Use of existing lacerations
1. Principles
General considerations
Facial fractures are often associated with lacerations. These existing soft-tissue injuries can be used to directly access the facial bones for the management of the fractures.
The surgeon may elect to extend the laceration to attain enough access to the fractured area, however this may not be as good as an elective incision.
Proper cleansing, debridement, and hemostasis should be accomplished before repairing injuries to the bone, the peripheral nerves, or Stensen’s duct (parotid duct).
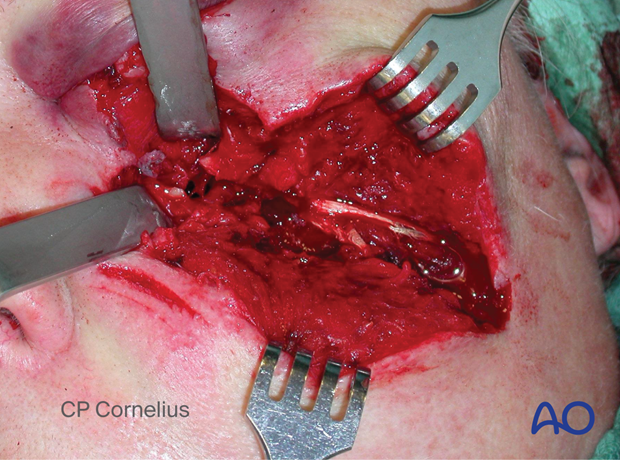
This photo shows an extended incision from the existing laceration to allow access to the infraorbital rim and orbital floor. Elective incisions are usually placed in boundary areas of esthetic units and/or along the relaxed skin tension lines (RSTL).
Bacterial contamination is not a contraindication for the use of existing lacerations for the surgical approach.

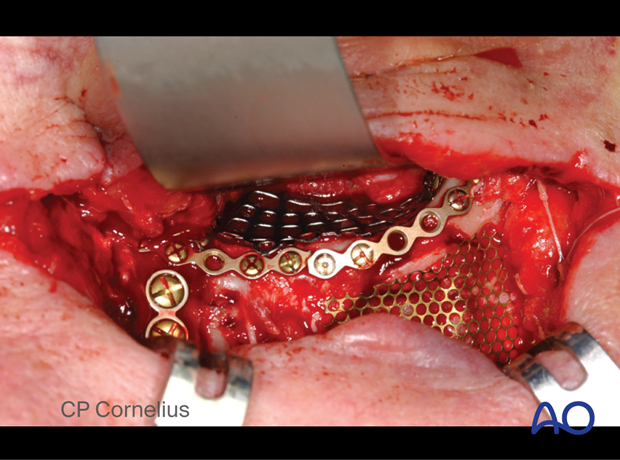
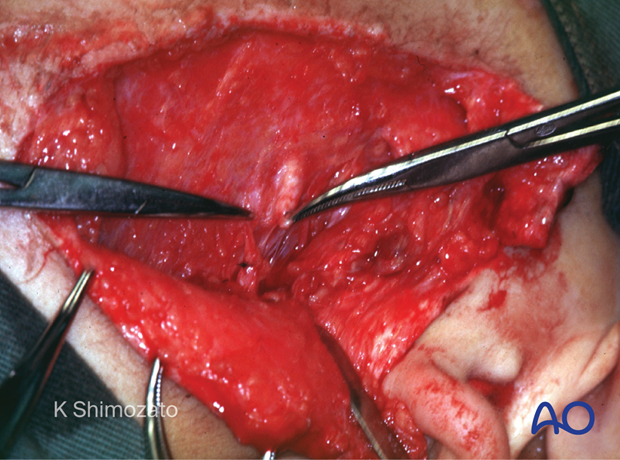
Clinical photograph of the same case showing osteosynthesis and orbital mesh plate applied through the extended laceration.
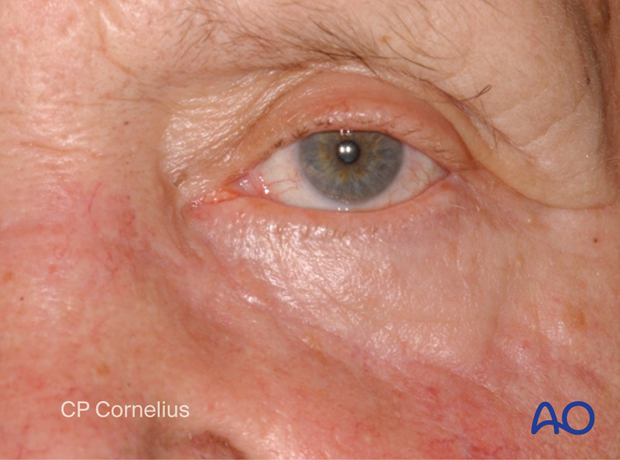
This photograph shows an acceptable outcome after using the extended laceration for the surgical approach.
Peripheral nerve and parotid duct injuries
Depending on the location of the laceration, structures such as nerves, the parotid gland, or the parotid and lacrimal ducts may be affected by the injury.
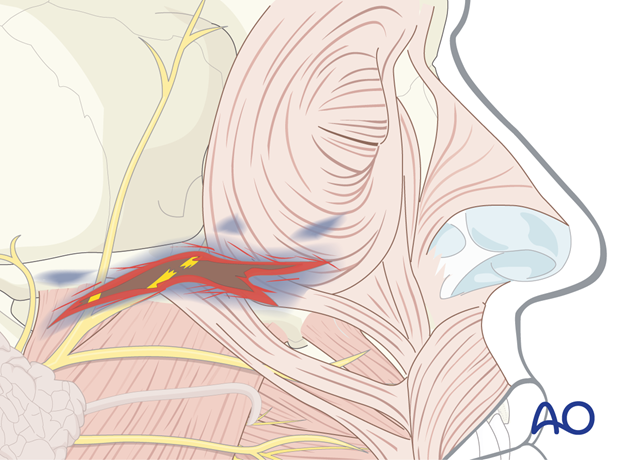
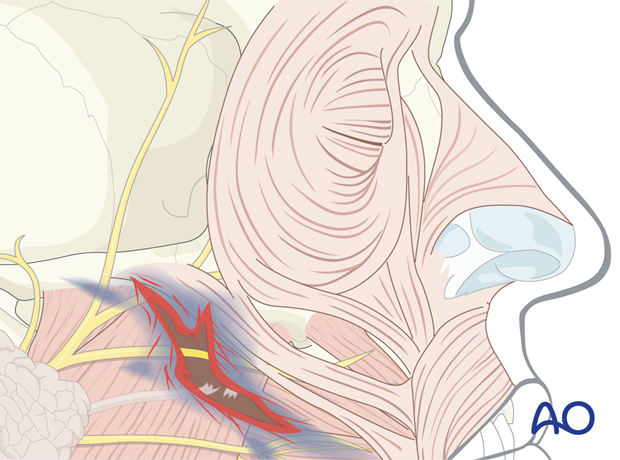
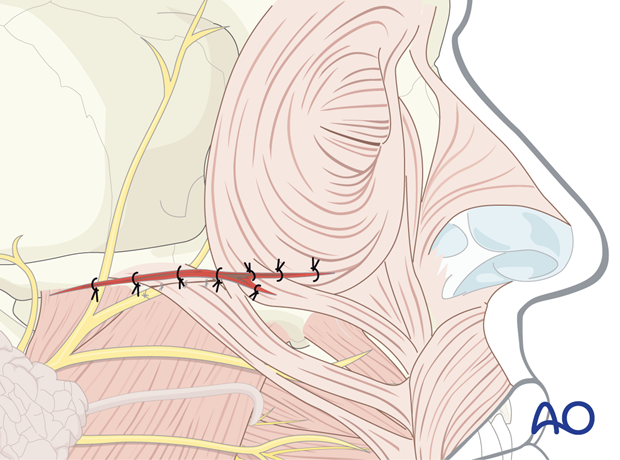
In the illustration, a peripheral facial nerve branch is directly involved. The facial nerve is best repaired primarily; however, it may be tagged and repaired in a secondary setting.
When in doubt, the lacrimal apparatus should be explored and repaired primarily.
Aggressive exploration of the facial nerve and primary repair under microscopic magnification are advantageous for ensuring normal facial animation and lid closure.
Parotid duct injury and repair
Injuries of the parotid duct may cause acute drainage of saliva into the wound or surgical field, resulting in a salivary fistula.
In such cases, the parotid duct should be explored through the laceration.
Repair of the parotid duct
The distal portion of the duct is cannulated from the intraoral orifice with silicone rubber tubing until continuity is reached with the lumen of the proximal duct (stenting the duct laceration).
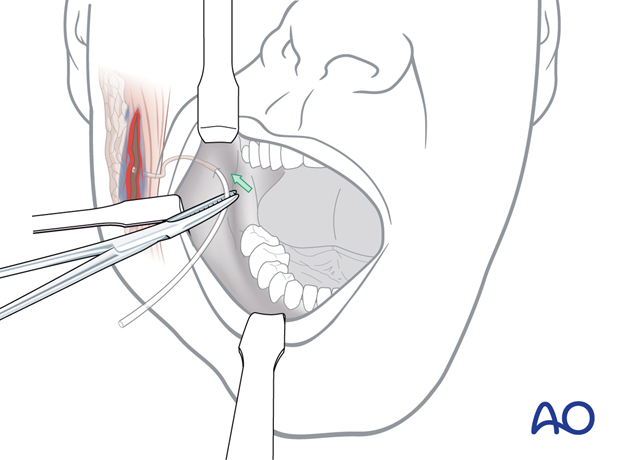
The edges of the duct are reapproximated and sutured over the stent using microsurgical instrumentation. The silicone rubber tubing is left in position for an extended period of 3 weeks to 3 months.
Unrepaired parotid duct injuries may result in a persistent salivary fistula or sialocele.
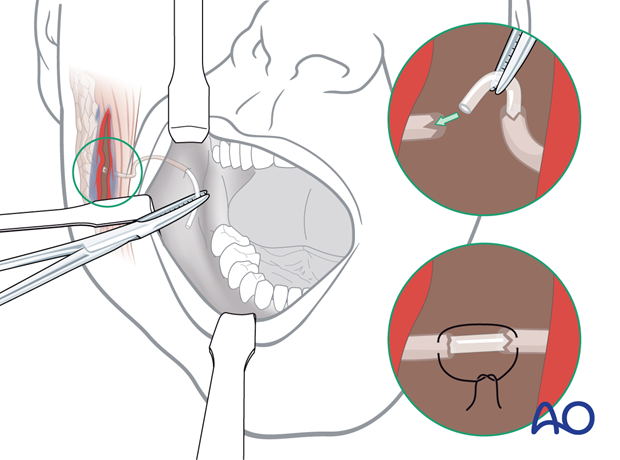
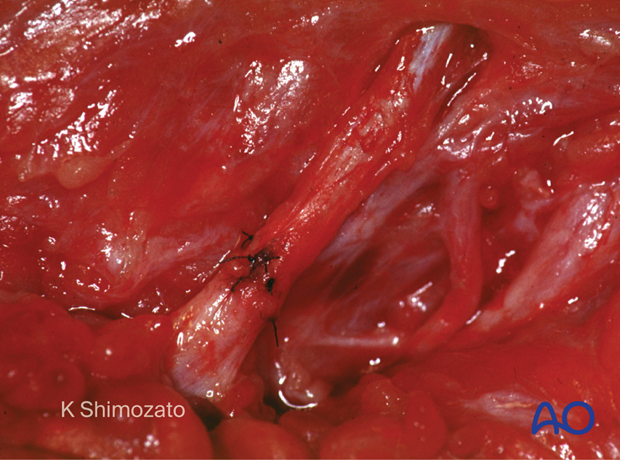
This clinical photograph shows a repaired parotid duct.
2. Wound closure
Facial wounds can be closed primarily up to 24 hours after the injury due to the high vascularity of this region.
Lacerations should be closed in a layered fashion. Devitalized skin margins should be debrided before closure.
A multilayered closure should be performed to eliminate dead space and realign the following:
- Periosteum
- Mimetic muscles
- Platysma/SMAS
- Subcutaneous tissues
- Epidermis
Particular attention should be given to the lips, nose, ears, and eyelids, where precise realignment of the aesthetic subunits is critical for best results. A variety of skin closure techniques are available based on surgical preference. A suction drain may be placed to reduce dead-space and prevent hematoma formation.
A bacteriostatic non-desiccating ointment should be applied to the skin closure.
3. Postoperative care and follow-up
Close monitoring of the early wound healing phase is necessary to detect infection or bleeding. Devitalized tissues should be debrided, and abscesses drained.
Skin sutures should be removed at 5-7 days to avoid suture markings (railroad tracks) on the skin.
Postoperative instructions should include the avoidance of direct exposure to the sun and the use of sunblock.
Patients should be informed about the natural evolution of scars. They should be reminded that facial scars require months to mature, lose their redness, and become less conspicuous. Secondary procedures may be necessary to improve aesthetics and minimize visible scars.
4. Examples of a facial laceration with underlying fracture
An example of a soft-tissue laceration after a horse-shoe injury.

Elevating the soft tissue reveals an underlying multifragmentary (comminuted) zygoma fracture.
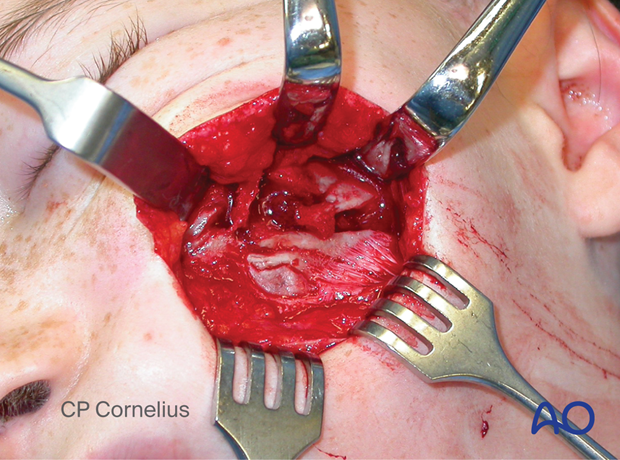
Another example of a soft-tissue laceration after a chain saw injury.

Elevating the soft tissue reveals an underlying multifragmentary fracture of the infraorbital rim and the orbital floor.