Bony anatomy of the orbit
1. Introduction
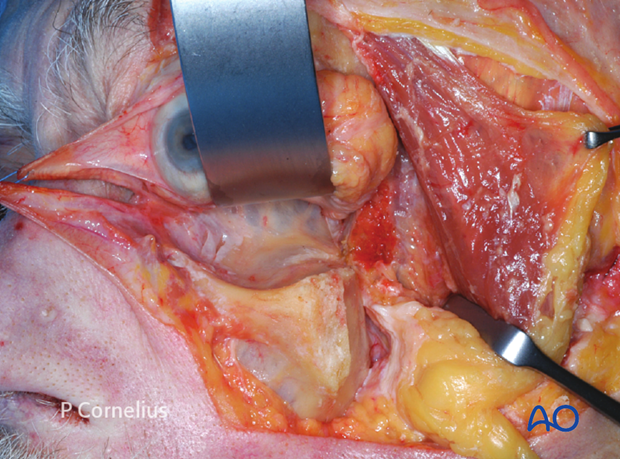
A thorough understanding of the complex surface bony contours of the internal orbit is essential to avoid critical structures and achieve a safe periorbital dissection.
Though it is possible to reformat CT scans into a 3 dimensional surface rendering of the internal orbit using segmentation, often times only axial, coronal and sagittal slices are available. These need mental extrapolation to figure out how to proceed during real life periorbital dissection.
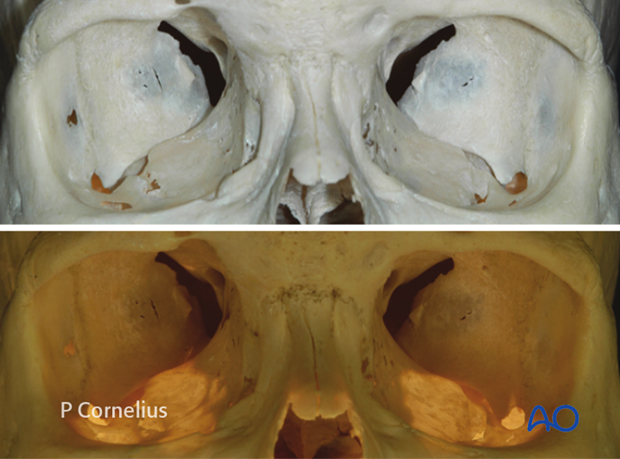
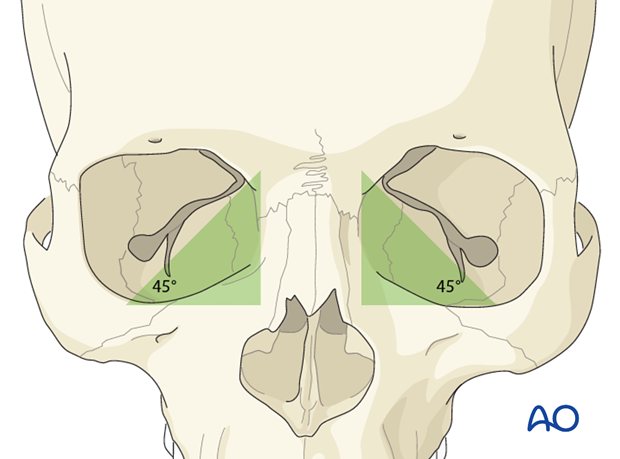
In order to best appreciate the subtle nuances of the intraorbital anatomy, such as the 45° angulation of the orbital floor, it is helpful for the surgeon to refer to anatomical skulls on a regular basis to familiarize himself with the unique anatomy. Furthermore, sterilizable skulls are also available for intraoperative reference.
The position, size and shape of the inferior and superior orbital fissures are some of the basic landmarks for topographical orientation during the surgical approach.
The bony orbital walls are referred to as the:
- floor (or inferior wall)
- roof (or superior wall)
- medial wall
- lateral wall
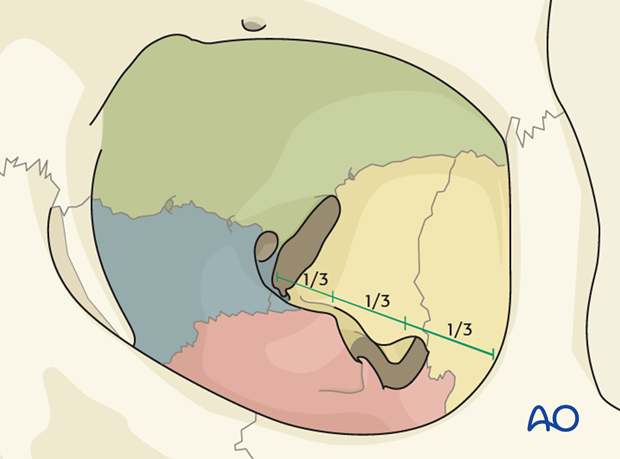
The orbital floor extends from the rim to approximately two thirds of the depth of the orbit, where it curves medially as the posterior medial border of the inferior orbital fissure and blends with the medial wall.
Only three of the four orbital walls, the medial, the superior and the lateral walls extend into the apex.
The length of the lateral orbital wall from the rim to superior orbital fissure is about 1.0 cm shorter than the medial wall and appears even shorter owing to the different angulation and the more posterior position of the lateral rim.
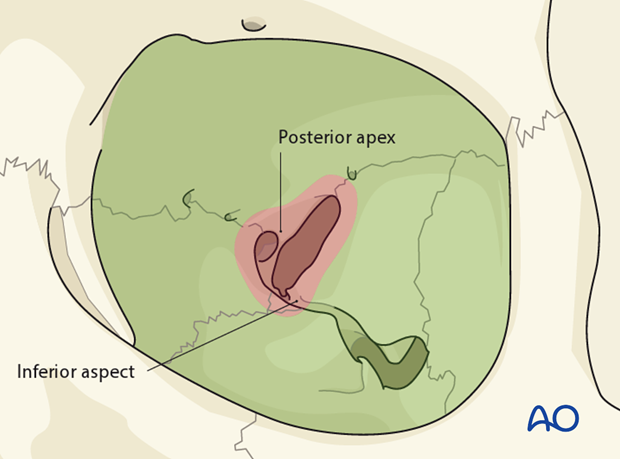
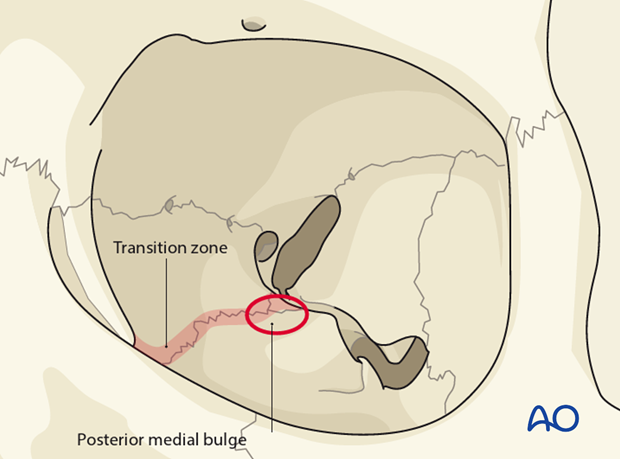
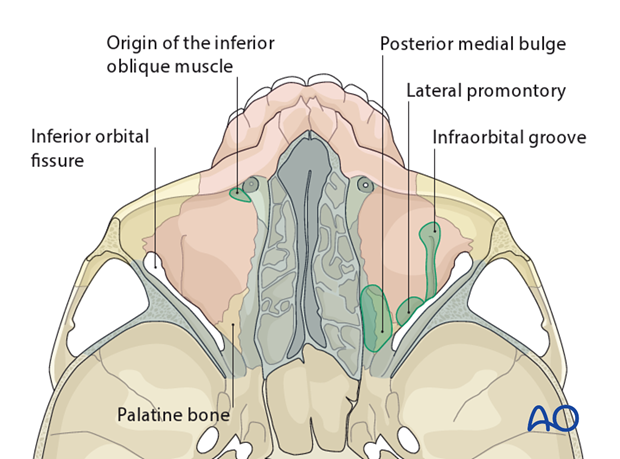
The posteromedial aspect of the orbital floor transitions into the medial orbital wall, to form the “posterior medial bulge”, a structure frequently involved in orbital fractures.
Fragmented bony lamellae and orbital soft tissues usually prolapse into the air filled paranasal sinuses, (ie, the maxillary antrum or ethmoid sinus), resulting in an increase in the orbital volume.
Similarly, a decrease in volume and compression of the orbital contents occurs when orbital wall fragments are displaced into the orbit.
2. Floor of the orbit
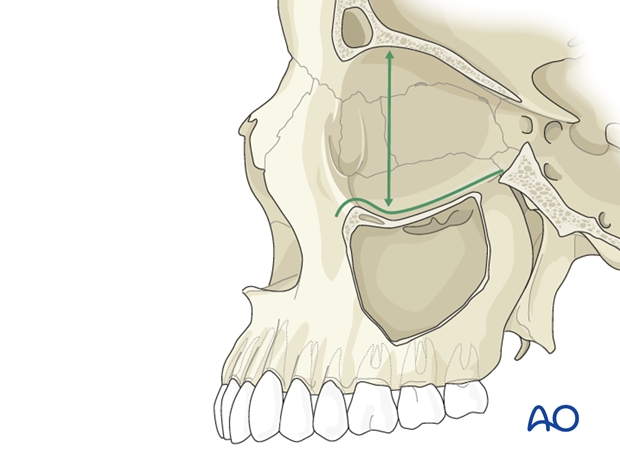
In the anterior third of the orbit the diameter widens immediately (about 1 to 1.5 cm) behind the superior and inferior margins, thus forming an overall concave shape in the sagittal plane, the ‘post entry concavity’.
As a consequence, the initial subperiosteal dissection must proceed in an inferior or superior direction as one dissects the the floor or roof respectively.
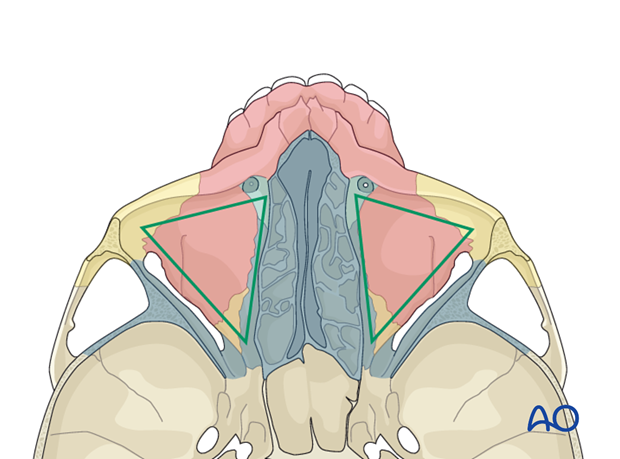
The floor of the orbit with it's triangular shape has the shortest surface of all orbital walls.
In the frontal plane it slopes downward from medial to lateral with an intermediate convexity at the midorbit level.
Behind the postentry concavity, the floor is separated from the lateral wall by the inferior orbital fissure.
In the sagittal plane the floor has a lazy S shape with the upper ledge at the height of the orbital process of the palatine bone (posteriorly) and extending downward to the infraorbital margin (anteriorly).
In a surface view the posteromedial convexity has a sphere-like appearance that levels off inferior-laterally but maintains its height posteriorly and diverges into the medial wall.
This convex area, referred to as the ‘posterior medial bulge’, is the key zone for the vertical position and anterior projection of the globe. It also provides its main support.
The surface landmarks of the orbital floor include the
- Infraorbital groove: a bony sulcus running forward from the middle border of the inferior orbital fissure. Anteriorly it is covered with a thin bone plate as it converts into a canal, which continues to the infraorbital foramen.
- Posterior lateral promontory: medial to the dorsal end of the infraorbital groove the posterior medial bulge ending in a raised promontory shaped lateral plateau. It delineates the junctional zone of the maxillary surface of the orbital floor with the orbital process of the palatine bone. In large orbital floor fractures it represents an important intact bony landmark, the residual posterior bony ledge.
- Origin of the inferior oblique muscle: a small bony depression in the anteromedial orbital floor behind the edge of the orbital rim, just lateral to the anterior lacrimal crest.
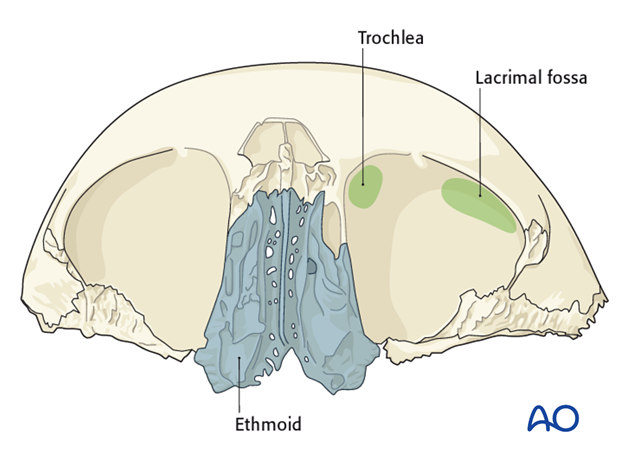
3. Medial wall of the orbit
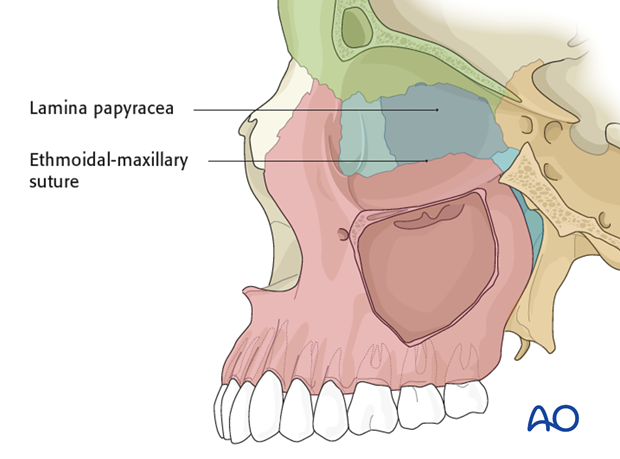
The medial wall has a convex rectangular shape and runs parallel to the sagittal plane. This convexity becomes particularly prominent in the midorbit at the maxillary-ethmoidal suture line, where it transitions into the posterior medial bulge of the maxillary surface of the orbital floor. The medial wall is paper thin (Lamina papyracea) but reinforced along the maxillary-ethmoidal suture forming an internal orbital buttress.
Many fractures of the posterior medial bulge abruptly break off along this line and do not cross over into the lamina papyracea of the medial wall.
The surface landmarks include the
- Lacrimal fossa: located in the anterior one third of the medial wall between the frontal process of the maxilla anteriorly and the lacrimal bone posteriorly. The posterior limb of the medial canthal tendon (Horner’s muscle) inserts on the posterior lacrimal crest. The tendon is a landmark structure of the medial orbit in the pre-/transcaruncular surgical approach.
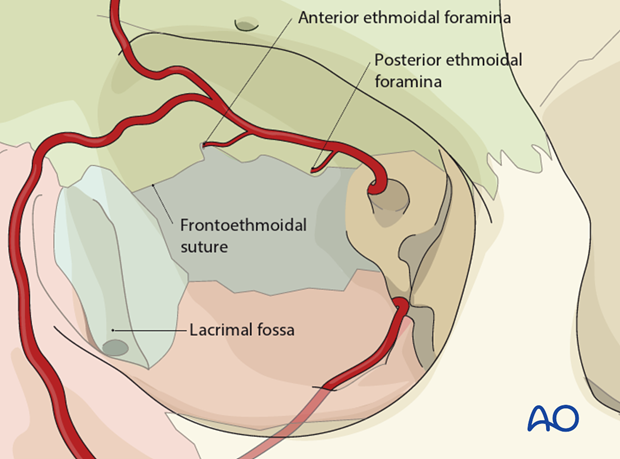
- Frontoethmoidal suture: marks the roof of the ethmoid sinus at the level of the cribriform plate.
- Anterior and posterior ethmoidal foramina: located along the frontoethmoidal suture in the midorbit. They are easily identified intraoperatively. The distance from the anterior lacrimal crest to the anterior ethmoidal foramen is 22-24 mm. The posterior ethmoidal foramen is 12-15 mm posterior to the anterior foramen. The distance between the posterior foramen and the optic canal is usually 3-7 mm along an imaginary continuation of a line through the foramina to the orbital apex.
The ethmoidal foramina as well as the frontoethmoidal suture are critical landmarks:
- Instrumentation beyond the posterior ethmoidal foramen can result in mechanical injury to the optic nerve.
- Bone removal superior to the frontoethmoidal suture will result in communication with the anterior cranial fossa and expose the dura.
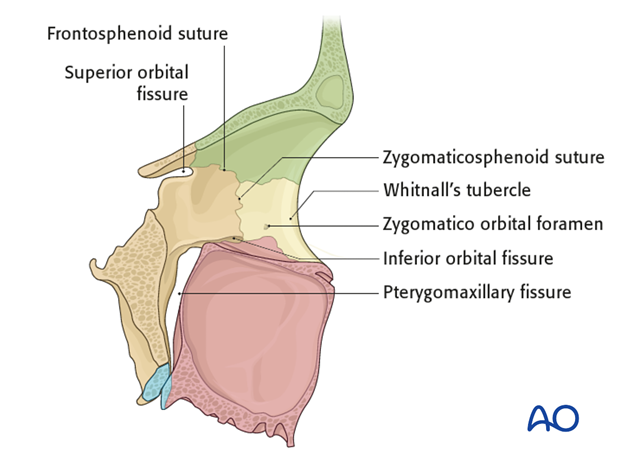
4. Lateral Wall of the orbit
The lateral wall roughly forms a triangle with an anterior base. It is a flat surface bounded by the zygomaticofrontal, frontosphenoid suture and lateral edge of the superior orbital fissure superiorly and the inferior orbital fissure. The lateral orbital wall forms a 45° angle to its medial wall counterpart.
Apart from the superior and inferior orbital fissure the surface landmarks include the
- Whitnall’s tubercle: a small lateral bony tubercle where the lateral retinacular structures attach.
- Zygomatico temporal and zygomaticofacial grooves/foramina: containing the neurovascular bundles of the same name.
- Zygomaticosphenoid suture: this long articulation between the orbital flange of the zygoma and the greater wing of the sphenoid lies in the thinnest portion of the lateral wall and courses into the anterior loop of the inferior orbital fissure. It is an important landmark to verify proper reduction of complex zygoma fractures.
- Frontosphenoid suture: one or more unnamed meningeal foramina are located within this junction and contain recurrent meningeal vessels, which set up anastomoses between the external and internal carotid artery circulation.
5. Roof of the orbit
The superior wall is triangular and has a domed contour in the anterior orbital one third and the midorbit. It is mainly comprised of the horizontal orbital plate of the frontal bone. It can be extremely thin, frequently with dehiscent spots in elderly individuals. In such cases the periorbita can become confluent with the dura.
In the apex the orbital roof terminates into the lesser wing of the sphenoid, where the vertically oriented oval shaped optic foramen forms the orbital opening of the optic canal.
The surface landmarks include the
- Trochlear fovea: zone of attachment for the pulley of the tendon of the superior oblique muscle, located superomedially about 5 mm behind the upper medial rim
- Lacrimal gland fossa: smooth and broad indentation within the anterolateral dome containing the orbital part of the lacrimal gland.
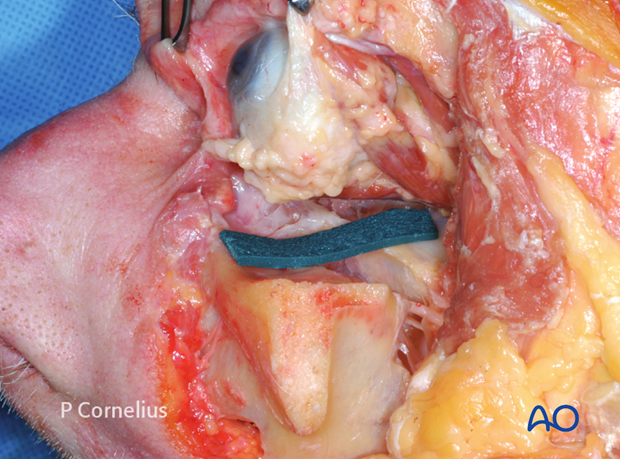
6. Limits of deep periorbital dissection
The posterior third or the apex of the orbit is made up by the sphenoid bone. All neurovascular structures pass through openings in this bone. The superior orbital fissure separates the greater wing of the sphenoid at the lateral side from the lesser wing on the medial side. The optic canal is located medially within the lesser wing of the sphenoid. All the extraocular muscles except for the inferior oblique arise from the annulus of Zinn, a common tendinous ring located at the apex.
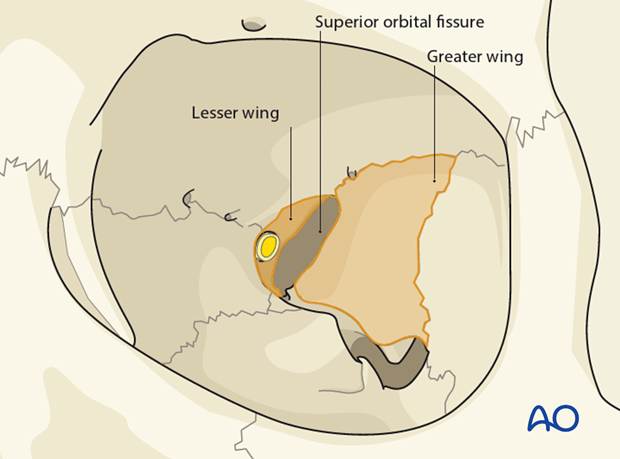
The intraorbital dissection should not proceed into the posterior apex space.
The limit of the inferior dissection is defined by the upper end of the posterior recess of the maxillary sinus that corresponds to the posterior tip of the orbital surface of the maxilla just before the orbital floor joins the orbital process of the palatine bone.
Laterally the boundary for the dissection is the dural reflection at the lateral aspect of the superior orbital fissure.
Superiorly, the orbital roof dissection is stopped at the periorbita surrounding the recurrent meningeal artery, which is identified passing through a bony canal within the sphenofrontal suture line.
Medially, the posterior extent of the deep dissection is marked by the posterior ethmoidal vessels, running in the fronto ethmoidal suture line just anterior to the optic foramen.