Infected fracture with or without bone loss
1. Diagnosis
Definition
Open fractures can generally be regarded as contaminated. Since fractures in the dentate area have communication with the oral cavity, these are considered open fractures.
Infections with clinical relevance show swelling, pain, fever, redness, and exudation of pus. In the case of acute infection, radiographic signs can be absent. Chronic cases exhibit the typical signs of osteomyelitis.
Additional considerations
Patients with infected fractures often present a constellation of problems:
- Noncompliance
- Alcohol addiction
- Drug abuse
- Self-neglect and social deprivation
- Imprisonment
- Dementia
Medical risk factors:
- Chronic corticoid medication
- Immune deficiency
- Diabetes mellitus
- Osteopathy
Passeri LA, Ellis E 3rd, Sinn DP. Relationship of substance abuse to complications with mandibular fractures. J Oral Maxillofac Surg. 1993 Jan;51(1):22-5.
Special conditions influencing adequate internal fixation
Instability produces and maintains the infectious process.
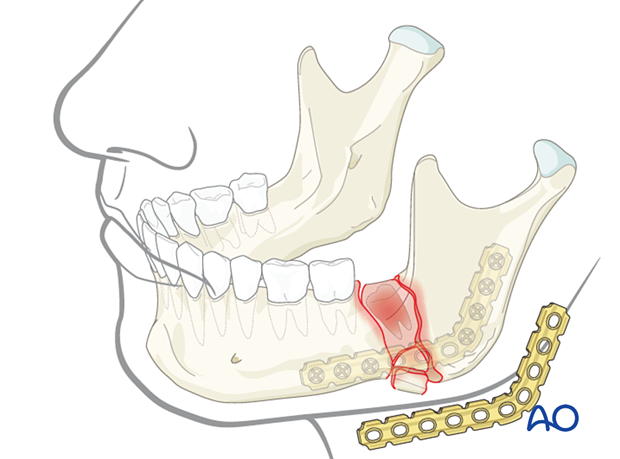
Osteosynthesis of an acutely infected fracture requires high rigidity (absolute immobility). Therefore, the 2.4 locking reconstruction system is recommended. It is essential not to place any screws into the infected bone area and that the reconstruction plate functions as a bridging device. Large regions of infected or necrotic bone require curettage and either immediate or delayed cancellous bone grafting. Antibiotic therapy alone does not eliminate the infection as long as the fracture is unstable.
Clinical findings
Clinical photograph showing an infected fracture between the first and second molar. The pericoronal gingiva of the second molar contains pus, and the swelling fills the vestibular sulcus.

Imaging
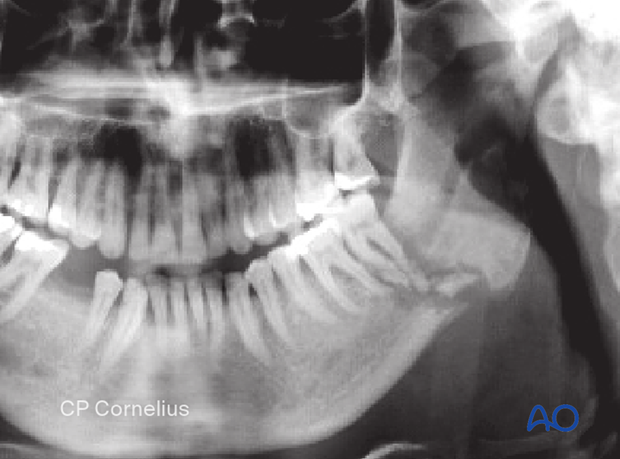
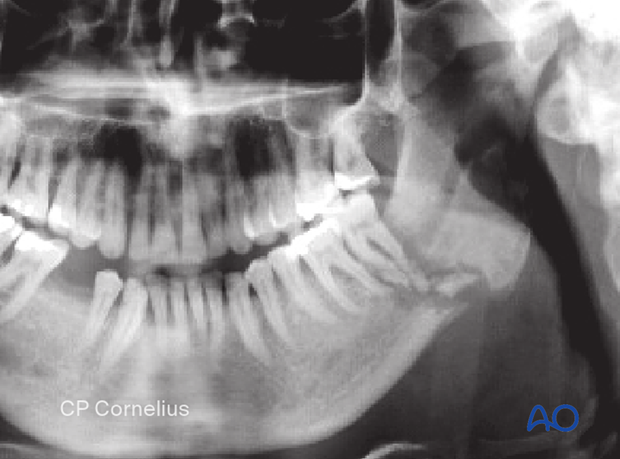
OPG confirms the clinical diagnosis of an infected fracture site in the posterior mandibular body with radiolucency around the second molar and an extended fracture zone containing several bone sequestra.
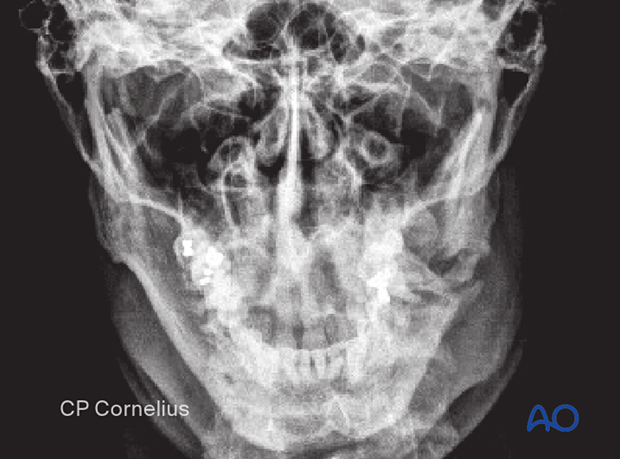
This image is the PA view of the same case.
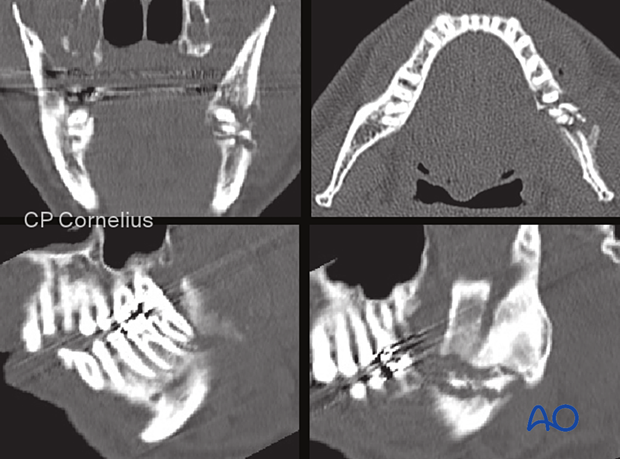
These CT scans of the same patient show the details of the fracture zone.
2. Principles
Formal pathogenesis
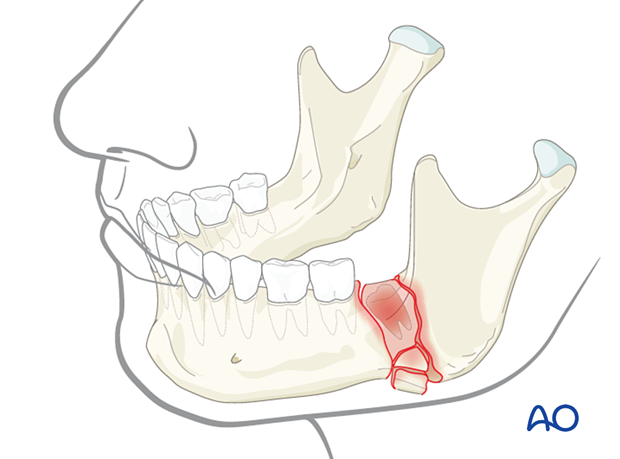
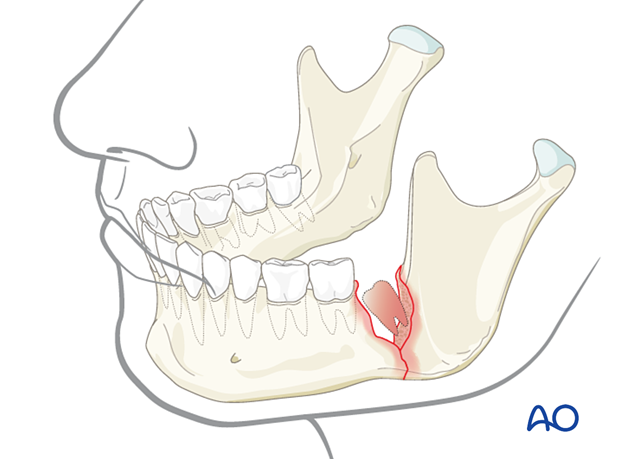
A predilection zone for infected fractures is in the posterior mandibular body or the angle region. Contributing factors in this area are impacted or partially impacted wisdom teeth. Chronic infection leads to osteomyelitis with inflammatory resorption and sequestration of the bone in the fracture line's proximity.
The current concept is that the infection and osteomyelitis are propagated by the fracture fragments' instability and mobility.
When dealing with osteomyelitis, the infected fracture will be debrided, and the patient can be left with a bony defect for later repair.
If the bony defect extends throughout the entire fracture, grafting will be necessary.
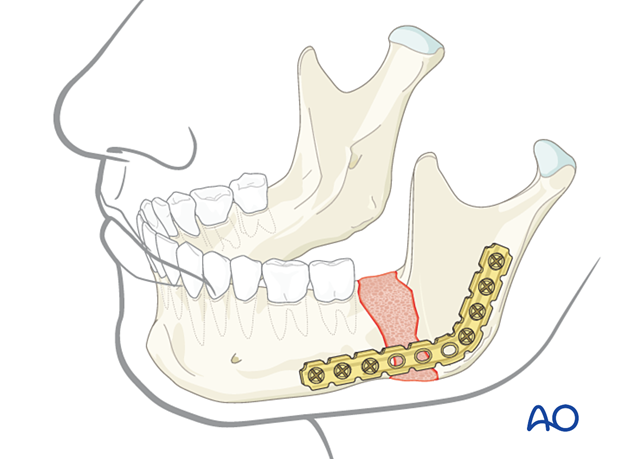
Choice of implant
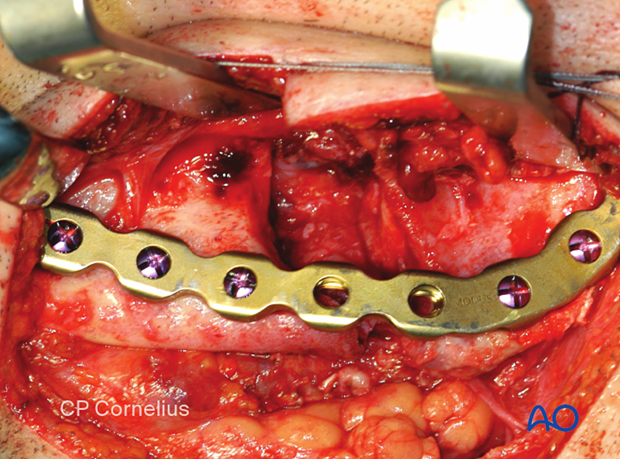
Since large plates' rigidity is defined by the number and diameter of the inserted screws, it is recommended to use reconstruction plates compatible with large diameter screws only, ie, 2.4 or 3.0 mm screws.
The plate's span has to cover such a length that at least three screws on each side of the defect can be inserted into the intact bone. Very often, with large span defects, it is advisable to have four or more screws on each side of the defect.
3. Sequestrectomy and debridement
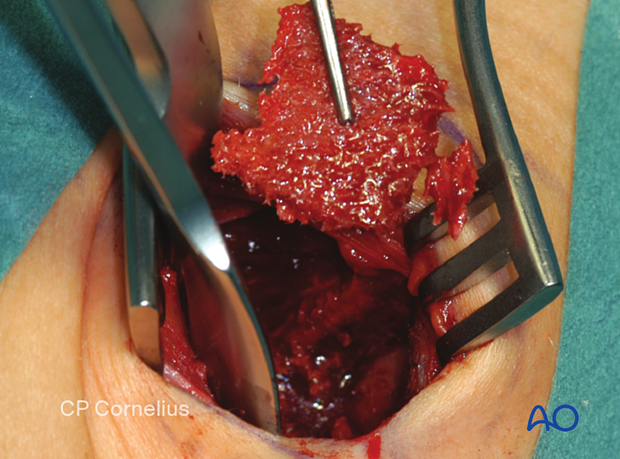
Clearing of the infected area
After a wide exposure, the infected area must be cleared of any granulation tissue and devitalized bone.
The extent of the exposure must anticipate applying a large reconstruction plate allowing for the placement of at least three screws on each side away from the defect.
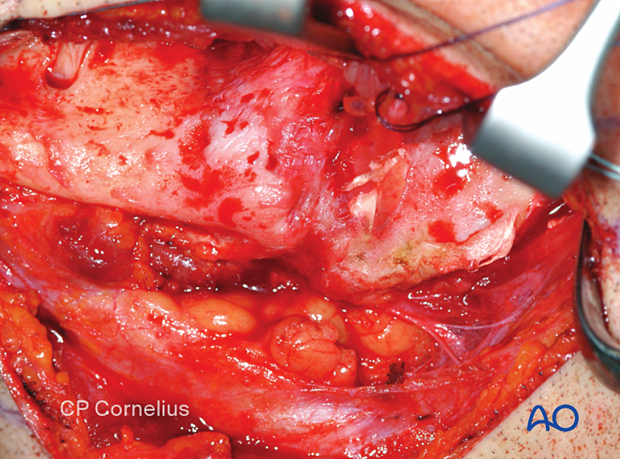
Sequestrectomy
Remove devitalized bone (sequestra) and decorticate the bony surfaces of the fractured ends.
Sharp bony edges should be smoothed. The remaining bone surfaces should have bleeding patches to make sure that they are vital.
The mandibular nerve should be preserved, if not irreversibly damaged by the chronic infectious process.
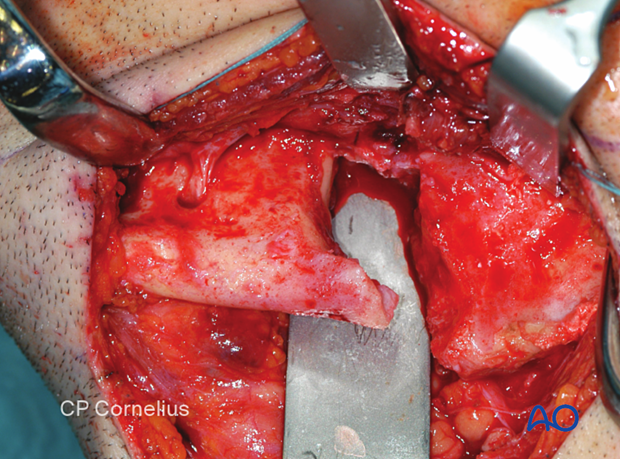
Tooth and sequestra removed.

4. Load-bearing osteosynthesis
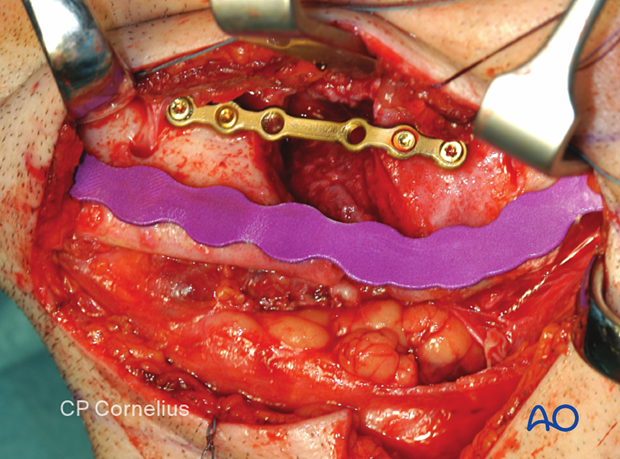
MMF and preliminary fragment fixation
The tooth-bearing distal part of the fracture is secured via MMF. The condyle bearing part is repositioned, and a small (adaptation) plate is applied onto the superior border of the defect to maintain the fragments' position while the reconstruction plate is adapted and secured.
Prior to adapating and securing the reconstruction bone plate, it is useful to release MMF at this point and assure that the proper condylar position has been achieved by the adaptation plate. Opening and closing the mouth should be performed to assure the proper occlusion before again securing MMF and applying the reconstruction bone plate. If the proper occlusion has not been achieved, MMF should be secured and the adaptation plate removed, followed by re-seating the condylar fragment and reapplying the adaptation plate.
Contouring the plate
The load-bearing bridging plate is contoured to the lower border with the help of a malleable template.
The contour of the plate must match the template in all three dimensions.

Click here for a detailed description of the bending procedure.

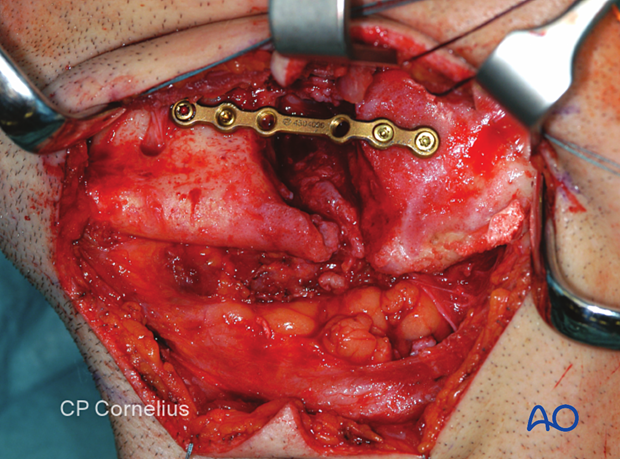
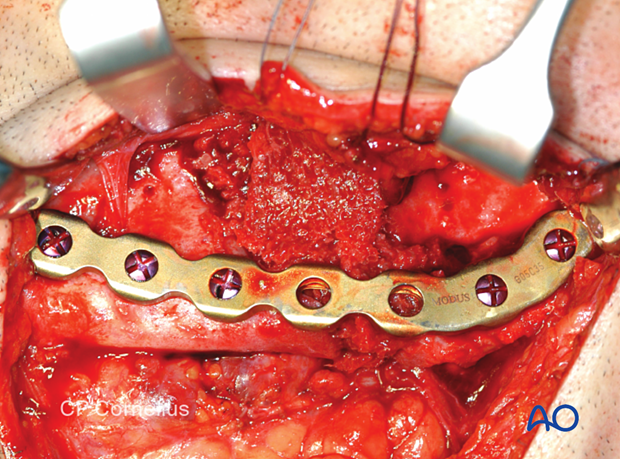
Plate fixation
The bridging plate is firmly applied to the bone with plate forceps, and the screws are inserted in the usual manner, starting with the screws closest to the defect zone.
Screws must not be inserted close to the fracture gaps.
Click here for a detailed description of screw insertion into locking plates.
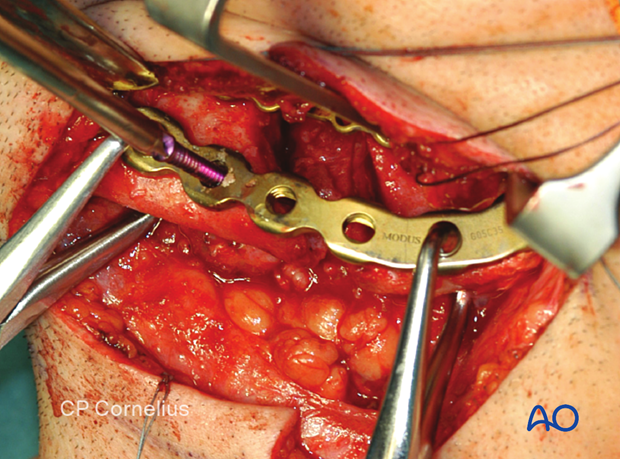
When the reconstruction plate's fixation is completed, the adaptation plate at the mandible's superior border may be removed.
Occlusion check
Load-bearing osteosynthesis is stable and cannot be influenced postoperatively using elastic traction. Therefore, the occlusion must be checked after plate application. In malocclusion cases, it must be decided whether the occlusion can be corrected by minimally grinding the teeth or repositioning the bone and plate. The revision of the osteosynthesis may be difficult because of reduced bone quality and reduced bony buttressing.
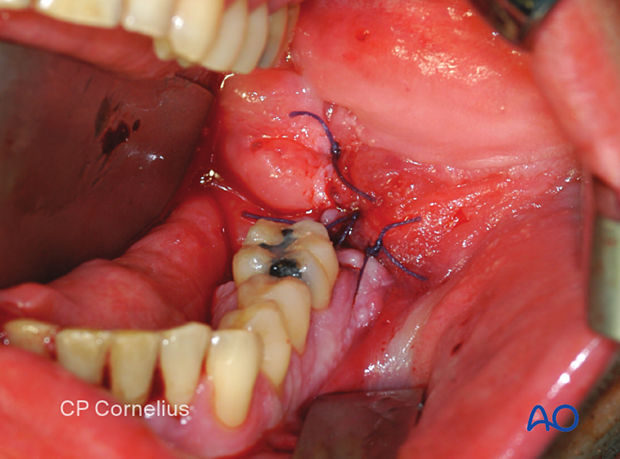
Removal of MMF device
Usually, this type of fracture occurs in compromised or noncompliant patients. Therefore, one might consider removing all MMF appliances before intraoral wound closure (at the tooth extraction site). MMF removal can facilitate oral hygiene.
5. Intraoral soft-tissue coverage
The intraoral mucoperiosteum is closed using the envelope technique with a flap derived from the lateral vestibule.
This is done before any bone grafting to separate the defect from the oral cavity.
6. Same stage bone grafting
Bone harvesting
If immediate bone grafting is desired, bone is harvested from the anterior iliac crest or the tibial head according to preference and the amount of bone graft needed.
In this case, a corticocancellous piece and cancellous chips were taken from the iliac crest's inner table.
The corticocancellous piece was shaped approximately to the size of the defect. Holes were drilled to increase the bony surface to enhance revascularization.
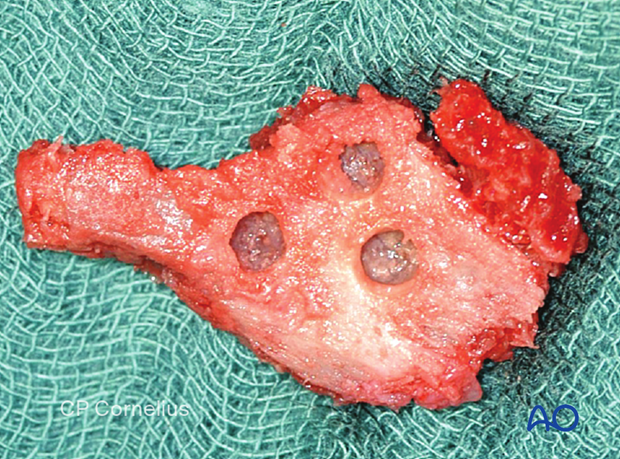
Cancellous chips were harvested to augment and fill in the defect.

Applying the bone graft
All bone grafts are inserted through the external approach.
The shape of the corticocancellous bone graft is checked and introduced into the defect.
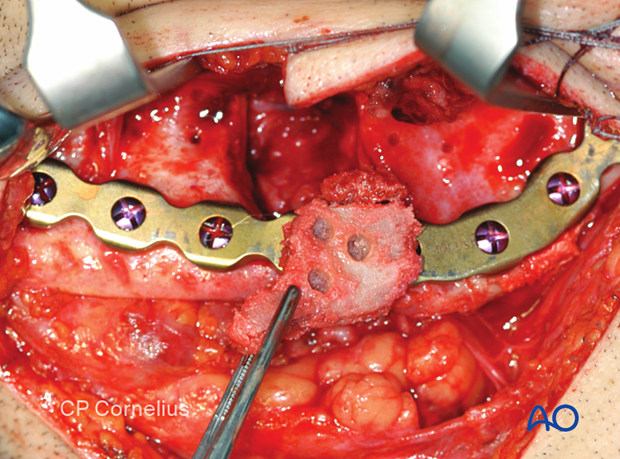
The remaining dead space is filled with cancellous chips, which are further used to augment the area.
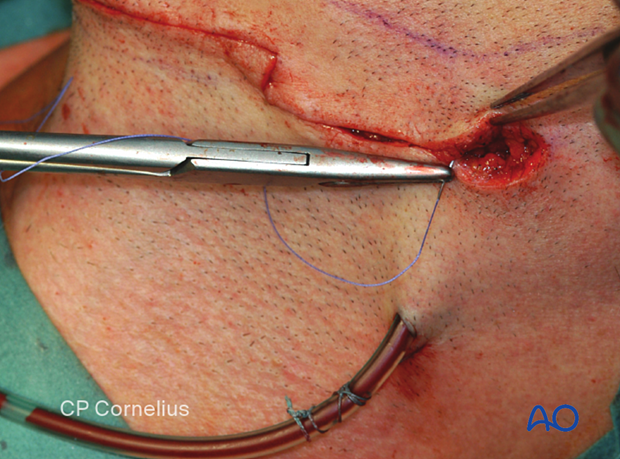
7. Extraoral wound closure
The use of suction drain is at the discretion of the surgeon. The external wound is closed in layers.
8. Completed osteosynthesis
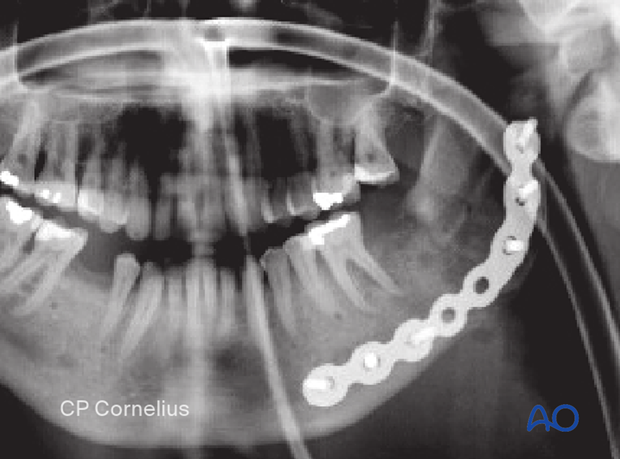
The Panoramic x-ray shows the plate osteosynthesis bridging the defect zone in the left posterior mandibular body.
Note: there are three screws on each side of the defect, and these are placed away from the fracture. The defect zone appears opaque because of the bone graft.
A nasogastric tube can be used to feed the patient to enhance intraoral hygiene.
9. Aftercare following treatment of infected fractures
Removal of arch bars and MMF screws
If arch bars or MMF screws are used, they may be removed at the end of the surgery or maintained for several weeks at the surgeon's discretion.
X-rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken at the 4–6-week interval.
Follow up
It will be necessary to see the patient after approximately one week to assess the occlusion and the status of the incision/wound. In an infected mandibular fracture, aftercare includes observing several factors, including the unique wound situation, the general health condition (nutritional status, diabetes, and particular medication), psychosocial status, economic situation, and specific local regimens. The surgeon must also evaluate patient response to the current antibiotic regimens and check for systemic parameters (for example, CRP, white cell blood count, erythrocyte sedimentation rate). Patients will have to be re-examined periodically to rule out recurring signs of infection. At each visit, the surgeon must evaluate the patient's ability to perform adequate oral hygiene and wound care. It may be necessary to provide additional instruction to ensure appropriate hygiene and wound care.
Follow-up appointments are at the surgeon's discretion and depend on the occlusion's stability noted on the first visit. If a malocclusion is noted and treatable using training elastics, weekly appointments to determine the progression are recommended.
Malocclusion
If a malocclusion is detected, the surgeon must ascertain its etiology (using the appropriate imaging technique). If the malocclusion is secondary to surgical edema or muscle splinting, training elastics may be beneficial. The lightest elastics possible are used for guidance because the active motion of the mandible is desirable. Patients should be shown how to place and remove the elastics using a hand mirror.
If the malocclusion is secondary to a bony problem due to inadequate reduction or hardware failure or displacement, elastic training will be of no benefit. The patient must return to the operating room for revision surgery.
Basic postoperative instructions
DietDepending upon the internal fixation's stability, the diet can vary between liquid and semi-liquid to "as tolerated" at the surgeon's discretion. Any elastics are removed during eating.
Patients with only extraoral approaches are not compromised in their routine oral hygiene measures and should continue with their daily schedules.
Patients with intraoral wounds must be instructed on appropriate oral hygiene procedures. The presence of the arch-bars and any elastics make this a more complicated procedure than usual. A soft toothbrush (dipping in warm water makes it softer) should be used to clean the teeth and arch bars surfaces. Any elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least three times each day to sanitize the mouth. For larger debris, a 1:1 mixture of hydrogen peroxide (0.25%) /chlorhexidine (0.12%) can be used. The bubbling action of the hydrogen peroxide helps remove debris. A Waterpik® is a handy tool to help remove debris from the wires. If a Waterpik is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
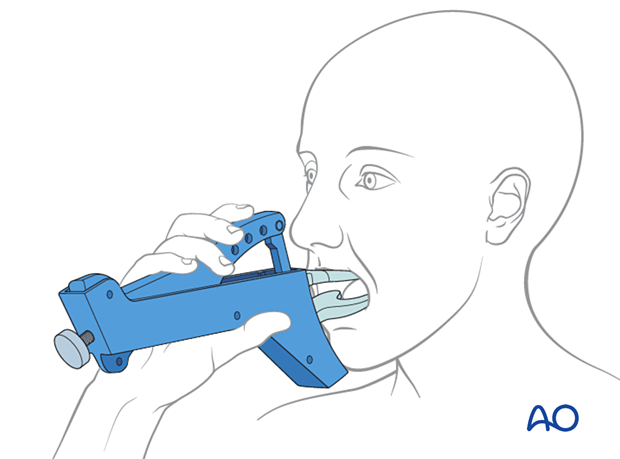
Physiotherapy can be prescribed at the first visit, and opening and excursive exercises begun as soon as possible. Goals should be set, and, typically, 40 mm of maximum interincisal jaw opening should be attained by four weeks postoperatively. If the patient cannot fully open his mouth, additional passive physical therapy may be required, such as Therabite ® (illustrated) or tongue-blade training.