Multiple fractures
1. General considerations
The mandible is similar in shape to an arch, and therefore multiple fracture sites are common. They can be grouped into the broad categories listed below:
- Unilateral fractures (double or multiple unilateral)
- Bilateral fractures
- Associated contralateral condyle fracture
- Bilateral condyle fractures with associated symphysis/anterior body fractures
Whenever one fracture of the mandible is identified, the surgeon must always suspect that one or more additional fractures are present. Careful clinical and x-ray examination will assist in establishing the correct diagnosis.
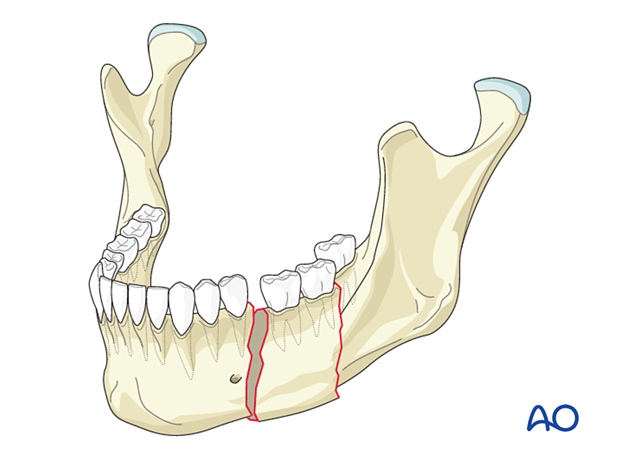
2. Unilateral fractures (double or multiple unilateral)
General considerations
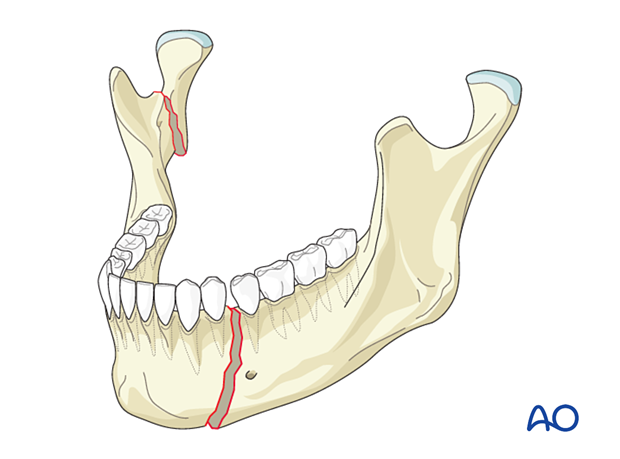
This injury occurs when a large amount of force is applied to a specific area of the mandible.
Treatment considerations
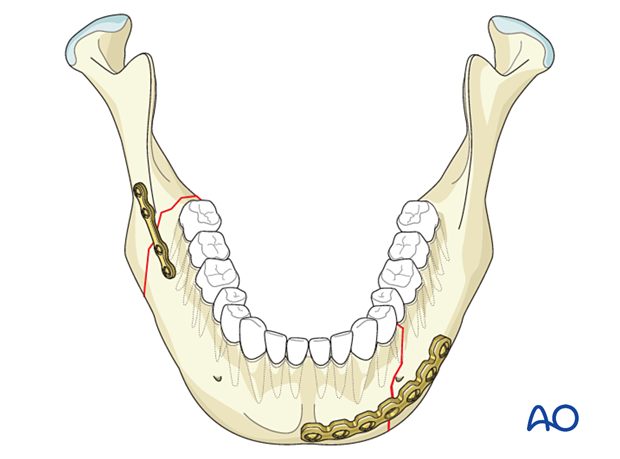
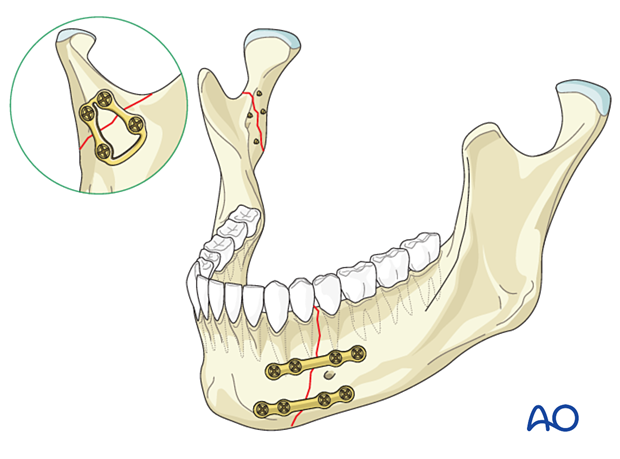
If the fractures are located unilaterally close to each other, the intermediate fragment is fixed with long spanning adaptation or, more frequently, reconstruction plates along the inferior border (load-bearing).
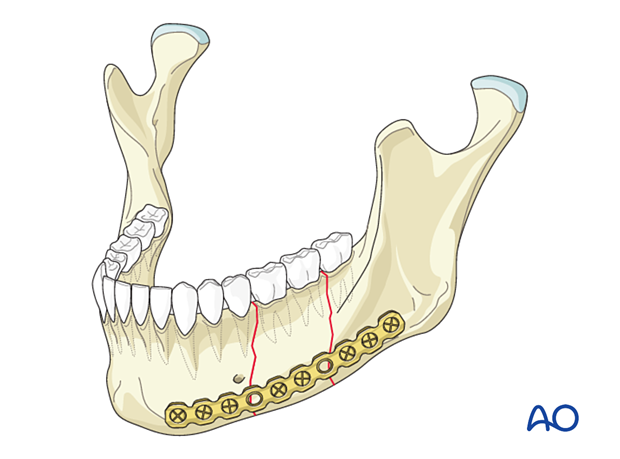
If the fractures are unilaterally located far apart from one another, the surgeon should choose rigid internal fixation (load-bearing) for both fracture sites as two fractures on the same side require more stable fixation than if they would have been treated as individual fractures.
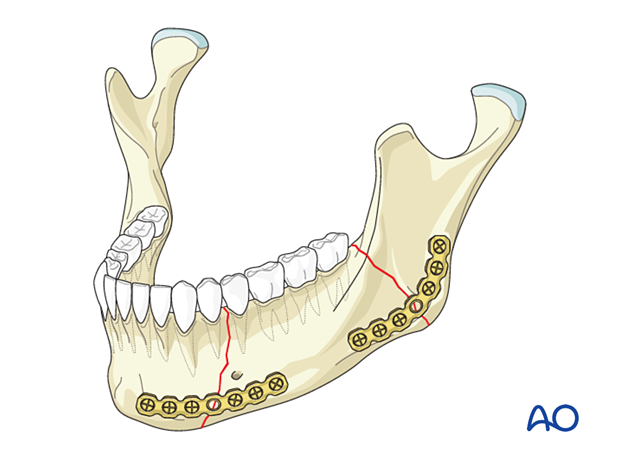
3. Bilateral fractures
General considerations
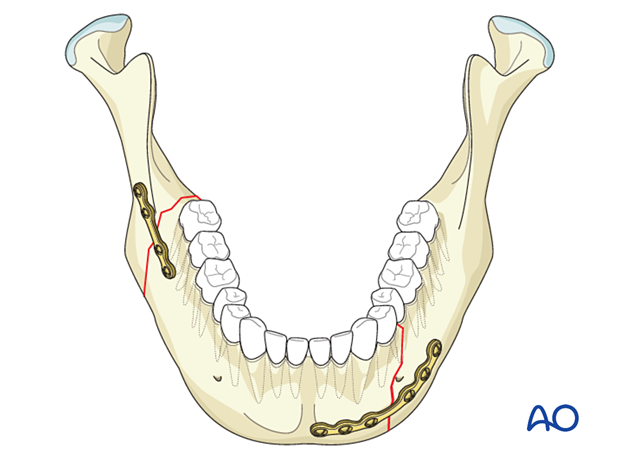
Bilateral mandibular fractures are commonly identified in clinical practice. The most common combination of fractures is an angle combined with a contralateral fracture through the body or symphysis.
When there is a combination of a mandibular body/symphysis and contralateral angle fracture, one of the fractures should be treated with more stability to neutralize the twisting forces at the inferior border, especially in the angular area.
Treatment considerations
Fractures in the tooth-bearing area of the anterior mandible are generally treated first to establish the ideal occlusion. Fractures in the regions without teeth (posterior body/angle/ramus/condyle) are usually treated secondarily.
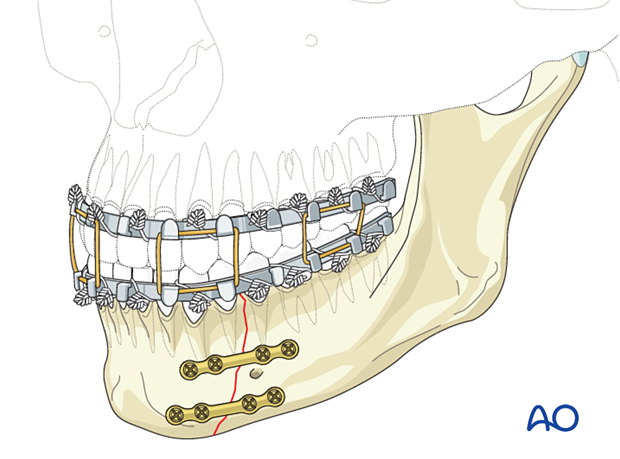
The angle fracture is most commonly treated with one miniplate fixation along the upper border of the lateral surface of the mandible, and the contralateral fracture through the body/symphysis is treated with more rigid fixation.
Various fixation schemes are available for the fracture of the body/symphysis (eg, two miniplates, a large or extra-large profile 2.0 locking plate, or a reconstruction plate).
Rughubar V, Vares Y, Singh P, Filipsky A, Creanga A, Iqbal S, Alkhalil M, Kormi E, Hanken H, Calle AR, Smolka W, Turner M, Csáki G, Sánchez-Aniceto G, Pérez D, Cornelius CP, Alani B, Vlad D, Kontio R, Ellis E 3rd. Combination of Rigid and Nonrigid Fixation Versus Nonrigid Fixation for Bilateral Mandibular Fractures: A Multicenter Randomized Controlled Trial. J Oral Maxillofac Surg. 2020 Oct;78(10):1781-1794.
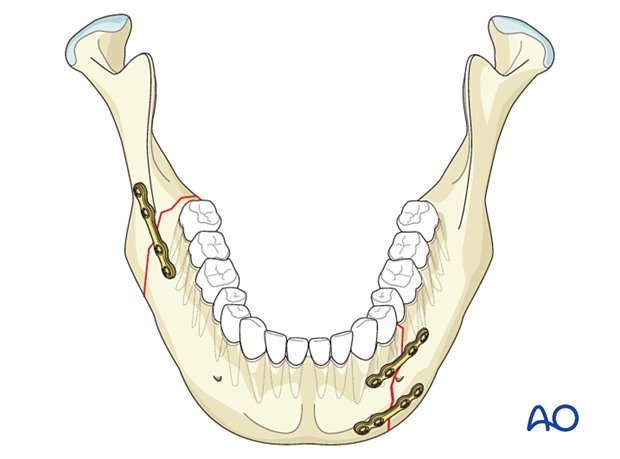
Simple right-angle fracture fixed with one miniplate along the upper border of the lateral mandibular surface and the simple left body fracture fixed utilizing a large profile locking plate 2.0 plate.
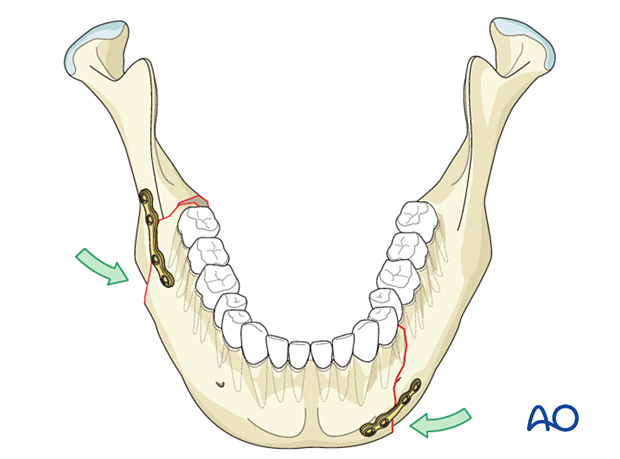
4. Fractures with contralateral condylar fractures
General considerations
This fracture combination usually results from a direct blow to the ipsilateral mandibular body, which fractures and causes a mandibular condyle fracture on the contralateral side.
Treatment considerations
Fractures in the tooth-bearing area of the anterior mandible are generally treated first to establish the ideal occlusion. Fractures in the condyle are usually treated secondarily.
The fracture through the body/symphysis is most commonly treated using stable fixation, which offers the choice of treating the condyle fracture closed or open.
One can choose various stable/rigid fixation schemes for the fracture of the body/symphysis. One can use two miniplates, a heavy locking 2.0 plate, or a reconstruction plate.
If it is decided that the condylar fracture will be treated closed, postoperative arch bars and training elastics can be used. Training elastics will allow postoperative physical therapy to rehabilitate the condyle.
5. Bilateral condylar fractures with symphysis/anterior body fracture
General considerations
One of the most challenging fractures to manage is the bilateral condylar fracture with an anterior body or symphyseal fracture.
Commonly, the condylar segments are displaced, and the mandible is widened with an opening of the lingual symphyseal cortex.
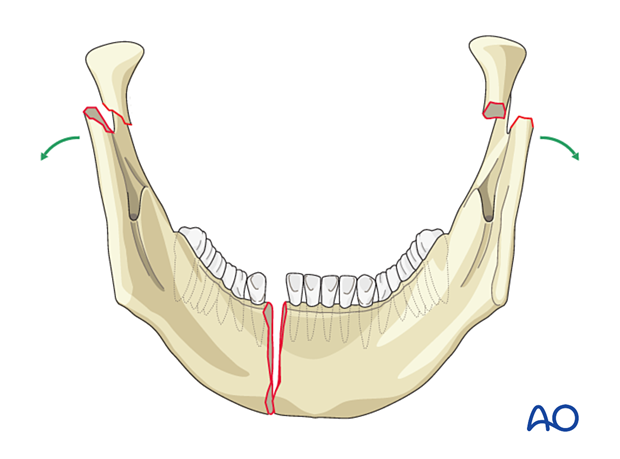
This CT shows mandibular widening, resulting in a "U"-shaped mandible instead of the typical "V" shape.

Treatment considerations
Treatment of bilateral condyle and symphysis/anterior body fractures usually begins with the most anterior fracture component and ends with the most posterior one.
The reduction and stabilization of the anterior fracture are crucial for the restoration of the mandible's transverse dimension.
If the mandible's exact transverse dimension is not restored, the transverse dimension of the subcondylar region can never be restored.
Adequate reduction of the fractured symphysis on the lingual side before fixation is crucial.
When the anterior osteosynthesis is performed with a strong plate, some overbending may be required to close the lingual gap.
The fixation of the subcondylar fracture(s) is/are usually performed secondarily.














