ORIF, load bearing plate with or without simplification
1. Principles
General considerations
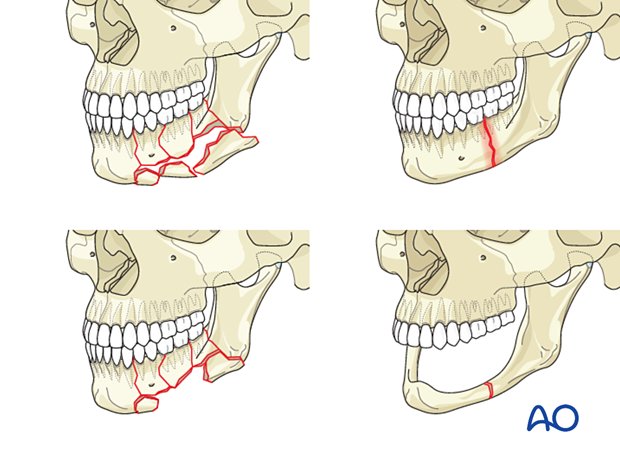
Load-bearing fixation is indicated for open surgical treatment in all types of complex fractures in the mandibular body (comminuted, chronically infected simple fractures, segmental defects, and fractures of the edentulous atrophic mandible).
Edentulous atrophic fractures and infected fractures
Further information on treating edentulous atrophic fractures and infected fractures with or without bone loss can be found in the respective hyperlinks.
If a reconstruction plate is used because of a history of chronic infection, the mandible's infected area should be spanned without using screws close to the area of infection within that area. At least three screws in the uninvolved bone on each side of the fracture are required.
Bone defects
Bone defects may be managed primarily or secondarily. If there is good soft tissue available for tension-free closure over the bone graft, osseous defects may be primarily bone-grafted. Otherwise, secondary bone grafting reconstruction is advisable.
If a secondary reconstruction is planned, the use of a temporary external fixator may be considered.
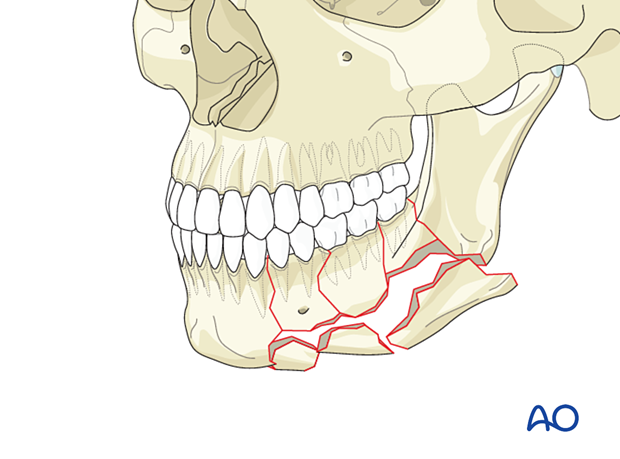
Comminuted fractures (the main focus of this procedure)
Although there is a risk of subsequent infection, sequestration, or bone loss, primary ORIF is the treatment of choice for comminuted fractures.
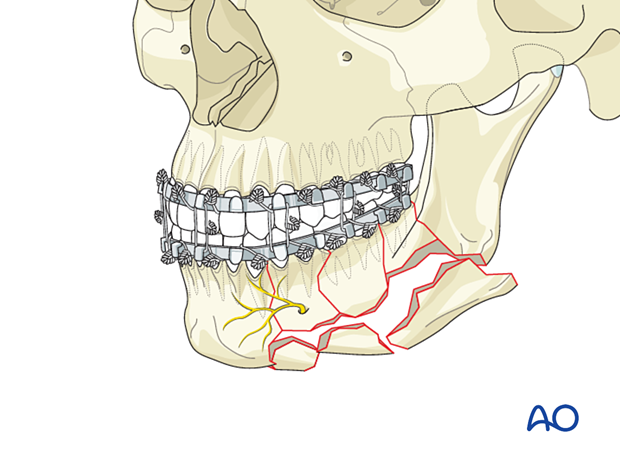
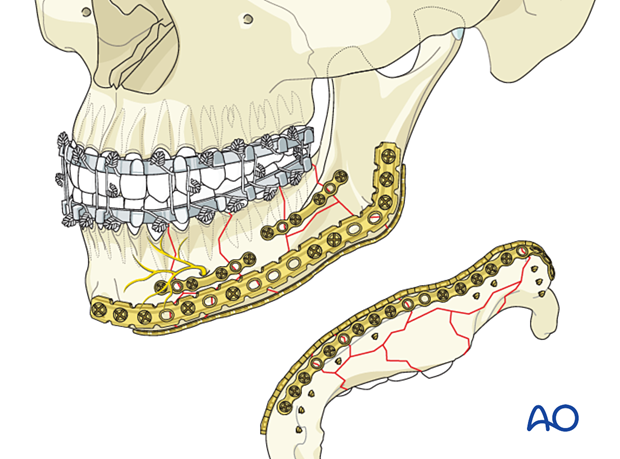
The load-bearing fixation bridges the area of comminution. The bone fragments within the comminuted area will usually not provide support to the construct. The reconstruction plate should be fixed with at least three, preferably four screws on each side of the comminuted area.
To illustrate the principles, the remainder of this procedure will focus on the comminuted fractures.
Keys to success
The keys to a successful result are:
- Fracture simplification with adequate three-dimensional fragment reduction and fixation
- Proper alignment of the alveolar segments to restore preoperative occlusion
- Application of a well-adapted reconstruction plate, bridging unstable segments
Other considerations
Following special considerations may need to be taken into account:
Click on any subject for further detail.
2. Fixation of comminuted fractures
Stepwise repair: simplification before load-bearing reconstruction
When treating comminuted mandibular body fractures, the surgeon should proceed in a stepwise fashion:
- Place the patient in occlusion and secure MMF
- Simplify comminuted fractures using miniplates
- Perform the load-bearing fixation
When simplification is performed, small fragments within a comminuted area are reduced and fixed to each other to build up larger bone fragments that will fit into the gap. These compound bone fragments are used to realign the overall bone shape (anatomic reduction) and help to contour the reconstruction plate along the reduced lower mandibular border.
The use of one long plate spanning the entire superior segment would provide more stability than several smaller plates.
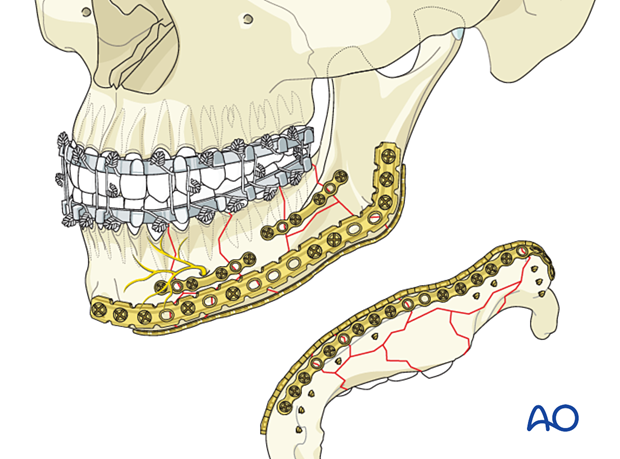
Plate selection for the load-bearing fixation
A thick locking reconstruction plate with an adequate length (at least three holes on either side of the fracture zone are required) is the implant of choice
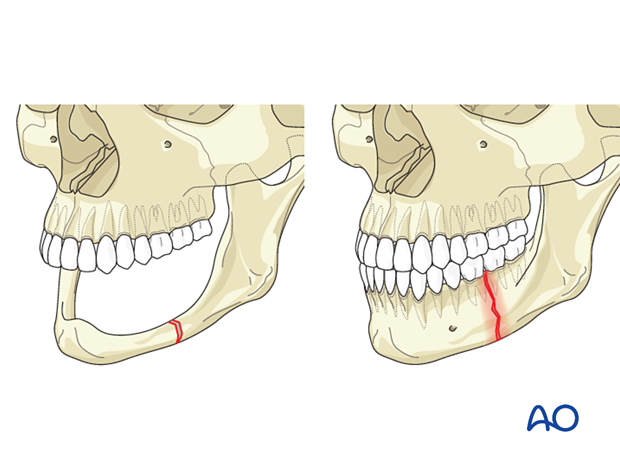
Zones for screw placement in the mandibular body
Two structures must not be harmed by screw insertion:
- the mandibular canal with the inferior alveolar nerve
- the tooth roots.
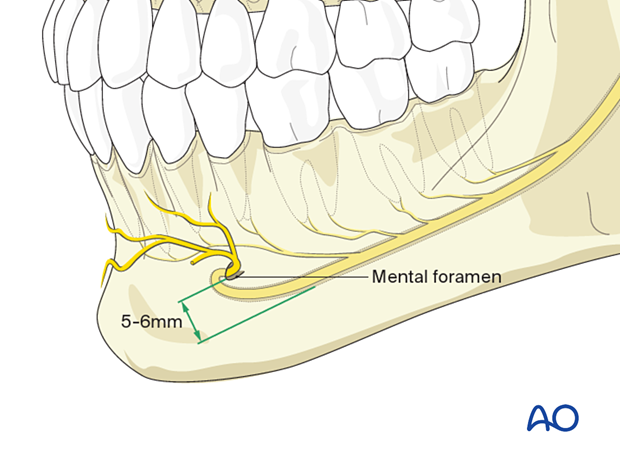
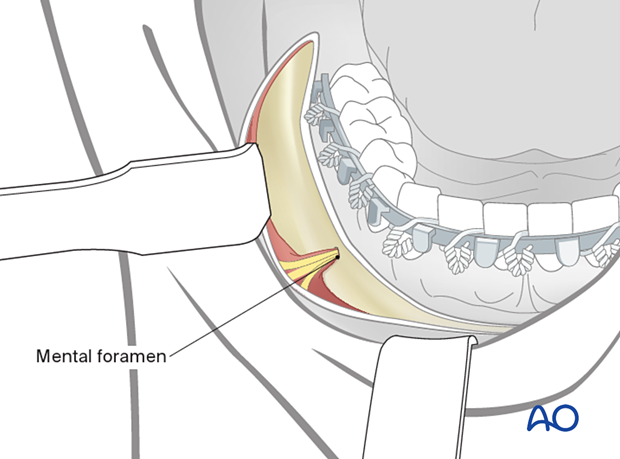
The classical description for screw placement in plate and screw osteosynthesis is depicted for orientation. Monocortical screws can be inserted above the level of the mandibular canal. The use of bicortical screws is restricted to the area below the nerve canal at the lower mandibular border.
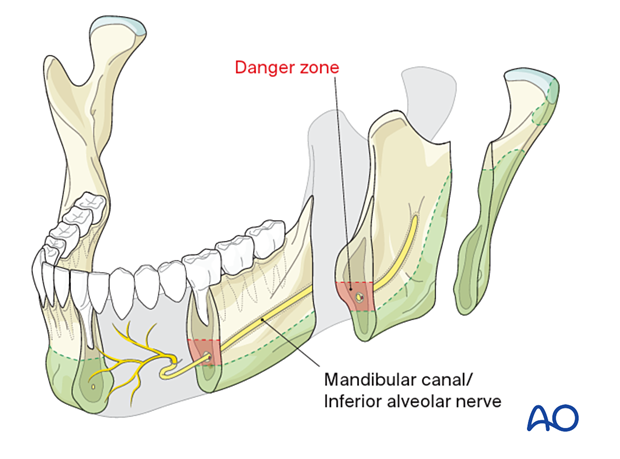
Bicortical screws should be inserted more than 5-6 mm caudal to the mental foramen because of the inferior alveolar nerve path in this area.
AO Teaching video
In this AO Teaching video, the application of a reconstruction plate is demonstrated.
3. Patient preparation
This procedure is typically performed with the patient placed in a supine position.
4. Surgical approach
The transoral approach is utilized for the superior plate. Inferior plate fixation may require a trochar for transcutaneous screw insertion or transoral screw insertion using an angled screwdriver.
Alternatively, a submandibular approach or existing lacerations may be used.
The submandibular approach will be favorable for posterior and complex fracture patterns.
If the submandibular approach is utilized, the risk of mental nerve injury is low since the nerve is reflected out of the surgical field due to the upward soft-tissue retraction. However, there is a risk of injury to the facial nerve's marginal branch.
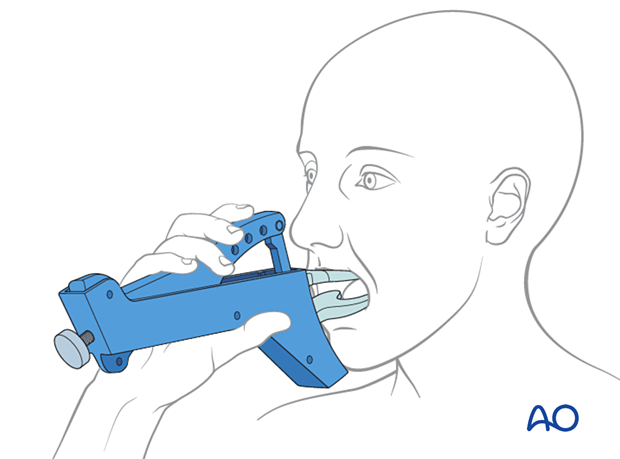
5. MMF
The fracture is exposed, and any tooth extraction deemed necessary is performed. The bony fragments should also be reduced before placing the dentate patient into occlusion and securing the MMF.
In the isolated mandible body fracture, an arch bar is preferred for MMF as it may be left in place during the fracture healing. It will then provide additional support during function.
MMF bone screws are mostly used to provide temporary fixation during surgery and do not postoperatively.
Another consideration would be the use of hybrid (bone-anchored) arch bars that offer rigidity to the alveolar segments.
Click here for further details on methods for applying MMF.
6. Simplification
Realignment and fixation of fragments at the superior border
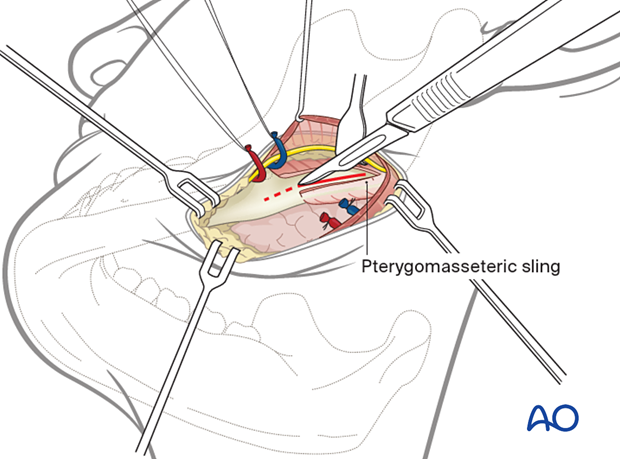
The superior border (alveolar process) fragments are reduced to create one "large fragment." This is also referred to as simplification of the comminuted fragments. The reduction is performed manually or with the use of elevators or bone hooks.
One or several miniplates are cut, contoured, and applied to secure the simplified fragment to the non-fractured mandibular proximal and distal mandible using monocortical screws.
One long plate can be used to span and hold all alveolar process fragments at once but can be more complicated to apply than several short plates. The use of small plates allows for fine-tuning each fragment's reduction before inserting the load-bearing (basal) plate.
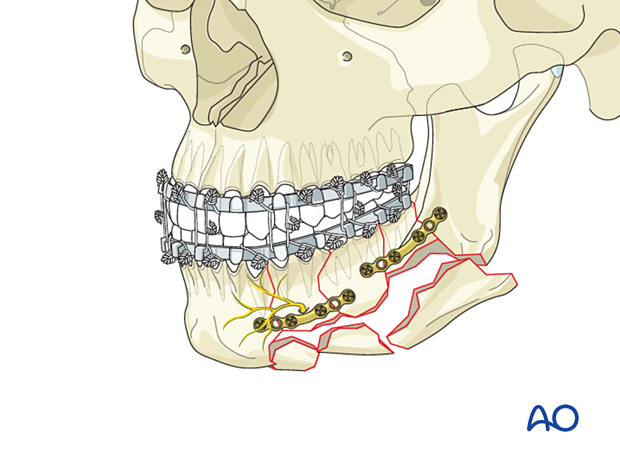
Realignment and fixation of fragments at the inferior border
After a framework has been created at the superior border, the simplification process is continued for the inferior border fragments.
Reduction of the fragments is performed manually or with elevators, bone clamps, or bone hooks.
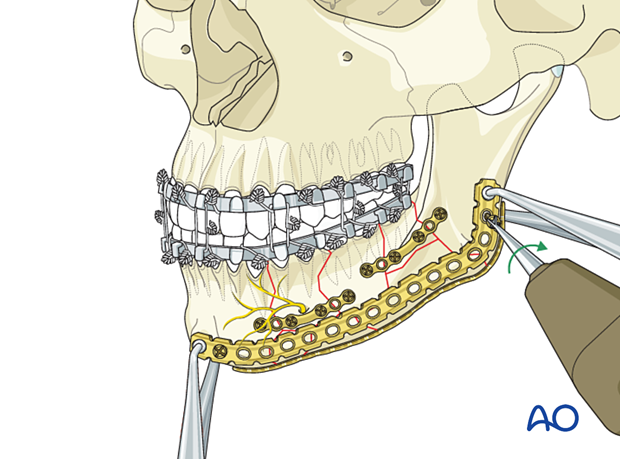
This illustration shows a simplification plate that has been placed on the inferior mandibular border to stabilize the lower fragments. Short screws should be used to not interfere with the bicortical screws used for the reconstruction plate inserted in the next step.
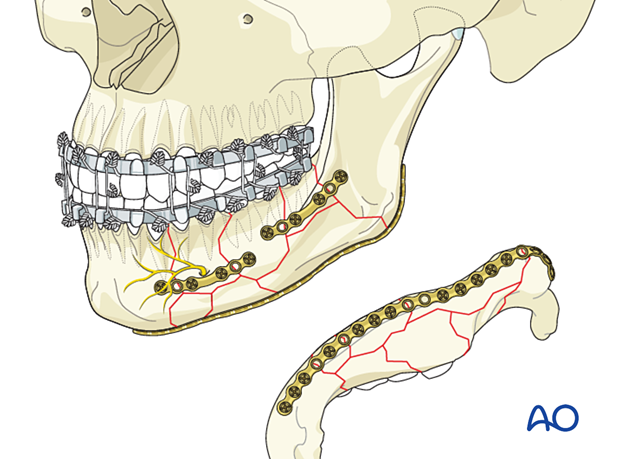
7. Application of the lower border reconstruction plate
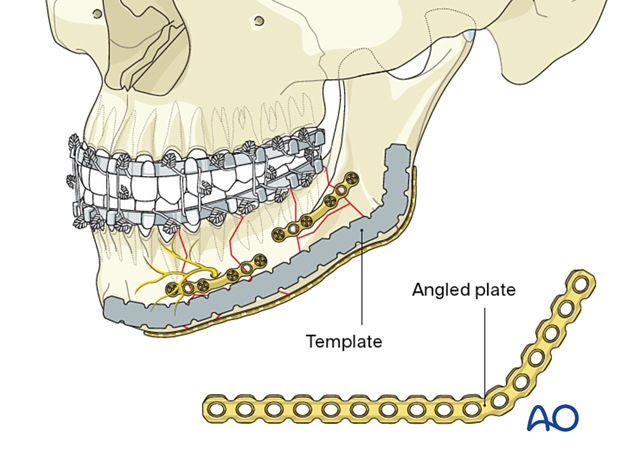
Plate contouring
A straight plate can be used if the comminution zone is confined to the anterior and midbody region. If the comminution zone extends towards the angle, a pre-contoured angled plate is advantageous.
The use of a malleable template is strongly advocated for accurate plate contouring.
Correct plate contour and adaptation is checked visually. To ensure screw purchase for all screws, ensure that the plate is located on the bone over its full length. Screw fixation of the realigned fragments along the inferior mandibular border should be performed.
Preformed reconstruction plates are commercially available.
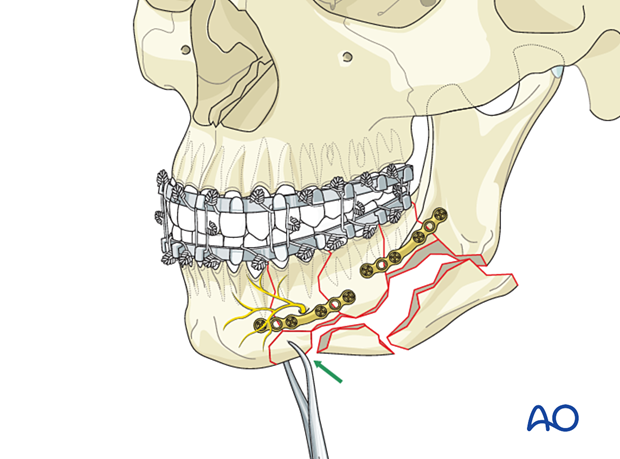
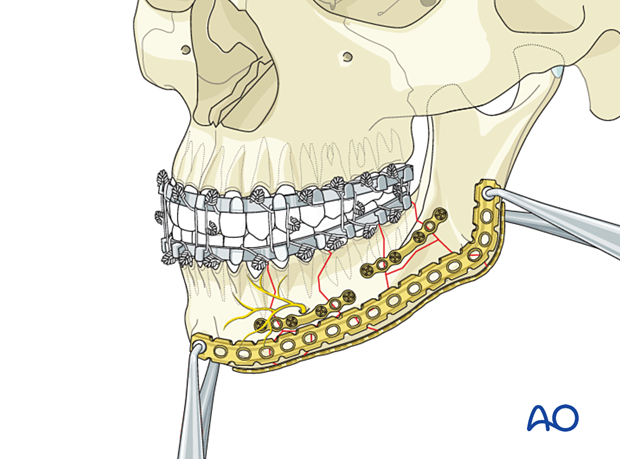
Temporary fixation of the reconstruction plate by holding forceps
Temporarily fix the plate to the intact bone portions using the plate holding forceps.
Insertion of the first screw
The first screw can be placed in any plate hole over either the anterior or posterior bone portion.
Insert the threaded drill guide into the plate and drill a bicortical hole. Use a depth gauge to determine the appropriate screw length.
A crucial point is choosing the appropriate screw length so that the far tip of the screw fully engages the far cortex, with the screw tip exiting slightly beyond the bone's lingual cortex.
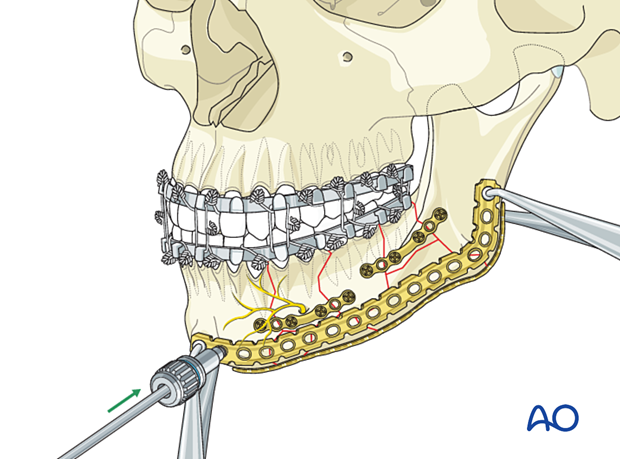
Insert a bicortical locking screw.
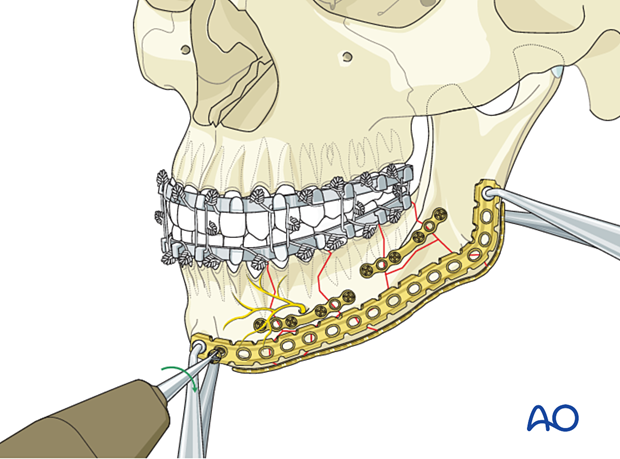
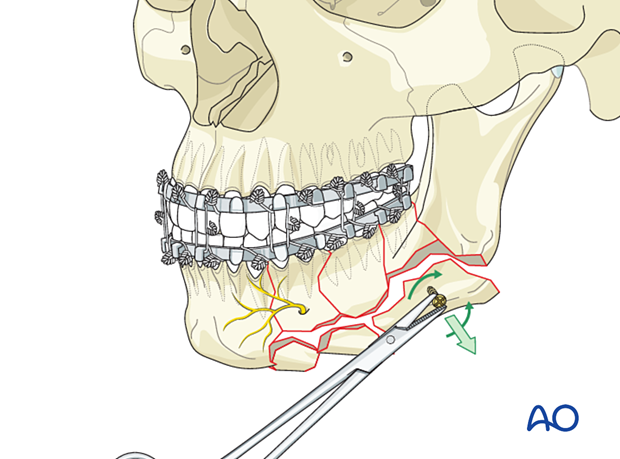
Insert the second screw
The second locking screw is inserted into a plate hole over the opposite intact bone portion.
Additional screw placement
Fill the remaining plate holes over the intact bone portions with locking screws.
Finally, the basal fragments are secured centrally with additional locking screws. Ideally, at least two bicortical screws should be inserted into each significant fragment.
Although locking screws are preferred to prevent secondary fragment displacement, angular screw insertion using conventional screws may be needed to secure a major fragment.
The inferior border simplification plate may be left in place if deemed advantageous.
Final check
Release the MMF and check the occlusion before proceeding with closure.
Wound closure
Intraoral wound closureThe intraoral wound closure has to take into account mucosal lacerations and tooth and bone loss. Appropriate flaps and mucoperiosteal undermining have to be chosen to achieve water-tight and tension-free wound closure.
Extraoral wound closure is performed in multiple layers.
The use of a suction drain may be considered.
8. Case example I
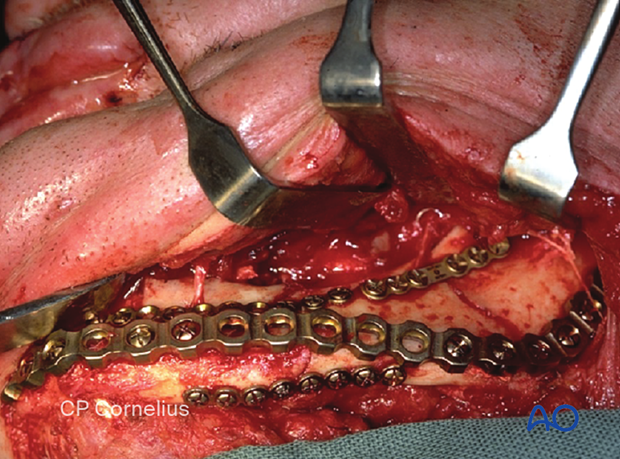
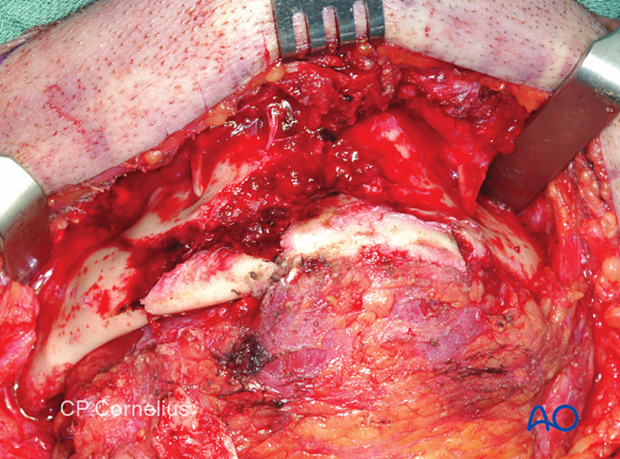
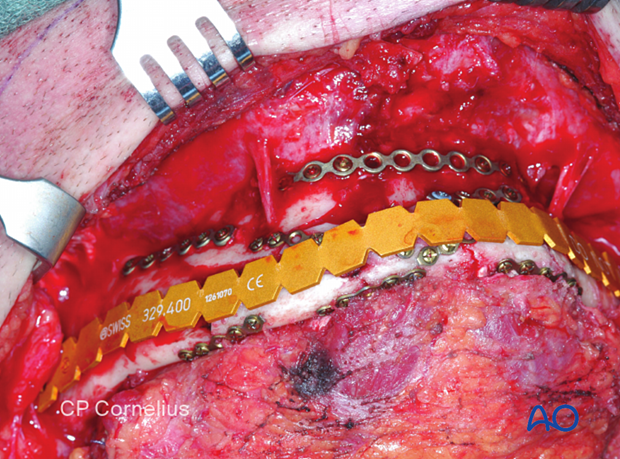
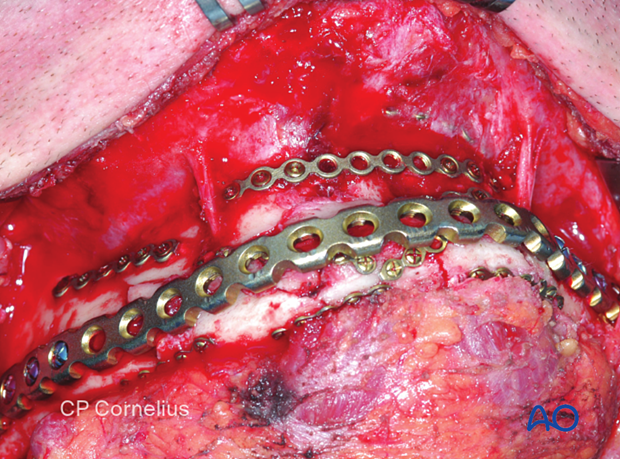
This intraoperative series shows images of a reduction and fixation of a comminuted fracture in the mandibular body.
The submandibular approach was used to expose a displaced complex fracture of the mandibular body.
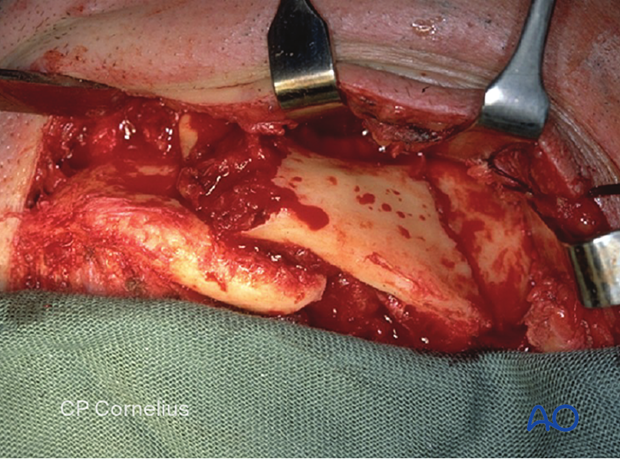
A preliminary reduction of the main fragments can be seen.
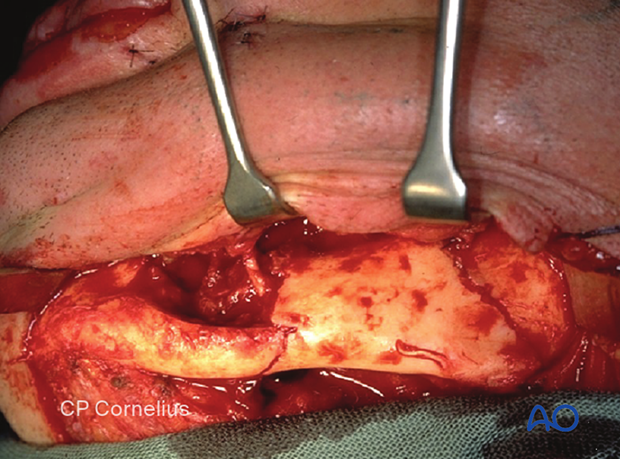
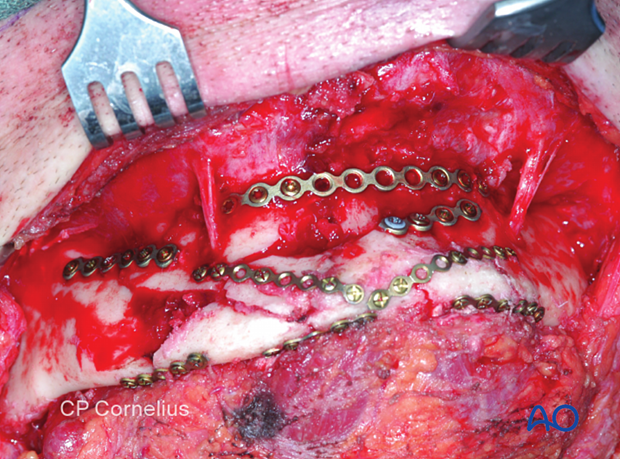
Realignment of all fragments and simplification of the fracture using miniplates on the superior border and the basal border. The anatomically reduced fragments position is maintained and facilitates the bending and contouring of a reconstruction plate.
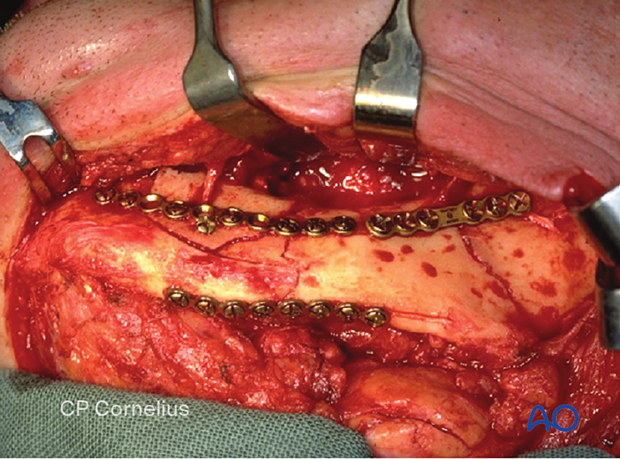
The contoured reconstruction plate was temporarily fixed using holding clamps.
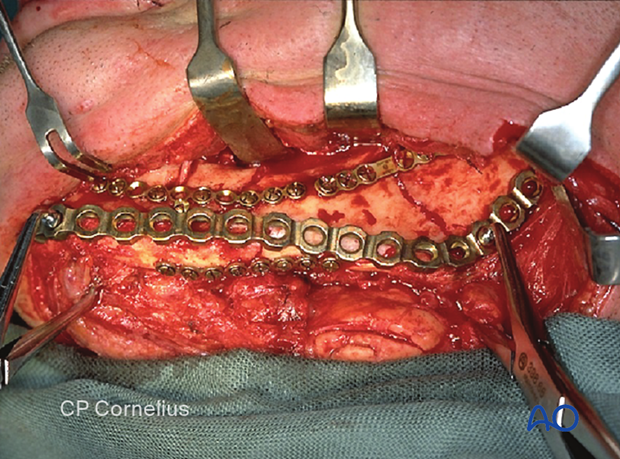
Screw fixation of the reconstruction plate with several screws (at least three) on either side of the comminuted area to achieve load-bearing fixation.
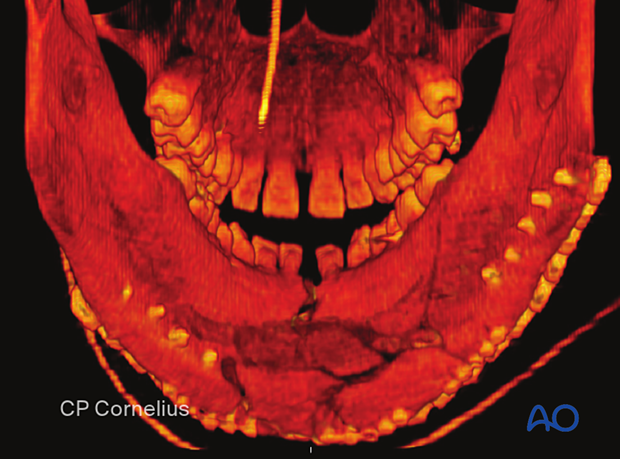
9. Case example II
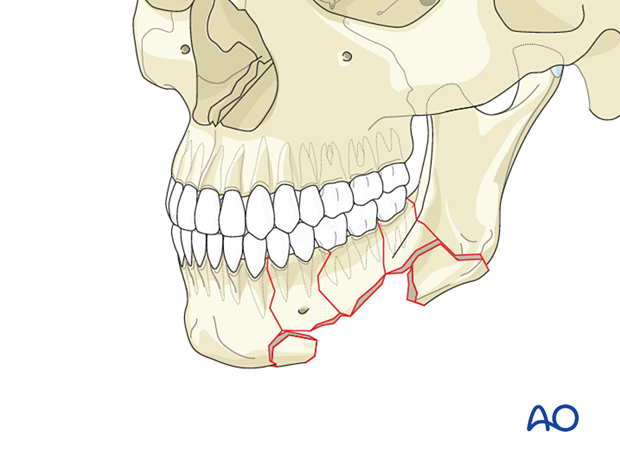
Comminution zone extending from the anterior mandible into the mandibular body on the left.
Anterior 3-D CT view.
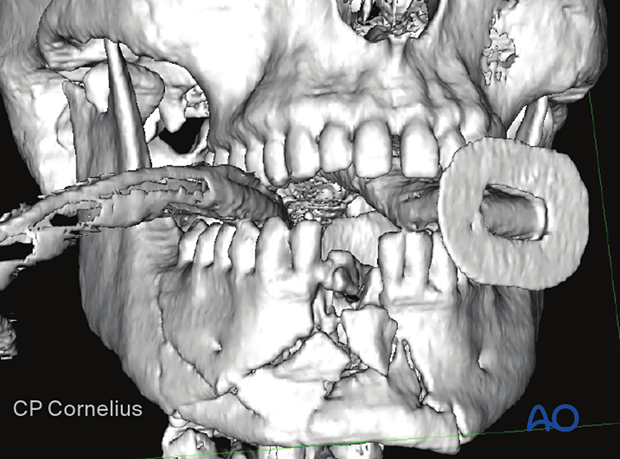
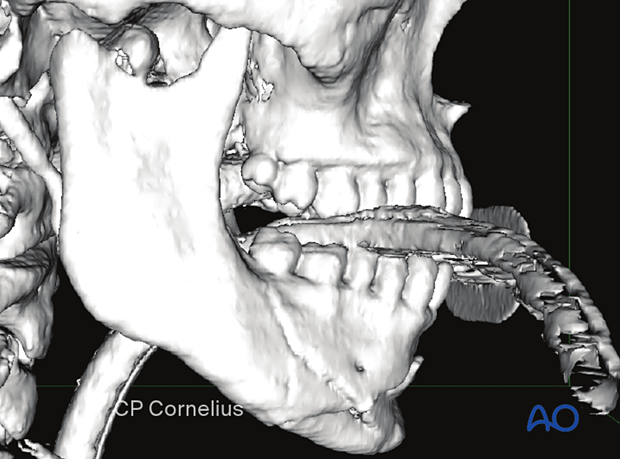
Lateral 3-D CT view.
Note the anteromedially displaced condylar head fracture.
The posterior 3-D CT view shows that the width of the mandible is slightly broadened.
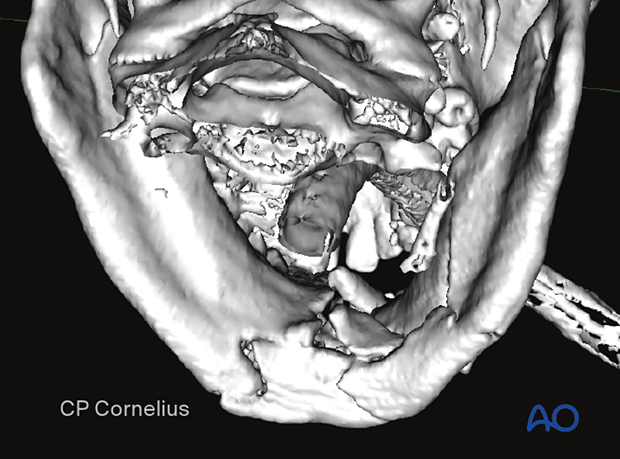
The fracture site was exposed using bilateral submandibular incisions combined with a submental incision (apron flap).
Fracture is reduced and simplified with miniplates. The miniplates are located at the superior border on the lateral bony surface and below the mandible's basal border to achieve an ideal three-dimensional reconstruction.
A template was contoured to facilitate the subsequent bending of a long-spanning reconstruction plate.
Locking screw fixation of the reconstruction plate in intact bony regions adjacent to the comminuted fracture.
The reduction and fixation were checked postoperatively using a:
- Lateral 3-D CT view
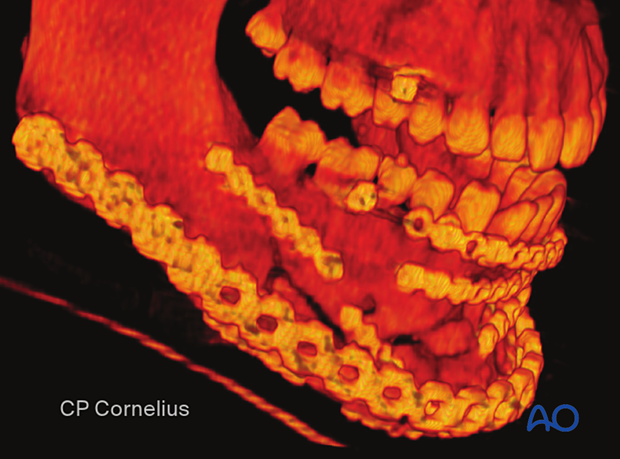
- Anterior 3-D CT view

- Posterior 3-D CT view
The posterior 3D CT view shows the restored width of the mandibular arch. Note the screw tips after bicortical fixation of the reconstruction plate (five screws in the right angle, four screws in the left anterior and midbody regions).
10. Aftercare following ORIF of mandibular symphysis, body, angle, and ramus fractures
Use of jaw bra
If significant degloving of the soft tissues of the mandible has occurred, there may be a consideration for using a jaw bra or similar support dressing.
Arch bars
If arch bars or MMF screws are used intraoperatively, they are usually removed at the conclusion of surgery if proper fracture reduction and fixation have been achieved. Arch bars may be maintained postoperatively if functional therapy is required or if required as part of the fixation.
X-Rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken after 4–6 weeks.
Follow up
The patient is examined approximately 1 week postoperatively and periodically thereafter to assess the stability of the occlusion and to check for infection of the surgical wound. During each visit, the surgeon must evaluate the patient's ability to perform adequate oral hygiene and wound care and provide additional instructions if necessary. Many patients need to be seen regularly for replacement of their intermaxillary elastics and to encourage range of motion in their TMJ in the later course of the treatment.
Follow-up appointments are at the discretion of the surgeon and depend on the stability of the occlusion on the first visit. If a malocclusion is noted and treatable with training elastics, weekly appointments are recommended.
The patient should be warned to continue routine follow up with their dentist. Fractures near the dental roots can often result in delayed loss of tooth viability, requiring periapical films and additional dental procedures.
Malocclusion
If a malocclusion is detected, the surgeon must ascertain its etiology (with appropriate imaging technique). If the malocclusion is secondary to surgical edema or muscle splinting, training elastics may be beneficial. The lightest elastics as possible are used for guidance, because active motion of the mandible is desirable. Patients should be shown how to place and remove the elastics using a hand mirror.
If the malocclusion is secondary to a bony problem due to inadequate reduction or hardware failure or displacement, elastic training will be of no benefit. The patient must return to the operating room for revision surgery.
Basic postoperative instructions
DietDepending upon the stability of the internal fixation, the diet can vary between liquid and semi-liquid to “as tolerated”, at the discretion of the surgeon. Any elastics are removed during eating.
Patients having only extraoral approaches are not compromised in their routine oral hygiene measures and should continue with their daily schedule.
Patients with intraoral wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch-bars and any elastics makes this a more difficult procedure than normal. A soft toothbrush (dipping in warm water makes it softer) should be used to clean the surfaces of the teeth and arch-bars. Any elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least three times each day to help sanitize the mouth. Chlorohexidine may cause staining of the teeth and should not be used longer than necessary. For larger debris, a 1:1 mixture of hydrogen peroxide (0.25%)/chlorhexidine (0.12%) can be used. The bubbling action of the hydrogen peroxide helps remove debris. A water flosser, providing a water jet, is a very useful tool to help remove debris from the wires. If a this is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Physiotherapy can be prescribed at the first visit and opening and excursive exercises begun as soon as possible. Goals should be set, and, typically, 40 mm of maximum interincisal jaw opening should be attained by 4 weeks postoperatively. If the patient cannot fully open his mouth, additional passive physical therapy may be required such as Therabite® or tongue-blade training.