Open reduction with or without internal fixation
1. Emergency treatment
Emergency treatment in midfacial fractures may be indicated in the following cases:
- Partial or complete visual loss due to direct or indirect optic nerve trauma
- Severely increased intraocular pressure
- Acute space-occupying lesion (eg, retrobulbar hematoma, emphysema)
- Severe shift of orbital content
- Entrapment of eye muscle (particularly in pediatric patients)
- Severe nasal and/or oral bleeding
Globe rupture and intraocular trauma
There are a variety of possible injuries affecting the globe that may require immediate ophthalmological treatment.
Retrobulbar hematoma
Pressure increase in the periorbital region due to retrobulbar hematoma can cause significant injury of the neurovascular structures with eventual loss of vision.
More details on retrobulbar hemmorage can be found here.
Note: Intraorbital bleeding in patients taking anticoagulation drugs requires special attention.
If a retrobulbar hematoma leads to a tense, proptotic globe, emergency decompression should be considered.
If a retrobulbar hematoma in the cooperative patient results in blindness, the time window to release the intraorbital pressure is limited to around one hour measured from the onset of blindness. This could mean urgent treatment under local anesthesia even in the emergency room prior to further imaging.
Transcutaneous transseptal incisions may help evacuate the hematoma and release the periorbital pressure. Alternative methods such as transconjunctival pressure release and/or lateral canthotomy and inferior cantholysis should be considered according to patient condition.
An exception may be where there is a pulsating exophthalmos which may be a sign of carotid-cavernous sinus fistula. A fistula of this nature requires appropriate preoperative imaging.
Note: retrobulbar hematoma is one of the most severe postoperative complications in patients who have undergone orbital trauma and/or surgery. This is one reason why the surgeon has to assess appropriate vision as soon as possible after injury and/or surgery.
Emphysema
Severe emphysema might significantly raise intraorbital pressure. If this compromises visual function or endangers the orbital contents, orbital decompression has to be considered. Drug protocol may include antibiotics and decongestive nasal drops.
Patients with sinus fractures in the periorbital region should not blow their nose in order to avoid additional emphysema due to acute pressure rise. Should sneezing occur, maintaining an open mouth posture minimizes increasing intranasal/intrasinus pressure.
Usually there is no need for emergency treatment in orbital floor/medial wall fractures unless there is severe ongoing hemorrhage in the orbital cavity, the paranasal, or nasal cavity.
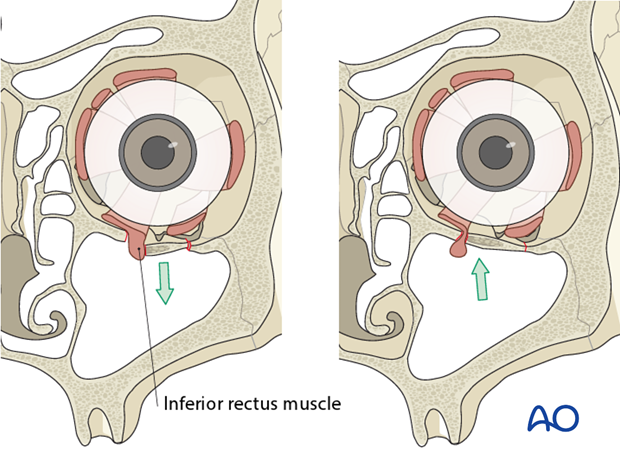
In some younger patients, the so-called trap-door phenomenon can occur in which there is danger of necrosis of the entrapped rectus muscle within a few hours; immediate release of entrapped tissues is necessary.
Entrapment of eye muscle (especially in children)
The inferior rectus muscle is the most common ocular muscle to become entrapped with an orbital floor fracture (trap-door phenomenon) and this may not be visible on conventional x-rays. Entrapment requires urgent freeing of the muscle to prevent necrosis of the incarcerated muscle. Clinical examination should give evidence on impaired ocular muscle function. Entrapment is often associated with severe ocular pain on attempted range of motion, as well as nausea and vomiting, especially in children.
Note: In children, entrapment of the eye muscles is more common than in adults; this might be due to the higher elasticity of the bony structures (green-stick fractures are more common).
Bone fragments affecting the optic nerve
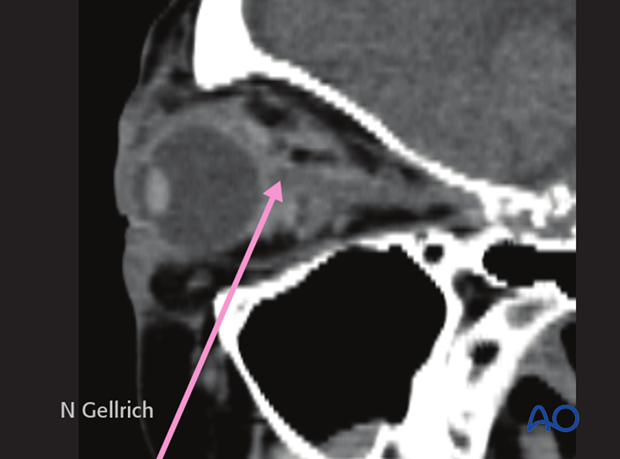
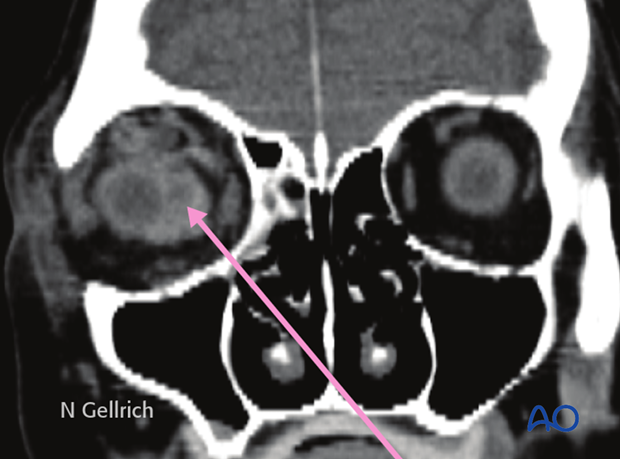
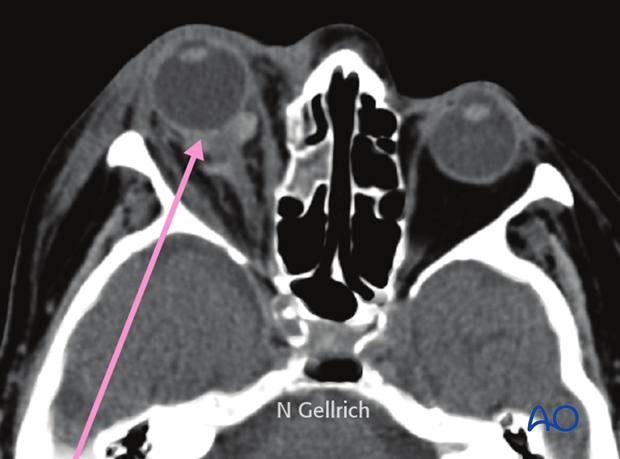
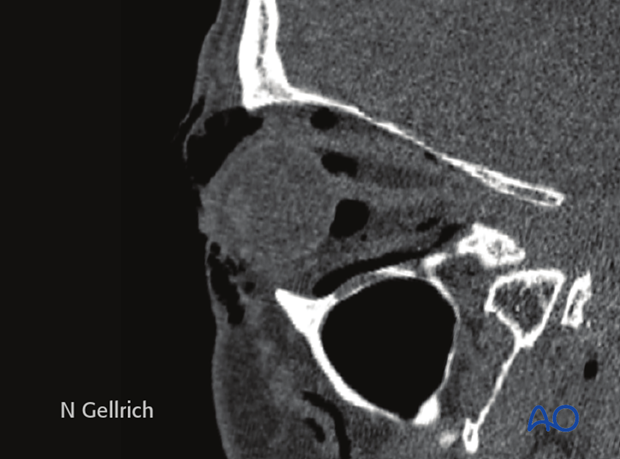
Special attention has to be paid to the posterior third of the orbit and the bony optic canal. Bony dislocations in these anatomical areas are more likely to be associated with traumatic optic nerve lesions.
Axial CT scan in the plane of the optic nerve shows multiple fractures of the lateral orbital wall and the greater wing of the sphenoid of the right side. Additional stretching of the right optic nerve is present. Fractures where fragments involve the posterior third of the orbit are susceptible to subsequent optic nerve disorders.
Severe bleeding
In case of severe bleeding the following options should be considered:
- Assessment of current medical treatment for anticoagulation such as Coumadin, Aspirin, or other anti-platelet medication.
- Compression: either by nasal packing, balloon tamponade, or direct compression.
- Electrocautery: if a clear bleeding source can be evaluated.
- Control and adjustment of blood pressure.
- Interventional embolization when other methods fail.
- In some cases fracture reduction may be required to reduce bleeding.
Note: following the emergency treatment, thorough diagnostic examination may be performed to find the source of bleeding:
- Intranasal inspection
- Angiography with possible superselective interventional embolization.
2. Selection of approach
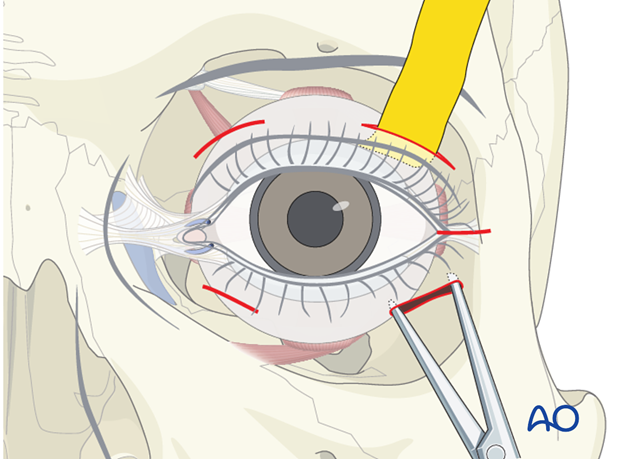
The orbital floor can be reached by various lower eyelid approaches (transcutaneous or transconjunctival). The type of incision has to suit the requirements of fracture reduction and reconstruction, surgeon skill, and individual patient specifics (eg, existing lacerations). Less frequently used is a transoral/transnasal maxillary sinus approach to reach the orbital floor from below. The maxillary approach does not provide visualization of the contour of the orbit.
Care should be taken not to damage the:
- Palpebral anatomical structures
- Lacrimal drainage systems
- Ocular muscles
- Neural structures
The following pages provide general information regarding orbital anatomy and dissection
- Preoperative considerations
- Anatomy of the bony orbit
- Correlation of surface and cross sectional anatomy
- Introduction to periorbital dissection
- Orbital floor dissection
- Medial orbital wall dissection
- Lateral orbital wall dissection
- Orbital roof dissection
- Adjunctive access procedures (orbitotomies)
- Retrobulbar hemorrhage
3. Reduction with or without fixation
Reduction without fixation
In some cases the orbital floor may be reduced and the fracture segment may be stable. Fixation may not be needed. In these cases, the patient should have close clinical follow-up.
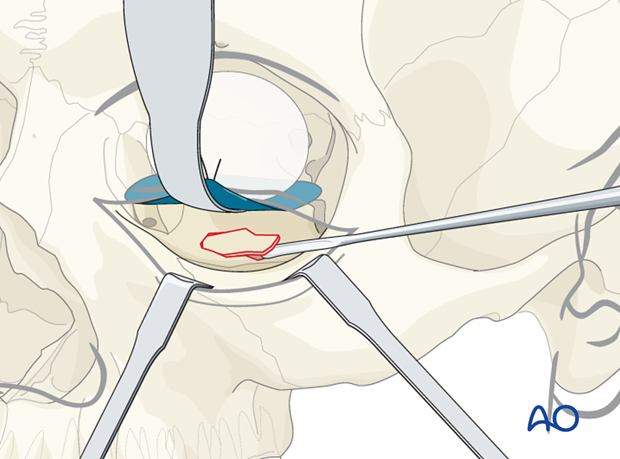
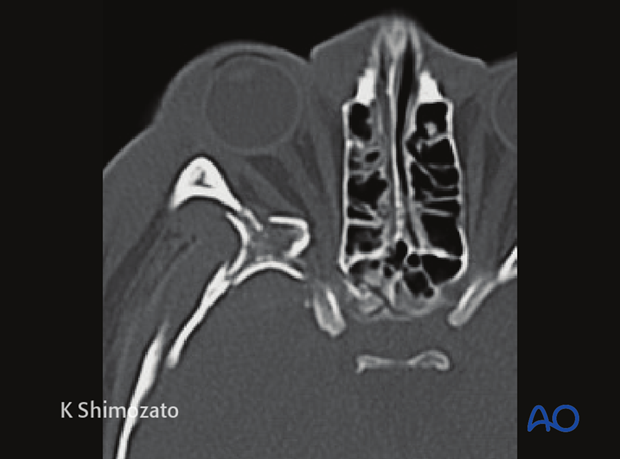
Reduction with fixation
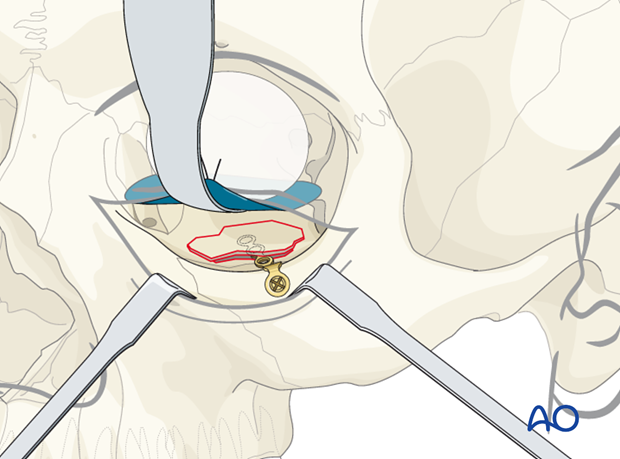
In some cases the orbital floor may be reduced but the fragment is not stable. In such cases a small bone plate can be secured to the stable bone laterally within the orbit and the medial extension is placed underneath the reduced trap door.
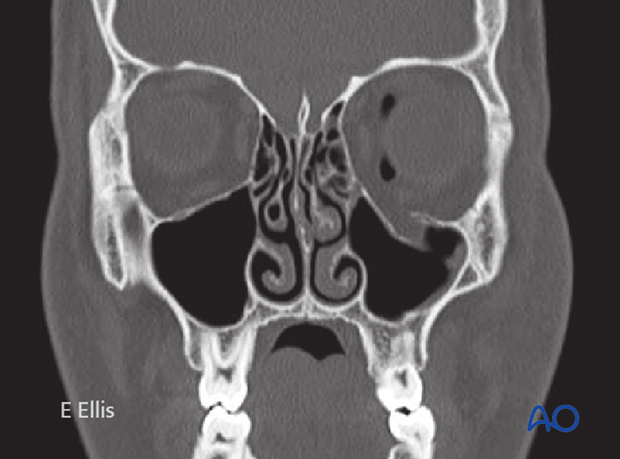
Preoperative CT scan.
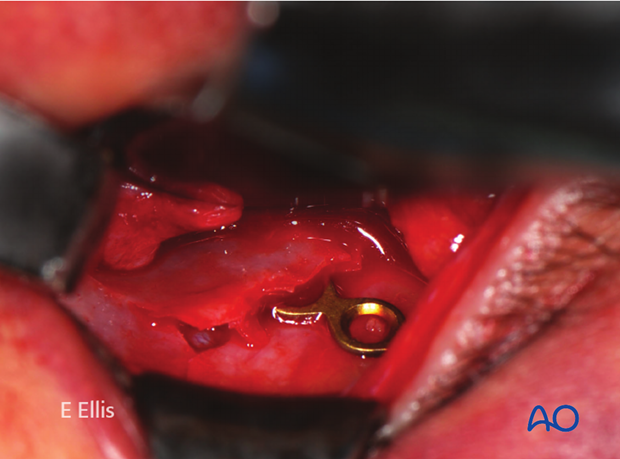
Intraoperative photograph of the same patient.
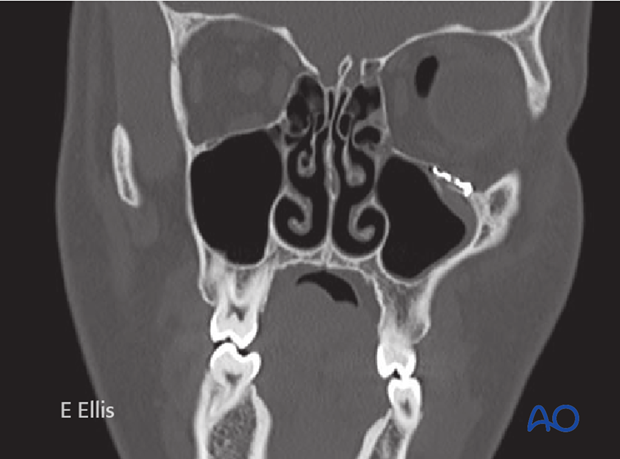
Postoperative CT scan of the same patient.
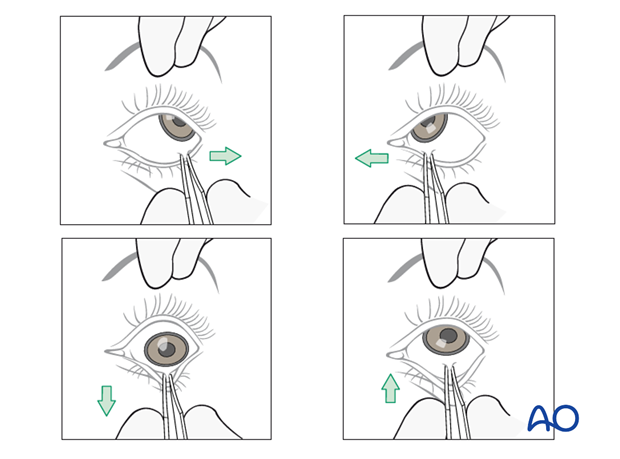
Forced duction test
After the insertion of any implant material, it is imperative to perform a forced duction test. Click here for details.
Note: Pupils should be checked; however pupillary function might be compromised by drugs or mechanical force to the orbital contents.
4. Aftercare following open treatment of orbital fractures
Evaluation of the patients vision is performed as soon as they are awakened from anesthesia and then at regular intervals until they are discharged from the hospital.
A swinging flashlight test may serve in the unconscious and/or noncooperative patient; alternatively electrophysiological examination has to be performed but is dependent on the appropriate equipment (VEP).
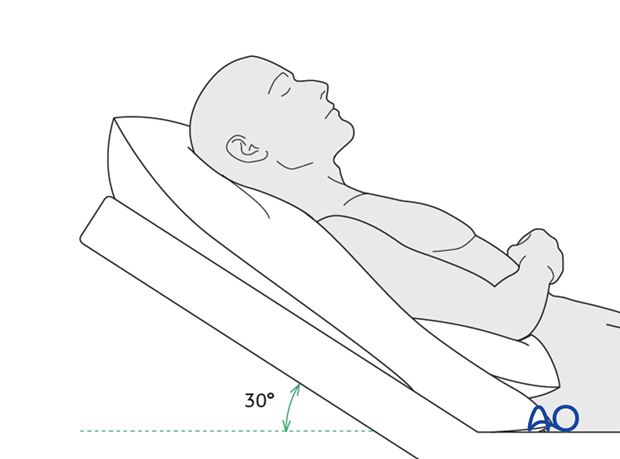
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose-blowing
To prevent orbital emphysema, nose-blowing should be avoided for at least 10 days following orbital fracture repair.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) for 7 days
- Analgesia as necessary
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any one antibiotic, and the recommended duration of treatment is debatable.)
- Nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
- Regular perioral and oral wound care has to include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Note: In case of postoperative double vision, ophthalmological assessment has to clarify the cause. Use of prism foils on existing glasses may be helpful as an early aid.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3-D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from skin after approximately 5 days if nonresorbable sutures have been used.
Apply ice packs (may be effective in a short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Intranasal feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery, and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures and alveolar ridge fractures include:
- Problems of dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), (lack of range of motion, pain)
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Implant removal is rarely required. It is possible that this may be requested by patients if the implant becomes palpable or visible. In some countries it will be more commonly requested. There have been cases where patients have complained of cold sensitivity in areas of plate placement. It is controversial whether this cold sensitivity is a result of the plate, a result of nerve injury from the original trauma, or from nerve injury due to trauma of the surgery. Issues of cold sensitivity generally improve or resolve with time without removal of the hardware.
Generally, orbital implant removal is not necessary except in the event of infection or exposure. Readmission might be indicated if long term stability of the orbital volume has not been maintained.
Follow-up
The patient needs to be examined and reassessed regularly and often. Additionally, ophthalmological, ENT, and neurological/neurosurgical examination may be necessary. If any clinical signs for meningitis or mental disturbances develop, professional help has to be sought. A regular follow-up CT scan is recommended 3-6 months after the trauma to assure proper pneumatization of the sinuses (particularly, mucocele formation has to be ruled out), sealing of the skull base and stability of fragment position.
Note: Posttrauma meningitis can occur even decades following trauma.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed. However, flying in military aircraft should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.












