications
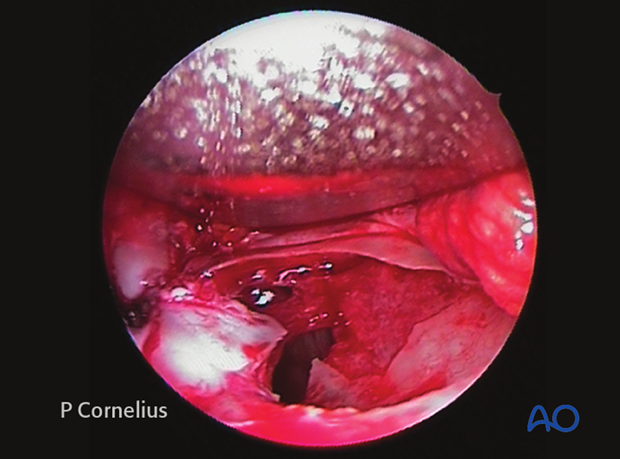
Endoscopes can also be used for transantral or transethmoidal approaches to the orbit.
This technique can be very useful to aid in the intraorbital exploration and correct placement of the orbital implant (ie, the posterior ledge). Endoscopic visualization is also a valuable adjunct for teaching and documentation purposes during intraorbital surgery.
An endoscopic view of a defect in the orbital floor after a lamellar fracture is shown (right orbit, endoscope positioned anteriorly). The soft tissues entering the inferior orbital fissure have been transected (left side of the photograph) to expose the entire defect, particularly the posterior bony ledge.
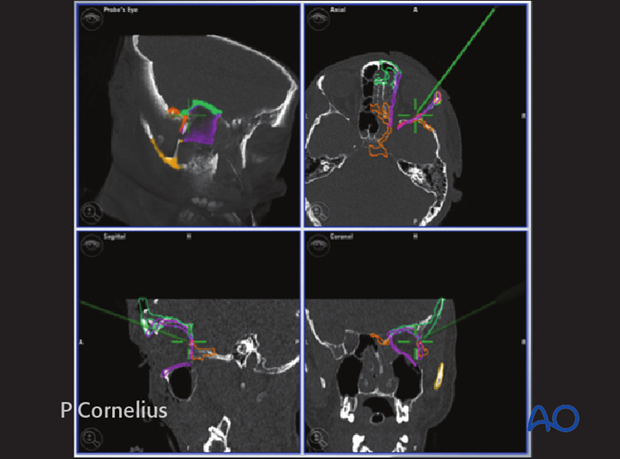
4. Intraoperative navigation and computer assisted surgery
CT based computer navigation assistance and intraoperative imaging (cone beam, CT) are useful tools for identification of the anatomy in deep, hard to visualize locations. Furthermore, mirroring of the intact contralateral structures can aid in precise orbital volume restoration and surface control of restored orbital walls.