Examination of patients with midfacial injuries
1. Introduction
Airway and circulation should have the highest priority. This is followed by an assessment of the patient neurological, visual, and cervical spine status.
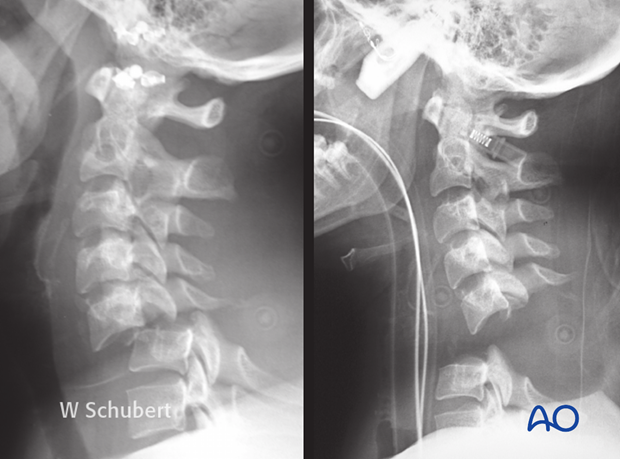
To assess the individual fracture pattern in midfacial fractures the patient medical history should be considered, if possible. This could reveal preexisting occlusal deformities or ophthalmologic pathologies independent of the injury. Often midface fracture patients are admitted to the hospital unconscious and intubated. Special regard has to be given to foreign bodies obstructing the airways such as dislocated partial or full dentures or teeth fragments (see x-ray).
As well as hard-tissue considerations, severe bleeding and/or cerebrospinal fluid (CSF) leakage may accompany and aggravate the treatment outcome.
Basic assessment of visual acuity is mandatory in the conscious patient. In the unconscious patient regular light reflex testing should be performed. The swinging flashlight test should be included to give evidence on optic nerve function (relative afferent pupillary defect (RAPD)).
2. General considerations
To clinically evaluate possible midfacial injuries a standard examination protocol is strongly recommended and has to include full examination of the head, eyes, ears, nose, throat, and neck.
For the experienced surgeon, assessment of midfacial injuries does not take very long.
A standard protocol is presented which may vary according to regional differences and preferences.
The protocol presented here is regarded as fracture or mainly trauma oriented. It does not replace examinations performed by specialists (ie, ophthalmologist, neurosurgeons, etc).
3. Signs and symptoms of midfacial fractures
Possible clinical signs for midfacial fractures include:
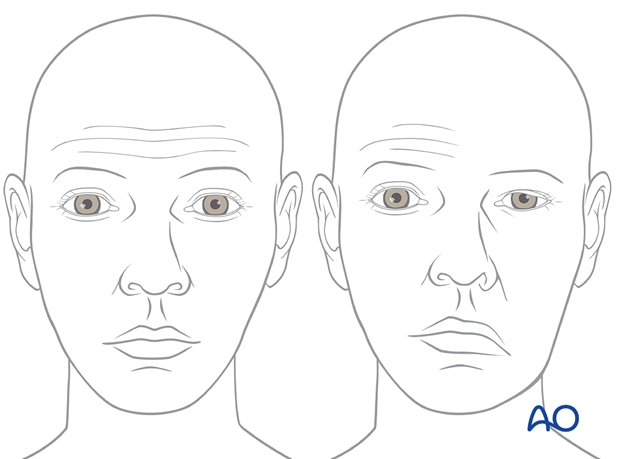
- Facial swelling (edema, hematoma, emphysema) (see picture), and deformity
- Subconjunctival bleeding (hyposphagma) (see picture)
- Oronasal bleeding
- Palpable and crepitating dislocated bony contour in the periorbital region
- Displacement of the globe (hyper-, hypo-, eno-, exophthalmos)
- Displacement of the medial canthal tendon (depending on the degree of NOE fracture)
- Compromised ocular motility
- Double vision
- Sensory deficit (hypoesthesia, anesthesia, paresthesia) of the trigeminal nerve
- Localized pain
- Occlusal disturbance
- CSF leakage (in case of anterior skull base involvement)
4. Instruments for clinical examination
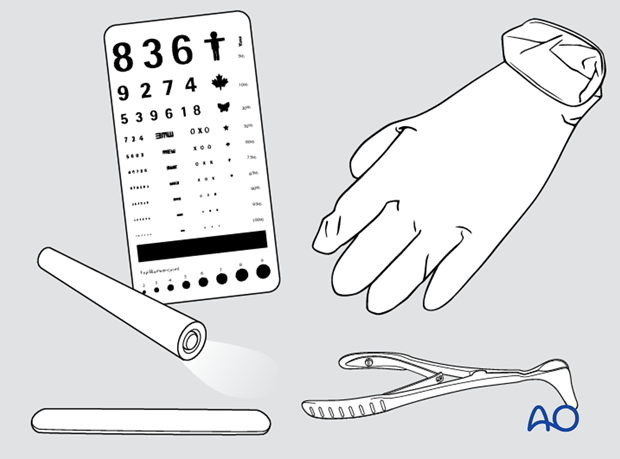
For clinical examination of midfacial fractures, the following instruments are recommended:
- Examination gloves
- Single-use tongue blades
- Examination light
- Visual chart
- Nasal speculum (in case of need for nasal examination)
5. Eye examination
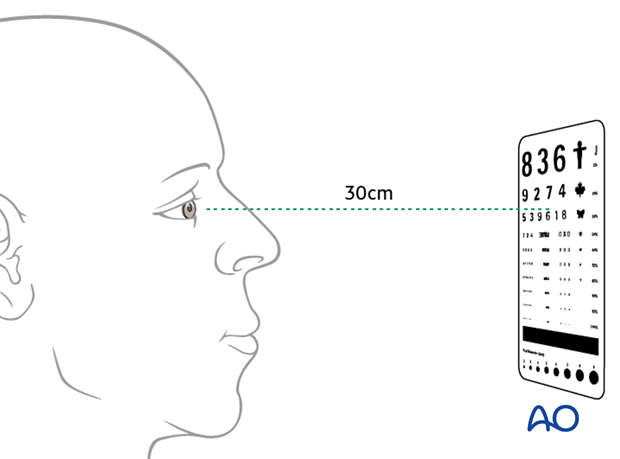
Every patient with orbital fractures should have an examination that includes gross visual acuity testing (remember: preexisting optical correction by glasses or contact lenses or ocular disorders such as cataract, glaucoma, and retinal disorders can compromise basic visual acuity testing), visual field testing, ocular motility, binocular vision, globe position, pupillary reaction, intraocular pressure testing.
Acuity testing
Visual field testing
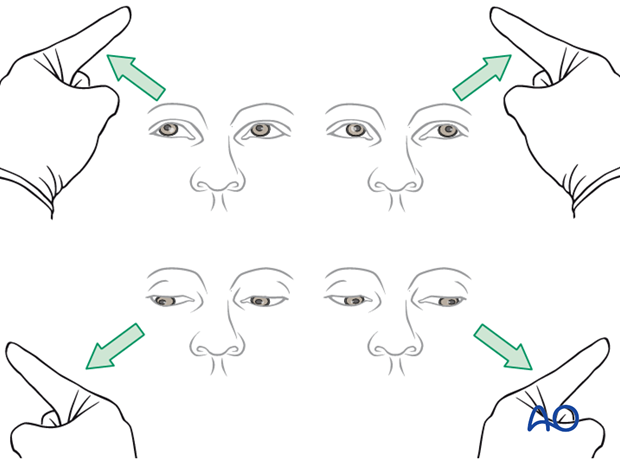
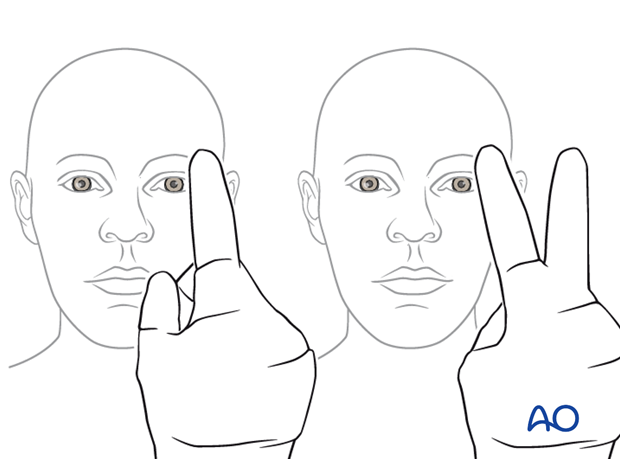
Testing of ocular motility
Examine the patient to check the extraocular muscle (EOM) are functioning properly.
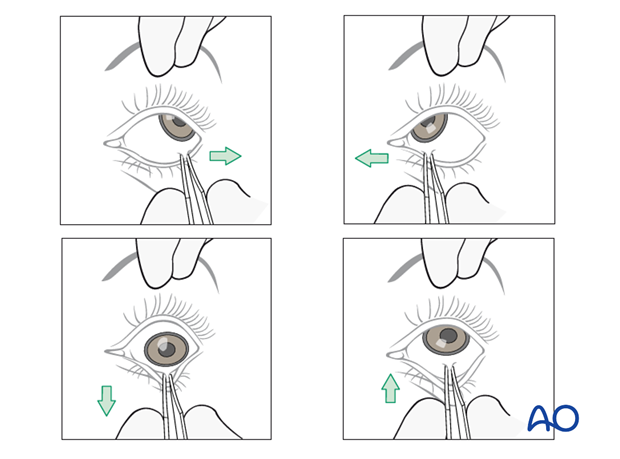
If the extra ocular muscles (EOM) are not functioning properly the surgeon should make sure that there is no entrapment of the soft tissues. It is recommended to perform the forced duction test under sedation, local, or general anesthesia.
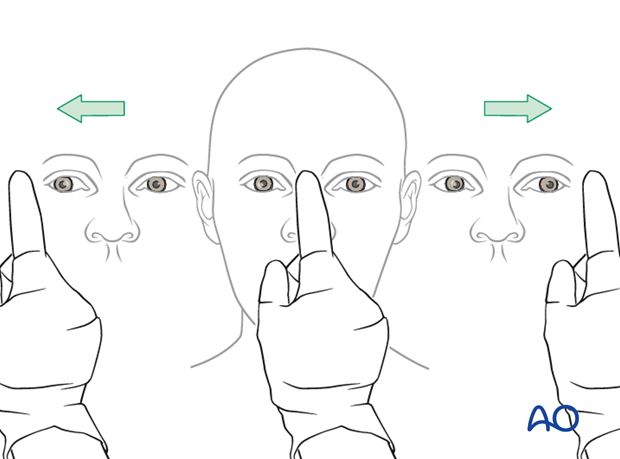
Globe position
Simple testing of pupil axis is provided using a straight instrument. Additional comparison of light reflexes might be useful.
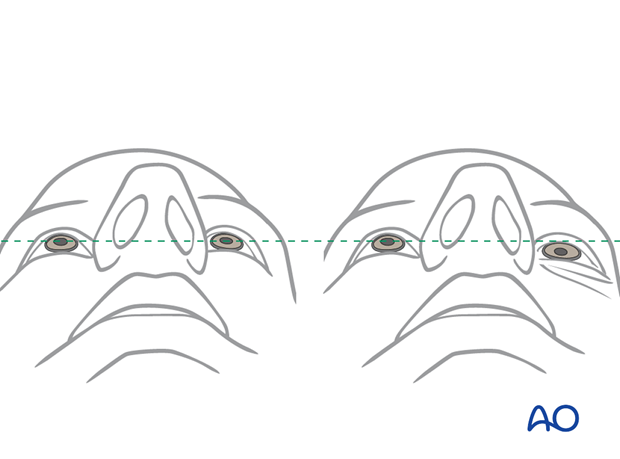
The examiner should include an examination from above …
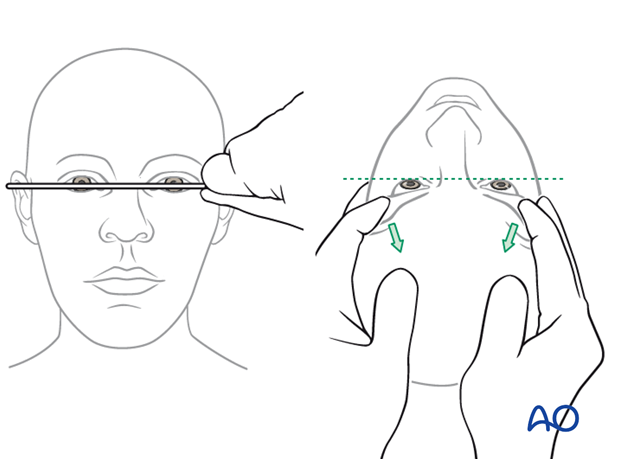
… and below to evaluate facial symmetry.
The illustration on the right shows a posttraumatic asymmetry of globe protrusion (left enophthalmos).
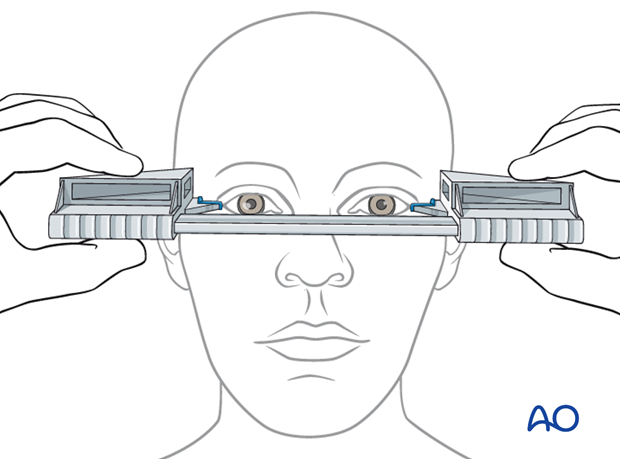
Hertel exophthalmometer
This instrument is only reliable to measure the sagittal globe position correctly in a side-to-side comparison if the lateral orbital rim is intact and not displaced. In these cases, the amount of en- or exophthalmos can reliably be measured.
Note: Evaluation for enophthalmos in the acute setting is unreliable because of orbital edema.
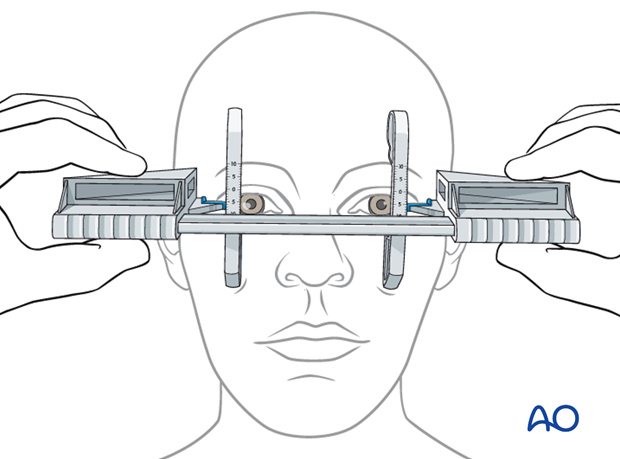
Naugle exophthalmometer
In case of acquired or congential asymmetry of the lateral orbital rims a Hertel exophthalmometer is misleading (see above). In these cases, a Naugle exophthalmometer is preferred since the referring structure is not the lateral orbital rim but the frontal and infraorbital structures.
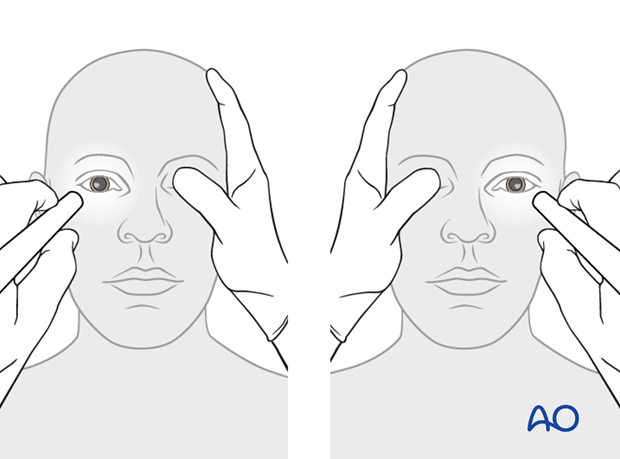
Pupillary reaction
A light is used to assess pupillary reaction.
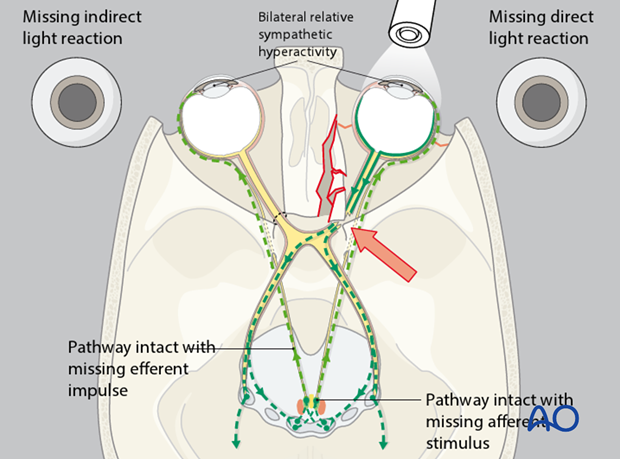
Relative afferent pupillary defect (RAPD)
With a light moving from one pupil to the other, a relative afferent pupillary defect can be detected. In the conscious or unconscious patient who has no drug-related compromise of pupillary function, this test provides a reliable assessment of whether or not an afferent disorder of the visual system is present.
When neither the RAPD nor the pupillary reaction test can be performed, a Visual evoked potential (VEP) may be appropriate.
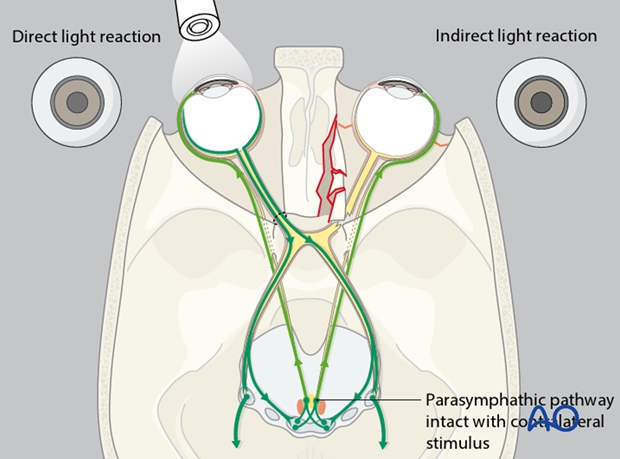
The illustration shows the optic nerve with impingement of the optic nerve at the orbital apex. There is no indirect light reaction of the unaffected right eye (Marcus Gunn pupil).
Note: The indirect light reaction is more reliable than the direct pupillary reaction to detect posttraumatic optic nerve lesions.
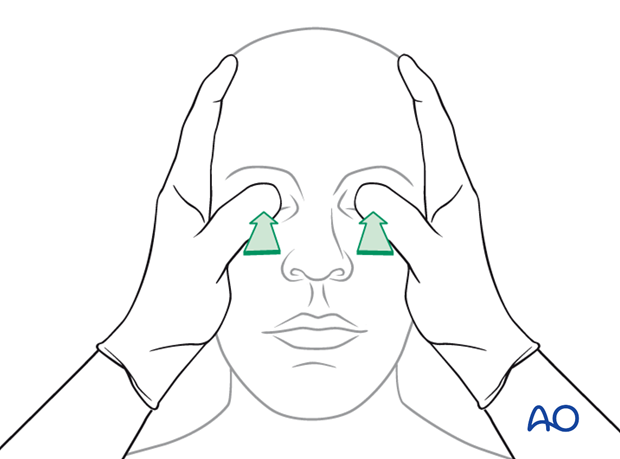
Gross digital intraocular pressure testing
If a patient has sustained significant periorbital trauma, an examination by an ophthalmologist should be performed pre- and postoperatively.
This should include an examination of the anterior chamber to rule out a hyphema. The exam should also include a bright light exam with dilation of the pupil, for a complete examination of the retina. Special consideration should be made to rule out retinal detachment by careful examination of the optic nerve using a bright light examination with a dilated pupil.
Severe exophthalmos due to retrobulbar bleeding may need immediate surgical intervention to decrease the intraorbital pressure. Preoperative radiological examination is mandatory in cases of pulsating exophthalmos which is typical for carotid-cavernous-sinus fistula.
Visual evoked potential (VEP)
Although this technique has been available for decades, it is not yet part of the clinical routine.
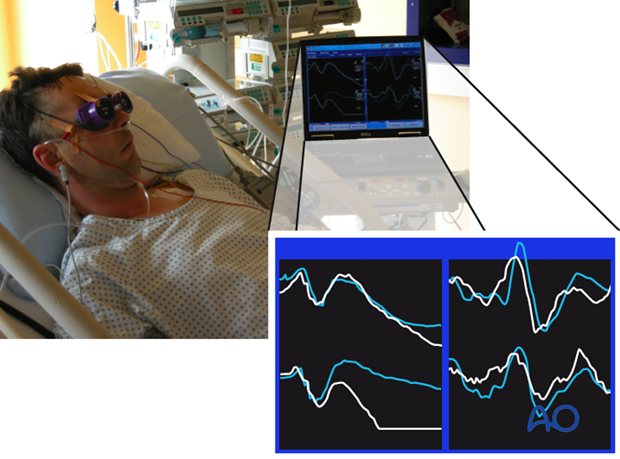
Especially in the unconscious patient where no reliable information on RAPD is available, electrophysiological testing can be performed in the emergency room, on the ward or even intraoperatively if an electrophysiological setup for this testing is available. Basically, an electroretinogram (ERG) together with a VEP has to be recorded for each eye. The ERG is essential to prove that the retina is functioning and generating an appropriate electrical signal which again is transduced via the optic nerve toward the visual cortex (VEP).
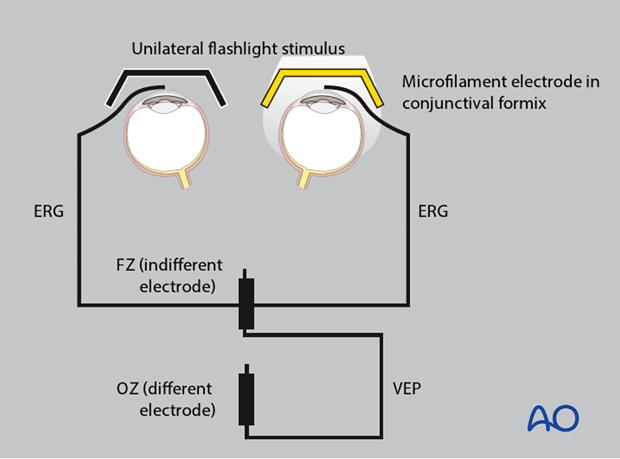
The stimulator consists of goggles or a light source that stimulate exclusively unilaterally one eye. In the author’s experience, the signal is averaged out of 100 singly recorded evoked potentials that are recorded parallel for the retina (ERG) and the cortex (VEP). Each series of recordings takes 100 seconds. For each eye, the recording process has to be repeated to validate the evoked potentials. Later, amplitude and latency of the electrical visual responses can be analyzed. This examination technique requires experience in order not to misinterpret the electrophysiological testing (eg, simultaneous artifacts during electrophysiological testing on an ICU).
However, it has to be emphasized that this testing is a strictly intraindividual testing method reliable in terms of side to side comparison and repeated testing within the same patient.
6. Ear examination
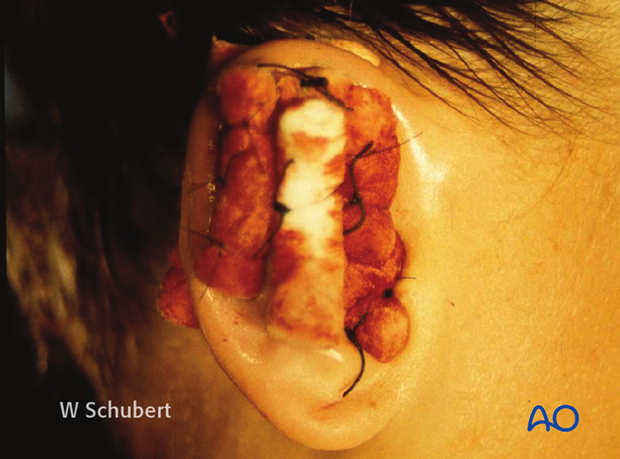
Examine for a hematoma of the auricular cartilage. If there is a hematoma it needs to be drained and a ‘through-and-through’ bolster dressing is recommended. This is to prevent the permanent deformity of a cauliflower ear, with a possible compromise of the external canal.
Note: Make sure the patient can hear with both ears.

Bolster suture are used in a ‘through-and-through’ manner to prevent reaccumulation of the hematoma.
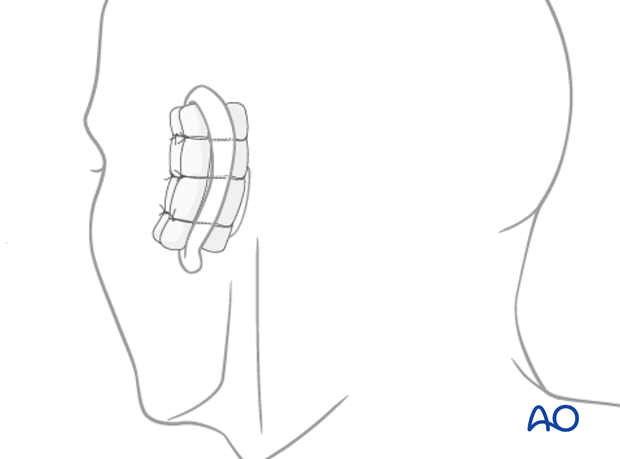
Many different materials can be used as a bolster dressing. In this case, dental rolls have been used.
Examine for blood and/or CSF leakage (which may be seen with a skull base fracture).
Examine for laceration or collapse of the external canal.
Examine the tympanic membrane for rupture or a hemotympanum.
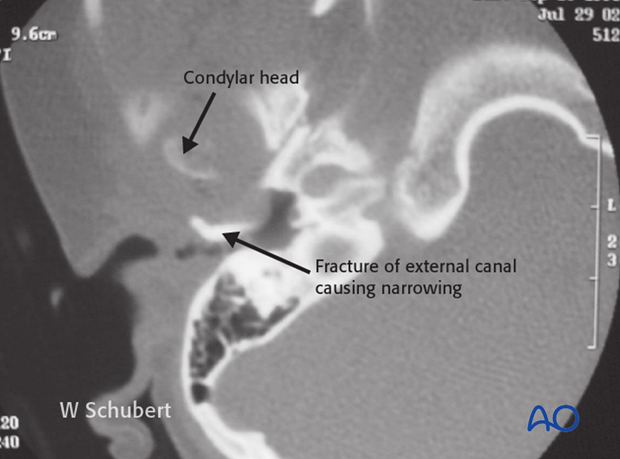
Note: Blood in the ear canal may indicate skull base fractures or external auditory canal lesion resulting from a condylar fracture.

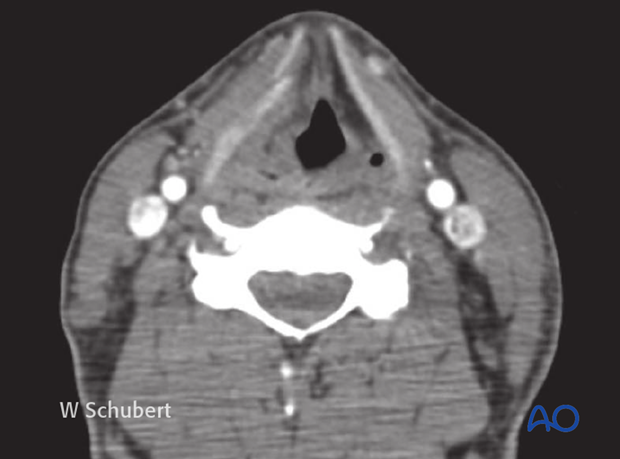
This CT shows a child following impact on her mandibular symphysis, driving the condylar head into the external ear canal. The patient presented with narrowing of the canal and hemotympanum.
7. Nose examination
Examination of the nose starts with inspection for swelling or asymmetry, followed by palpation. Characteristic signs for nasal fractures are:
- Pain
- Bleeding
- Swelling
- Compromised nasal airway
- Crepitation
- Palpable bony dislocation
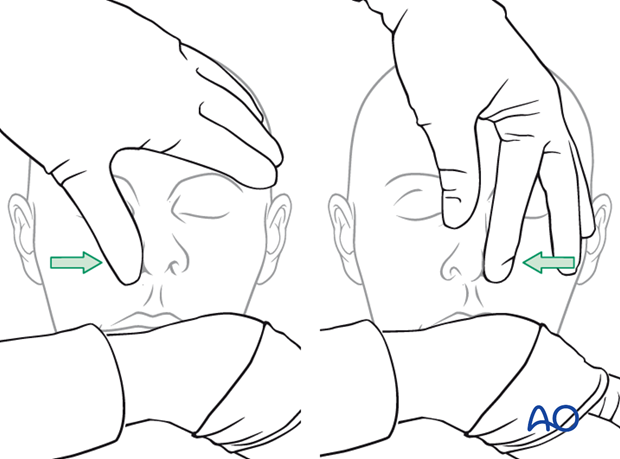
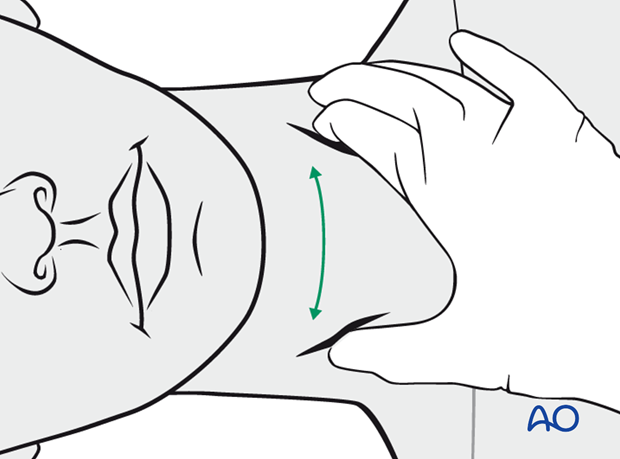
The illustrated testing of the nasal airway passage is a simple method to gather information on the function of the internal patency of the nose.
If the nasal airway passage is compromised the reason has to be investigated.
Note: Remember that obstruction of the nasal airway may also be caused by foreign bodies, preexisting septum deviation, malignancies, etc.
Nasal inspection using a speculum with appropriate light (headlights are recommended) allows for examination of the nasal cavity. If further clinical examination of more posterior or cranial parts have to be performed, additional nasal endoscopy may be indicated.
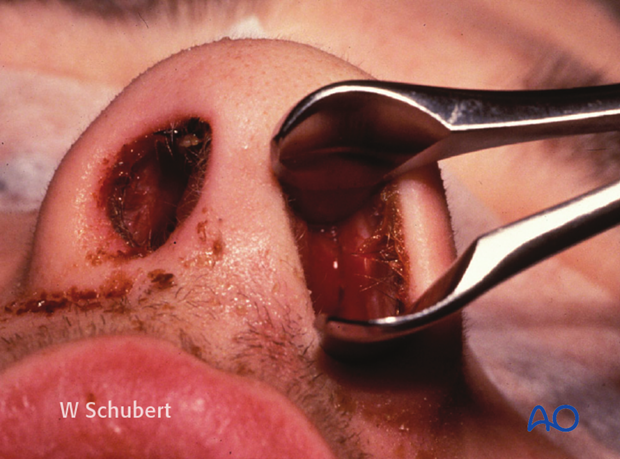
It is very important to rule out a septal hematoma, as this has to be drained to avoid an infection which can result in septal perforation. Nasal packing or splints should be inserted to prevent recurrence of hematoma.

This clinical photograph shows septal hematoma.
Clinical photograph shows delayed drainage of septal hematoma resulting in infection. This patient did not present to the emergency room until 1 week following sustaining nasal trauma.

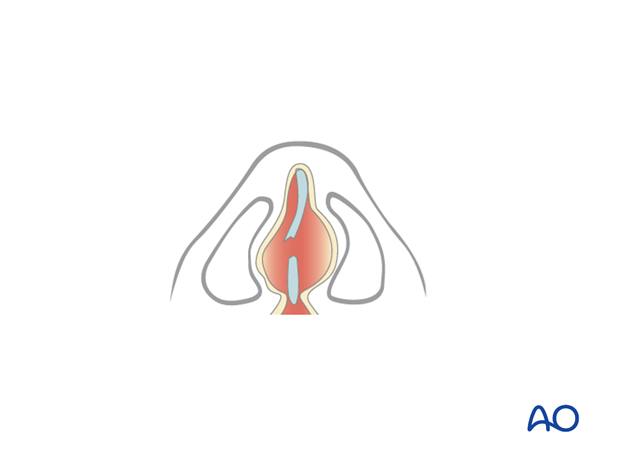
An undetected septal hematoma may also result in the formation of neocartilage, resulting in a widening of the septum and narrowing of the nasal airways.
8. Oral/throat examination
Intraoral inspection
Look for:
- Open fractures
- Asymmetries
- Hematoma
- Lacerations (including salivary ducts)
- Foreign bodies
- Avulsed and luxated teeth
- Malocclusion
- Occlusal irregularities
Intraoral palpation
- Bimanual manipulation of mandibular segments to identify mobile fragments
- Bony steps at the zygomaticomaxillary buttress
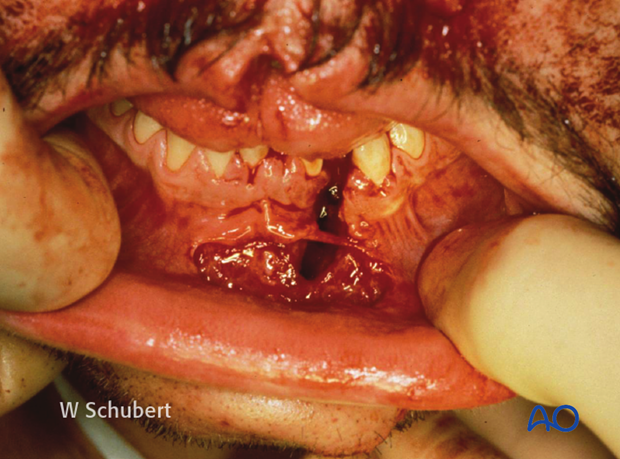
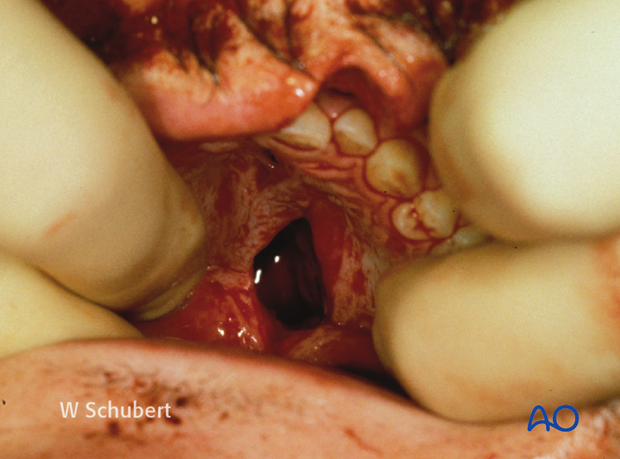
Panfacial fracture showing characteristic anterior open bite deformity which is commonly associated with Le Fort fractures. Multiple dentoalveolar injuries are present.

Note: Palatal hematoma and/or palatal lacerations can be noted in the sagittally split palate.
Clinical photograph shows an additional full-thickness lip laceration.
9. Neck examination
Neck examination
Palpate the posterior neck for any signs of cervical spine trauma.
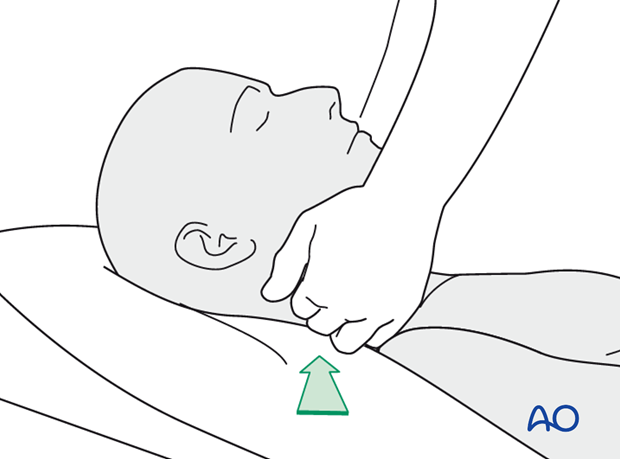
Palpate the anterior neck for signs of laryngeal trauma. A missed laryngeal fracture can result in soft-tissue swelling and a hematoma and consequently in rapid loss of the patient’s airway. Placement of an endotracheal tube may be difficult or dangerous if a patient has a large hematoma. ICU observation of the airway and possible emergency tracheostomy should be considered. Elective intubation for midface surgery should be delayed.
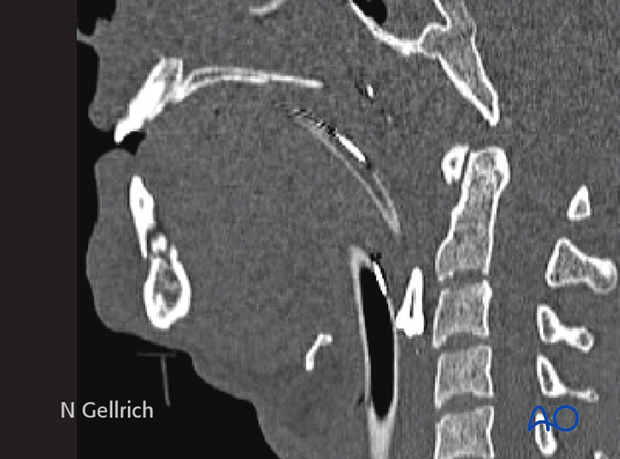
If a laryngeal fracture is suspected, we recommend obtaining a CT of the neck. This CT demonstrates a fracture of the thyroid cartilage.
Examine for any significant penetrating neck trauma or laceration.
10. Sensory exam of the face
Examine the function of the sensory nerves of the face (supraorbital nerve, infraorbital nerve, and mental nerve).
Examine the function of the motor nerves of the face (frontal (temporal), zygomatic, buccal, marginal mandibular, and the cervical branch of the facial nerve). The most important branches to check are the zygomatic and the marginal mandibular.
Illustration shows injury to the zygomatic branches of the facial nerve resulting in inability to close the eye.
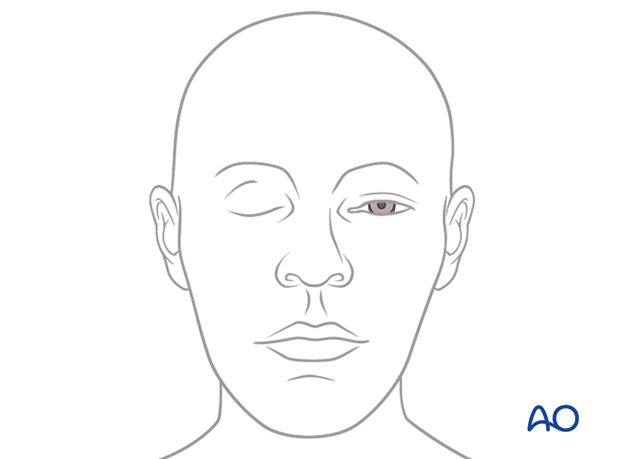
Illustration shows the absence of function of the depressor muscles, resulting in asymmetry of the lower lip.
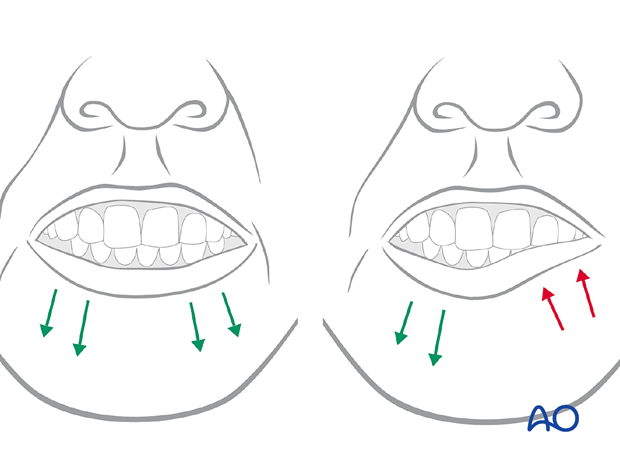
Illustration shows injury to the temporal branch resulting in significant brow ptosis and possible visual field impairment with upward gaze.
11. Fracture palpation
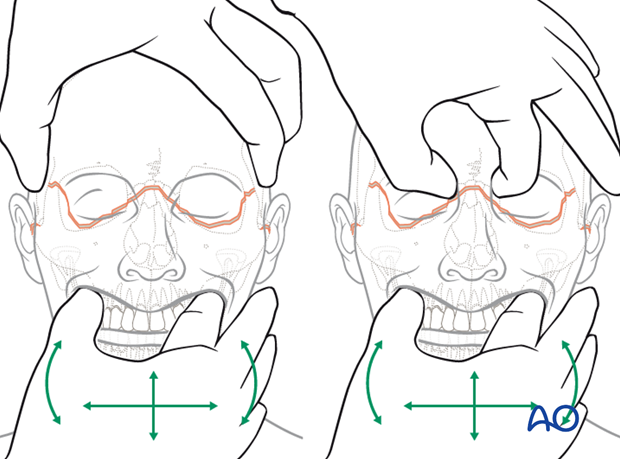
The midface and frontal cranium should be palpated to detect bony irregularities, step-offs, crepitus, and sensory disturbances.
It is crucial for decision making to ensure that one hand stabilizes the skull so that the examiner’s contralateral hand can provide movements which can be assessed.
The illustrations show the step-wise examination of the midfacial skeleton focusing on fracture end movement at the infra- and supraorbital rim.
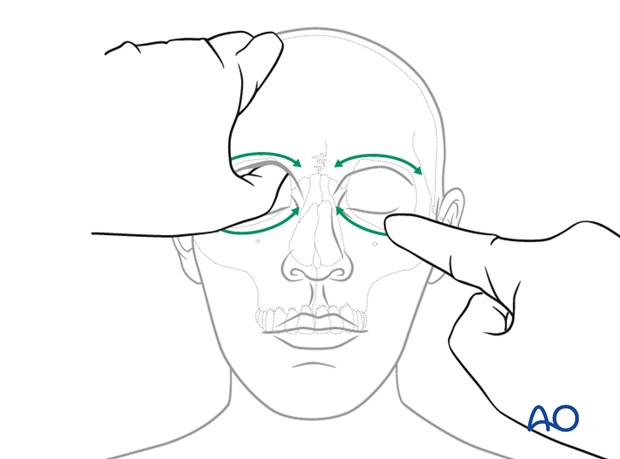
Illustration shows the palpation of the nose.
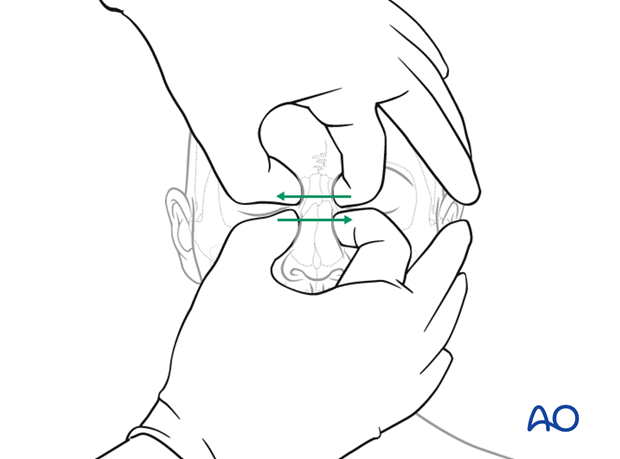
Illustration shows the palpation in the region of the zygomatic complex and zygomatic arch.
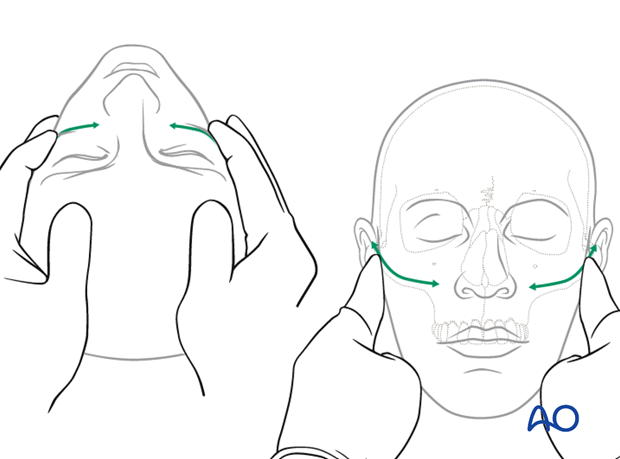
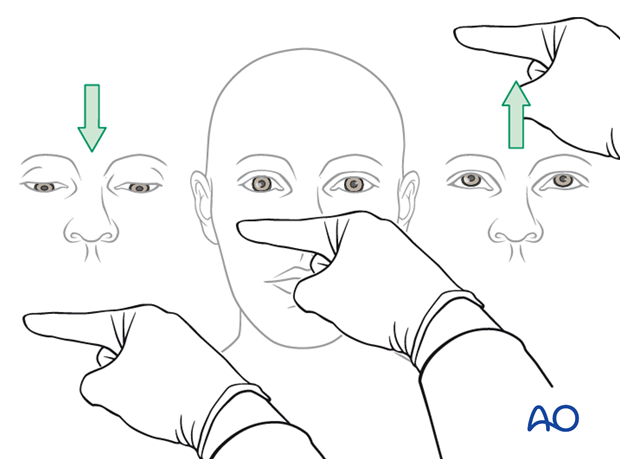
Illustration shows testing for mobility of the maxilla.
Mobility of the midface may be tested by grasping the anterior alveolar arch and pulling forward while stabilizing the patient with the other hand.
The level of a Le Fort fracture (ie, I, II, III) can often be determined by noting the structures of the midface that move in conjunction with the anterior maxilla.
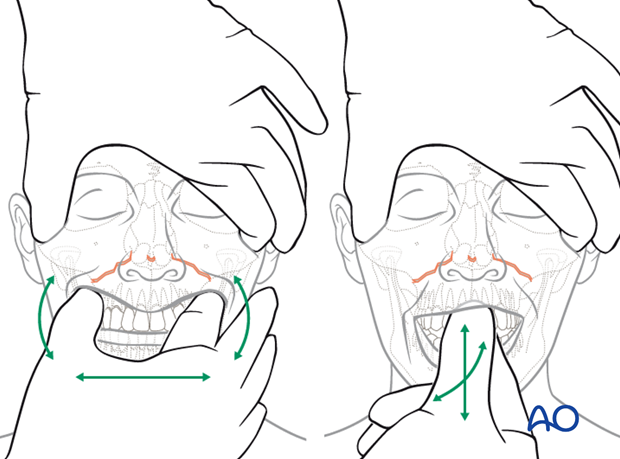
Illustration shows testing for mobility of the central midface.
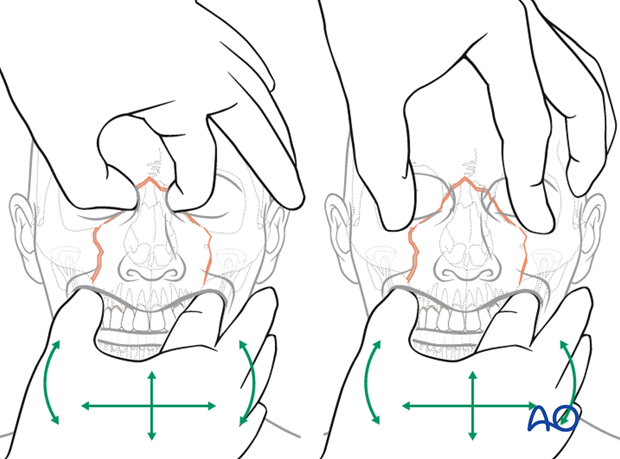
Illustration shows testing for mobility of the midface.
12. Clinical findings: Further reading
For further information see:
Cornelius CP, Altenmüller E, Ehrenfeld M (1996) The use of flash visual evoked potentials in the early diagnosis of suspected optic nerve lesions due to craniofacial trauma. J Craniomaxillofac Surg; 24(1):1-11.
Gellrich NC, Schramm A, Rustemeyer J, et al (2002) Quantification of the neurodegenerative impact on the visual system following sudden retrobulbar expanding lesions - an experimental model. J Craniomaxillofac Surg. 30(4):230-6.
Gellrich NC, Schimming R, Zerfowski M (2002) Quantification of histological changes after calibrated crush of the intraorbital optic nerve in rats. Br J Ophthalmol; 86(2):233-7.
Gellrich NC (1999) [Controversies and current status of therapy of optic nerve damage in craniofacial traumatology and surgery.] Mund Kiefer Gesichtschir; 3(4):176-94. Review. German.
13. Radiological findings
Prior to CT imaging, 2-D x-rays had been considered adequate for pre- and postoperative diagnostics in orbital floor fractures. One of the great weaknesses of 2-D imaging is that in many cases the modality may reveal a fracture, but not the degree of fracture displacement. With the availability of CT imaging, the surgeon can better define fractures, as well the degree of fracture displacement and the need for reduction.
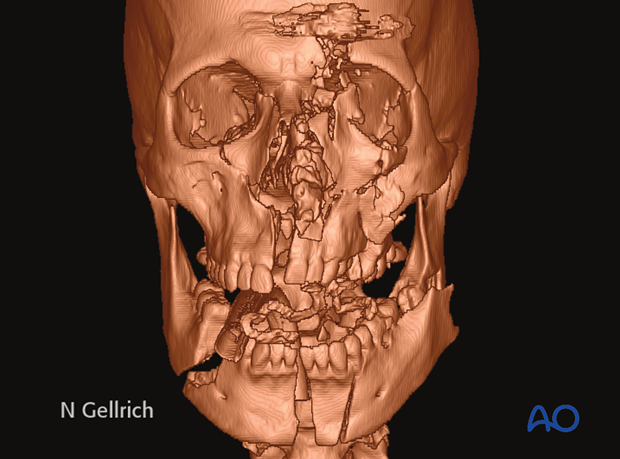
To assess the individual extent and type of fracture, CT or cone-beam based radiological examination should be performed.
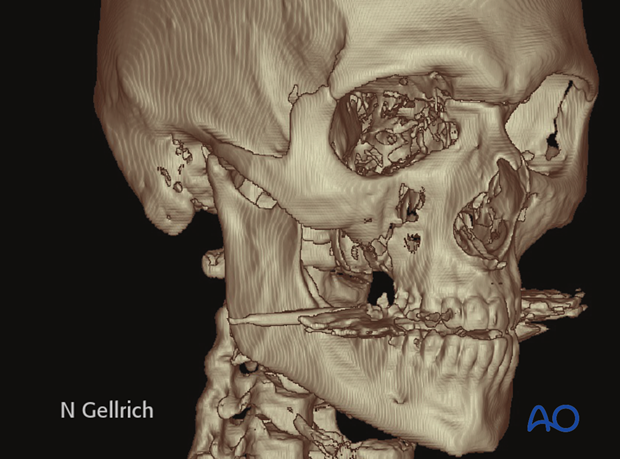
This CT scan shows a panfacial fracture.
CT-scanning
Recommended scanning protocol for CT includes:
- 2-3 mm sliced thickness (orbital fractures: 1 mm)
- Gantry = 0°
- Hard- and soft-tissue window rendering
- Field of view: complete skull (in order to visualize possible accompanying fractures or to scan for possible donor sites in case of bone grafting procedures) including the cervical spine.
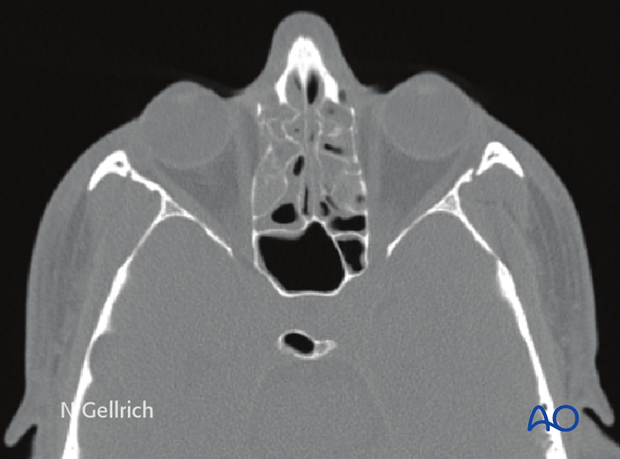
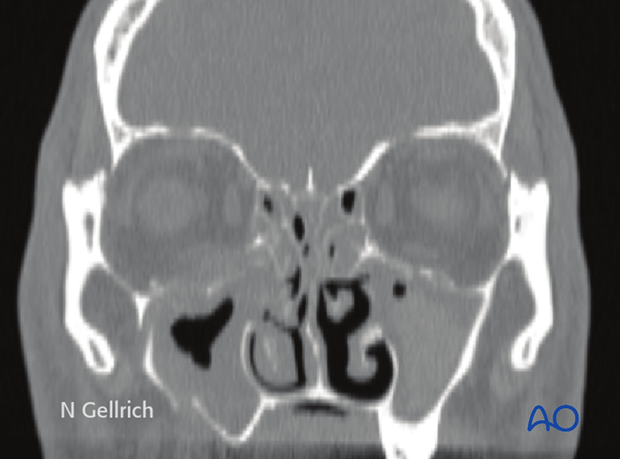
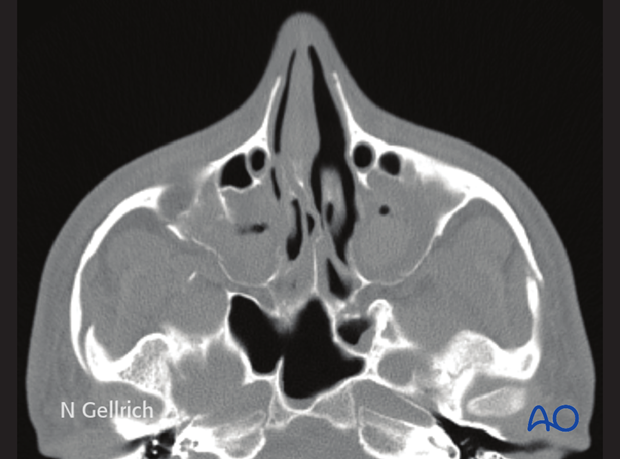
CT scan shows a Le Fort III fracture.
(Metal dental fillings appear as dental artifacts)
Axial CT of the same patient.
Coronal CT of the same patient.
Axial CT of the same patient.
In total body scans in the polytrauma patient, accompanying lesions can be detected.
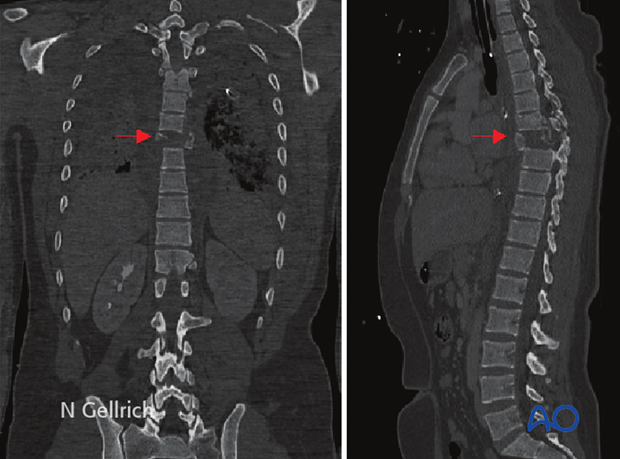
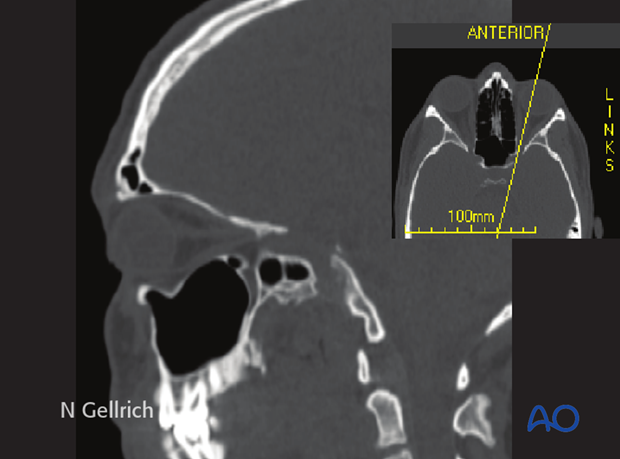
By obtaining CT axial fine slices , the surgeon can obtain excellent reformatted coronal, oblique parasagittal views. The surgeon can also obtain 3-D views.
The x-ray shows the proper plane to obtain an oblique parasagittal view. This plane runs along the axis of the optic nerve. It provides excellent visualization of the orbital roof, the orbital floor, and the course of the optic nerve.
CT evaluation is considered the standard of care for midface fractures.
Cone-beam technology
Cone-beam technology allows adequate determination of the hard tissue problems, but is not equivalent to CT technology in terms of soft-tissue assessment (eg. retrobulbar hematoma). Further limitations of cone-beam technology are given by a more limited scanning region. Cone-beam technology is becoming more important for pre-, intra- (3-D C-arm), and postoperative imaging.
Because there is less exposure to radiation, cone-beam scan may be more suitable for follow-up.
14. Conventional imaging (plain x-rays)
Most centers having CT facilities seldom use 2-D imaging. Some centers find a postoperative AP and lateral view useful to document plate and screw placement.
2-D imaging can include:
- Water’s view (this was a plain x-ray used for visualizing sinus fractures before CT was available. This offers poor visualization of fractures and does not provide the surgeon with adequate information about fracture displacement)
- Orthopantomogram (OPG) this is a standard view normally used for the mandible, but can also provide information regarding midface
- Lateral view (cephalic)
- Submentovertex view (Jug handle view; for zygomatic arch injuries)
2-D imaging particularly lacks precision for the sagittal extent of the injury. Treatment for midfacial fractures based on 2-D imaging risks underestimating the severity of the injury. This might result in later deformities such as enophthalmos or hypophthalmos which could have been avoided by 3-D preoperative radiological examination.
15. Radiological diagnosis of midfacial fractures: special considerations
Special scanning procedures might be necessary if the anterior or lateral skull base is involved and, particularly, for detection or control of CSF-fistula or aneurysms. Special fine slices may be considered for the petrous portion of the temporal bone, particularly in cases where there is paralysis of the facial nerve.
In the event of accompanying dental trauma with missing tooth parts or empty alveolar sockets, it is important to determine the location of the missing elements. For dislocations of teeth into the jaws, standard orthopantomogram (OPG) is helpful. If the missing tooth or tooth parts cannot be localized, additional radiographs of the upper and lower airways (including frontal and/or lateral cervical x-ray, frontal and/or lateral chest x-ray) and/or upper and lower gastrointestinal pathway should be considered. Additional endoscopic measures may be considered in retrieving dislocated dental fragments.
16. MRI
MRI might be indicated to better detect soft-tissue problems such as:
- Optic nerve edema or hematoma
- Ocular muscle disorders (incarceration, hematoma, disruption)
- Intraocular disorders (hematoma)
- Foreign bodies in the orbit
In rare indications ultrasound may be indicated to detect intraoccular or intraorbital disorders eg, hematoma.













