Periorbital dissection - Introduction
1. Introduction
The periorbita is the periosteum of the internal orbit and covers the four bony orbital walls from the anterior aperture of the orbital cavity back to the cone enveloping the optic canal and the superior orbital fissure.
Anteriorly the periorbita is continuous with the periosteum overlaying the orbital rims, the orbital septum in the upper and lower lids and the canthal structures.
The periorbita is not very adherent to the underlying bone except for its attachments to the suture lines, the trochlea and the lateral orbital tubercle.
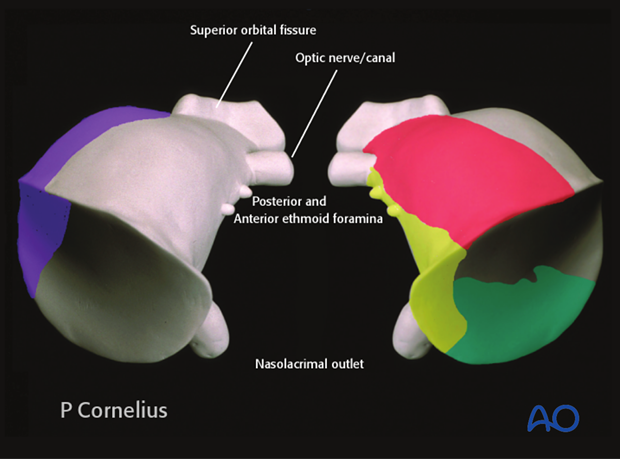
A sheath of the periorbita surrounds the inferior and superior orbital fissures. It connects to the dura within the optic canal as well as the superior orbital fissure.
The periorbita also extends into the anterior and posterior ethmoidal foramina as well as the nasolacrimal duct.
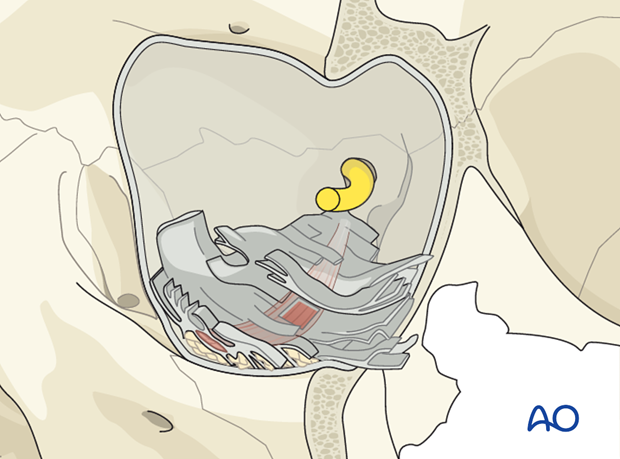
Elevation of the periorbita during the dissection opens up the potential space between the connective tissue layers of the periorbita and the bony surfaces of the internal orbit.
360° elevation of the periorbita in the anterior and midorbit allows ample access to reconstruct defects involving multiple walls.

A sheath of the periorbita surrounds the inferior and superior orbital fissures. It connects to the dura within the optic canal as well as the superior orbital fissure.
The periorbita also extends into the anterior and posterior ethmoidal foramina as well as the nasolacrimal duct.

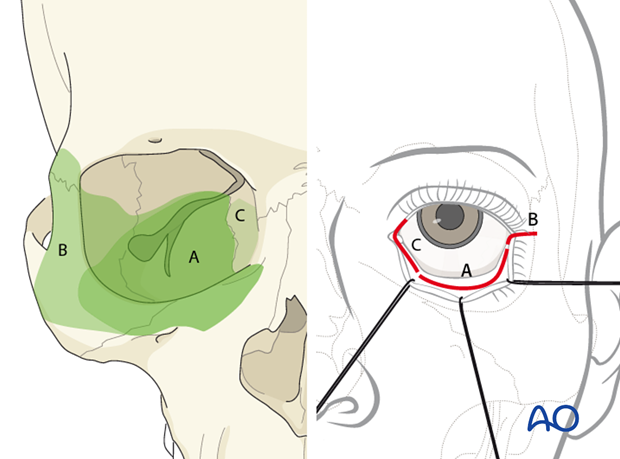
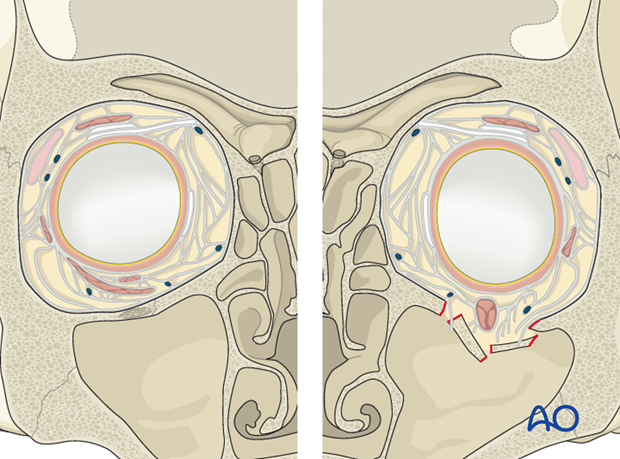
Surgical access to the orbital cavity can be achieved using a variety of transcutaneous and/or transconjunctival access incisions.
Depending of the topography of the injury or need for reconstruction, one or more of these approaches may be indicated as shown in the diagram.
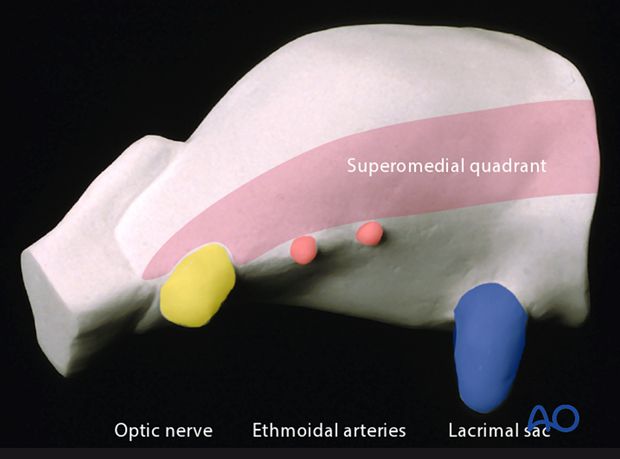
The orbital apex is usually not explored in trauma repair with the exception for surgical decompression in an acute optic neuropathy (visual loss/afferent pupil defect) or when the patient presents with signs of a superior orbital fissure syndrome.
When the superomedial quadrant needs to be explored, the addition of a superior surgical approach such as the coronal flap, will allow for the visualization of the frontoethmoidal suture line and anterior skull base region.
In general, every effort is made to maintain the integrity of the periorbita during elevation to prevent herniation of the orbital fat, obscuring the operator's view.
When an extended dissection into the orbit is required, transection of the periorbital envelope invaginating into the inferior orbital fissure and the soft-tissue overlaying Müller’s vestigial muscle will result in some prolapse of the orbital fat.
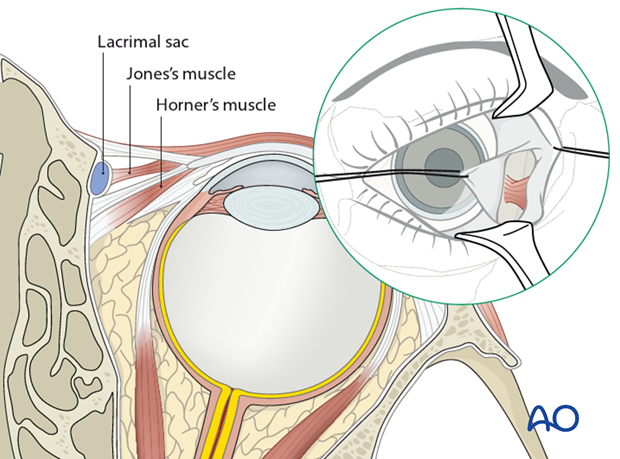
The pre/transcaruncular incision may also lead to fat prolapse as it proceeds posteriorly inside the periorbita between the medial rectus muscle and Horner ‘s muscle. A vertical incision is made then over the posterior lacrimal crest and the subperiosteal dissection can continue from this point.
Furthermore, a retroseptal transconjunctival approach to the orbital floor also leads to the prolapse of fat into the surgical field. A better alternative to avoid fat herniation is to use a preseptal approach to the orbital floor.
The periorbital dissection in the anterior midorbit should circumvent or avoid any disruption of the following structures:
- medial canthal tendons
- lacrimal apparatus
- origin of the inferior oblique muscle
- attachments to Whitnall’s tubercle
2. Connective Tissue Septa System
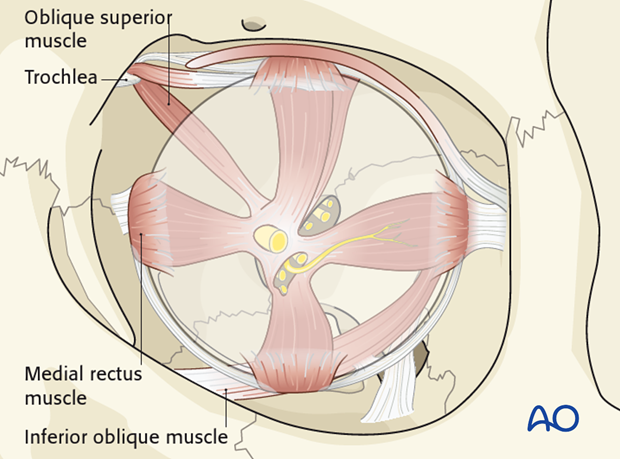
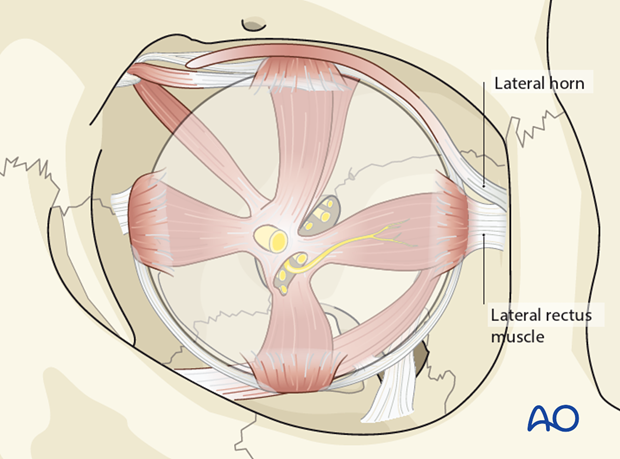
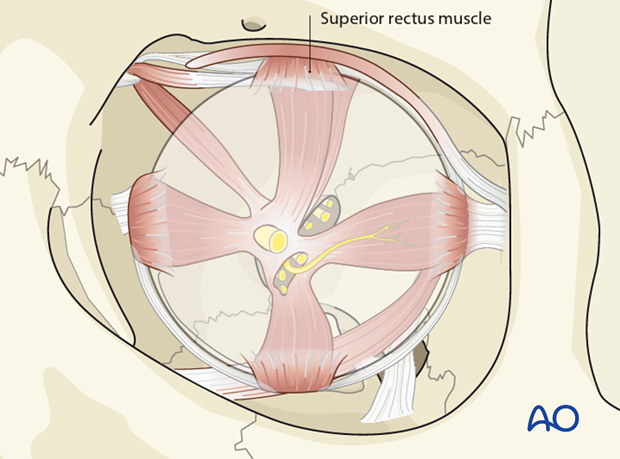
An intimately linked web of connective tissue septa surrounds the globe and all other orbital structures, including the extraocular muscles, the orbital vascular and neural elements connecting them to the periorbita.
Disruption and alteration in any portion of the delicate connective tissue septal system associated with trauma or surgical interventions may have widespread effects in areas of the orbit which are not primarily involved.
Globe motility restrictions after trauma rarely result from direct entrapment of the extraocular muscles but rather from herniation of the periorbita, orbital fat and the connective tissue septa into the paranasal sinuses. The prolapsed soft tissues exert traction on the muscle investments through the extensive septal interconnections.
Each eye muscle or eye muscle complex is embedded by its own connective tissue system with a special 3-dimensional architecture. The systems are characterized by (intraindividual) bilateral symmetry and interindividual uniformity.
For example in the inferior orbit the inferior rectus muscle is anchored by arch-like septa and is kept closely adherent to the orbital floor.
On the medial side of the orbit a craniocaudal orientation of the connective tissue septal system surrounds the medial rectus muscle.
This fascial system is more developed in the anterior and middle third of the orbit and less prevalent in the posterior third (orbital apex) .
At the apex, the periorbita fuses with the common tendinous ring (annulus of Zinn), from which the extraocular bulbar muscles originate.
3. Ligaments in Anterior Orbit
Many septal connections of the superior oblique muscle tendon spread between the trochlea and the medial levator aponeurosis.
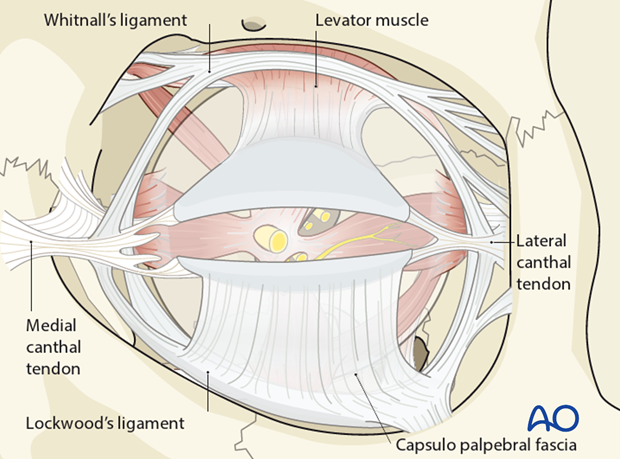
Whitnall’s ligament is a fibrous condensation of the levator palpebrae muscle forming a superior transverse band. It extends from the fascial layers investing the trochlea and the tendon of the superior oblique muscle to the superolateral orbital corner adjacent to the capsule of the lacrimal gland.
Whitnall’s ligament crosses the levator muscle about 8 to 10 mm above the musculoaponeurotic junction. The aponeurosis broadens and inserts into the medial and lateral retinacula behind the medial and lateral canthal tendons. These insertions are called the medial and lateral horns of the levator muscle.
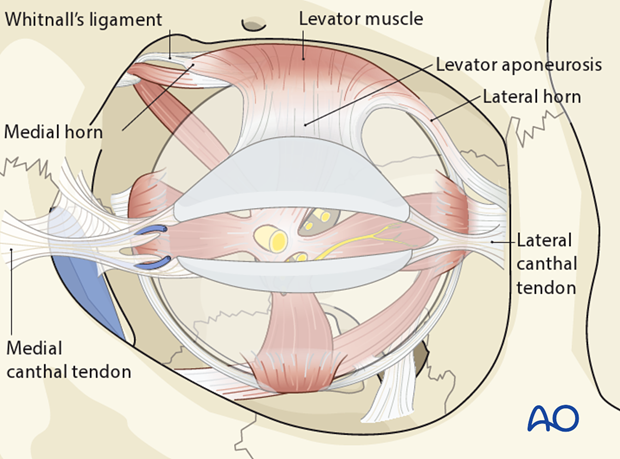
Lockwood’s ligament stretches across the inferior orbit and is analogous to Whitnall’s ligament in the upper lid. It acts as a support structure for the globe and extends from the lateral orbital tubercle to the medial canthal tendon. It is formed by the capsulopalpebral fascia and lies deep to it, anterior to the inferior oblique muscle.
The capsulopalpebral fascia, or the so-called lower eyelid retractors, send(s) fibre strands into the inferior fornix and into the septal connective tissue system at the base of the orbit.
4. Soft tissue landmarks
Some features of the connective tissue septal system are important to note during a periorbital dissection along the orbital walls:
Orbital floor
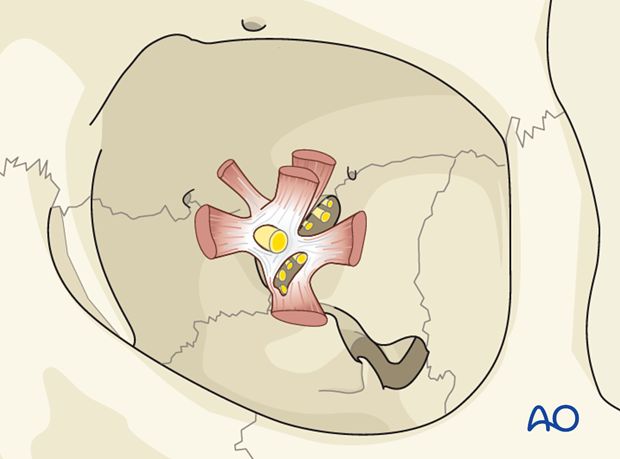
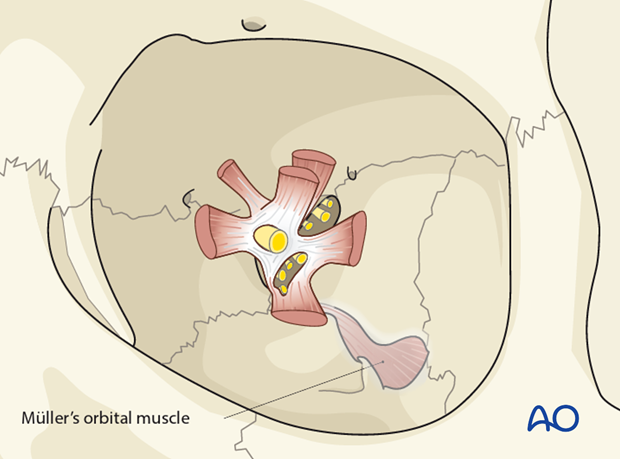
Müller’s orbital muscle covers the inferior orbital fissure and separates the orbital contents from the pterygopalatine and infratemporal fossa.
In the posterior third, the inferior rectus muscle is connected to Müllers orbital muscle by a number of septa. These must be sharply transected to achieve access to the bony surface.
Orbital floor/Medial orbital wall
At the level of the lacrimal duct, vertical connective tissue septa connect the inferior oblique muscle to the caudal portion of the medial rectus muscle. This area is entered when a combined pre-/transcaruncular and a lower conjunctival fornix approach is utilized detaching the insertion of the inferior oblique muscle. Dissection between the muscle bellies should be kept at a minimum.
The superior oblique muscle belly runs in a distinct fat tissue compartment and is located directly adjacent to the periorbital layer along the medial orbital wall. Care should be taken not to open this sleeve inadvertently when the trochlea is detached.
Lateral orbital wall
A compact sagittal septal layer is anchored to the periorbita adjacent to the entire lateral orbital wall by numerous finger-like radial connective tissue strands. This provides a resilient safeguard against shearing injuries.
Orbital roof
This rather thick lining space located under the horizontal orbital plate of the frontal bone is interrupted in the midorbit where the levator palpebrae lies directly below the periorbita. The levator palpebrae is at risk for injury if the protective periorbital layer is penetrated during the stripping procedure.
Safe surgical exploration distances
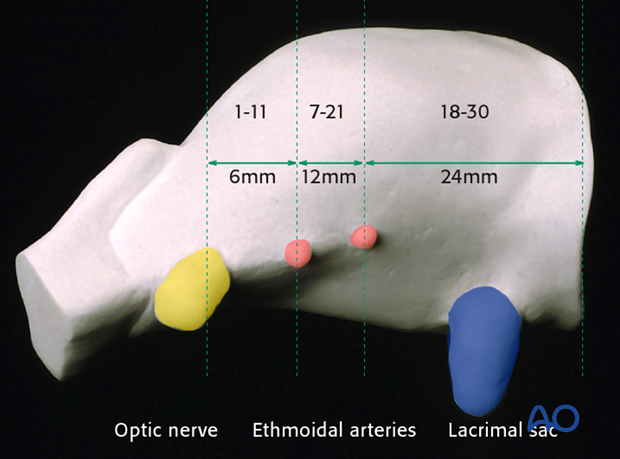
Safe distances for the periorbital dissection from the intact outside rim of the adult orbit to vital interior structures are specified in millimeters.
Generally an exploration depth of 25 mm along the lateral and inferior walls is regarded as safe.
A 30 mm distance from the supraorbital rim and the anterior lacrimal crest are also considered safe exposure of the roof and the medial wall respectively.
Along the medial wall, important landmarks are described as measurements from the anterior lacrimal crest :
- 24 mm* to the anterior ethmoidal foramen
- 36 mm* to the posterior ethmoidal foramen (12 mm from the anterior ethmoidal foramen)
- 42 mm* to the optic canal (6 mm from the posterior ethmoidal foramen)
* Mnemotechnic formula (rule of halves): 24-12-6.
The range of these distances is indicated in the illustration.
NOTE: These values may be inaccurate if there is displacement or absence of the reference landmarks in the injured orbit.
Furthermore one must also take into account anatomic variations such as duplication or absence of the posterior ethmoidal artery. Therefore it is recommended to identify the surface anatomy on the way into the deep orbit in a robe ladder fashion and interrelate the anatomic landmarks.
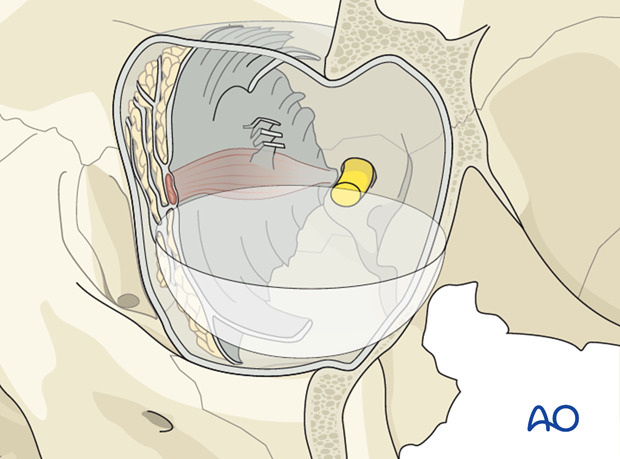
Safe surgical exploration
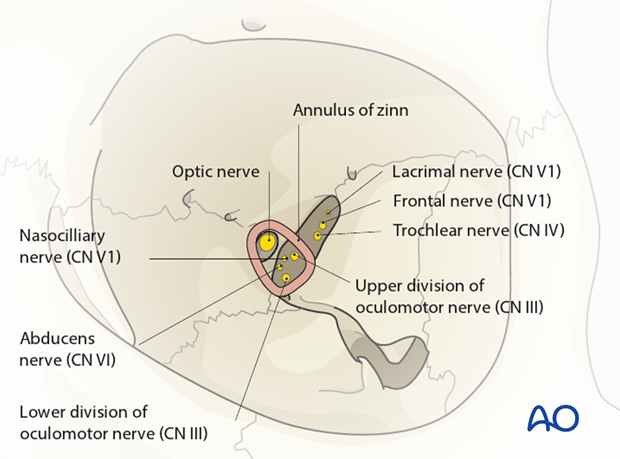
The periorbita can be safely elevated outside the anulus of Zinn and the superior orbital fissure. Deep dissection of the periorbita stops at this level.
A safety margin of 1 cm anterior to the optic canal must be maintained during dissection and reconstruction of the orbital walls.
The superior orbital fissure is divided into a two compartments by the lateral portion of the anulus of Zinn.
The lacrimal and frontal branches of the ophthalmic trigeminal division (V1) and the trochlear nerve run through the opening above the anulus.
The oculomotor nerve, the abducent nerve and the nasociliary nerve (branch of CN V1) pass through the anulus.
Branches of the ophthalmic veins are variable and may pass above, inside or below the anulus.