Fractures in the edentulous atrophic mandible
1. Diagnosis
General considerations
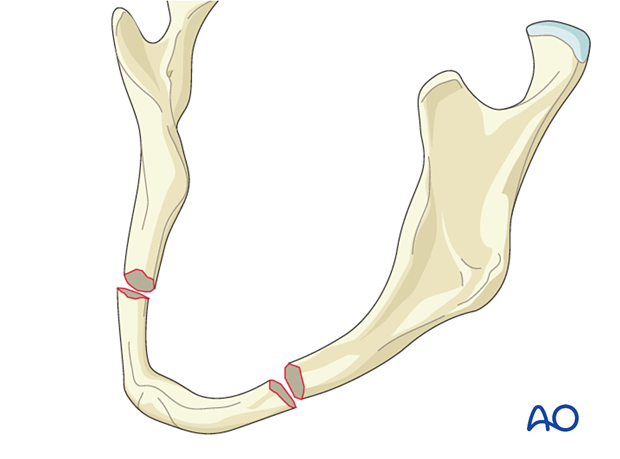
With increasing mandibular atrophy, the physical size of the mandible decreases. In the severely atrophic mandible, even very minor trauma can cause a fracture. Additionally, pathologic fracture during mastication can occur. Very often, due to the fragile nature of the jaw, these fractures occur bilaterally.
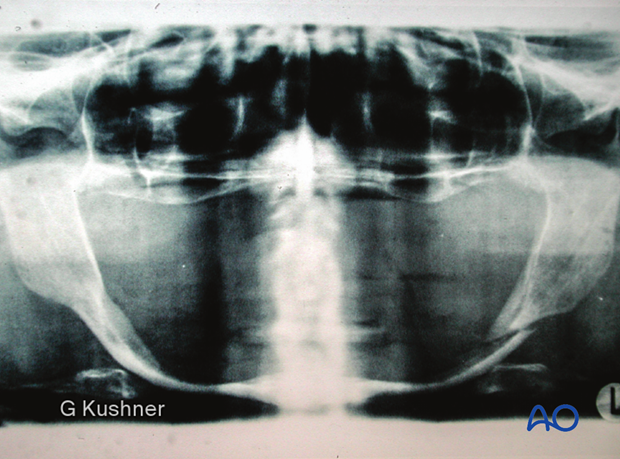
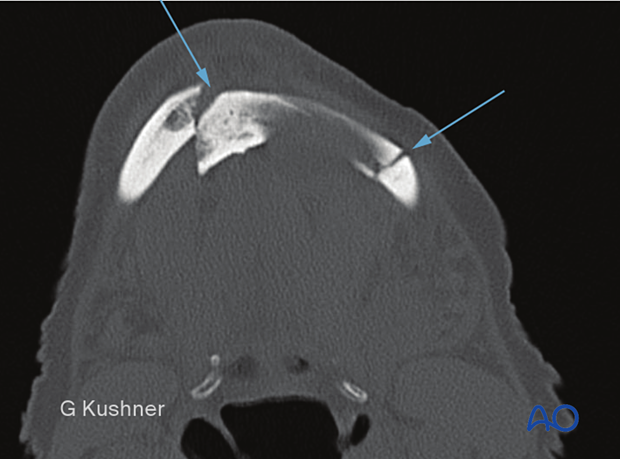
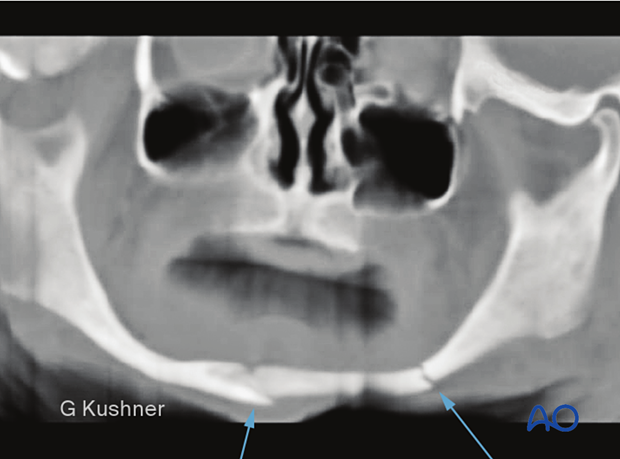
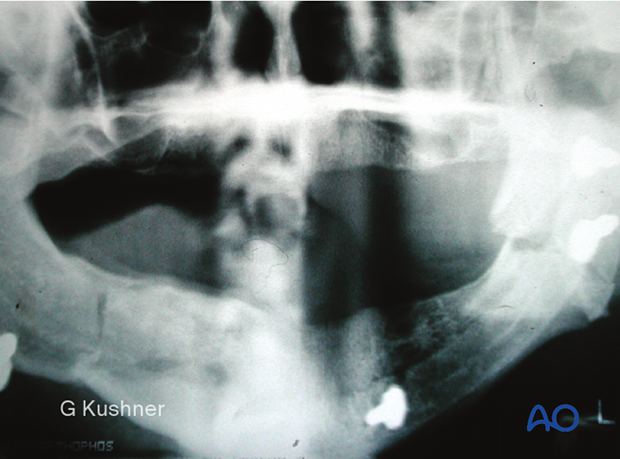
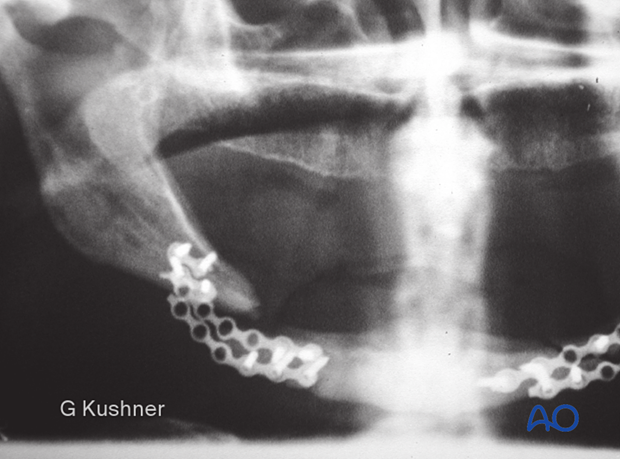
Orthopantomogram (OPG), mandible series radiograph, and CT scans can be used to diagnose and plan the treatment of the atrophic edentulous mandible fractures.
Clinical examination
The patient shows extraoral ecchymosis associated with an atrophic edentulous mandible fracture.
The patient exhibits pain and mobility of the anterior mandible.

The patient shows intraoral ecchymosis in the floor of the mouth associated with an atrophic edentulous mandible fracture.

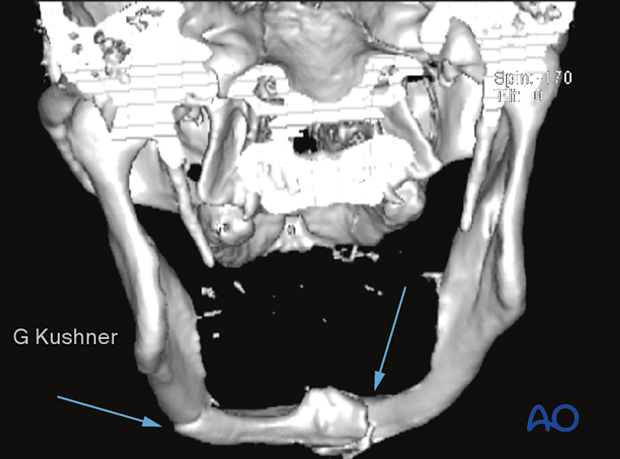
A typical example of an atrophic edentulous mandible fracture
Axial CT scan showing bilateral fractures.
Although there appears to be large bone stock, this patient's mandible has only approximately 7 mm of vertical height.
This CT image demonstrates the posterior displacement of the segment.
This panoramic radiograph demonstrates both the fracture and the extreme amount of vertical atrophy in the above case.
2. Decision/Indication
Observation and soft diet
This image is a 3D reconstruction of the same case.
Atrophic edentulous mandible fracture patients are often elderly with medical problems presenting severe anesthetic risks. Observation may be indicated for patients medically unfit for general anesthesia.
One major complication of observation and soft diet would be nonunion of the mandibular fracture.
Closed reduction
Historically, atrophic edentulous fractures were treated closed by wiring in the patients' dentures or fabricating Gunning style splints with postoperative maxillomandibullary fixation (MMF).
Standard treatment with closed reduction often resulted in prolonged periods of MMF, which was difficult for these patients. Additionally, the fractures were often poorly aligned. Postoperative malunions and nonunions were very common.
This photograph shows a patient denture that has been modified by removal of the anterior teeth to permit intake of food during the period of MMF.
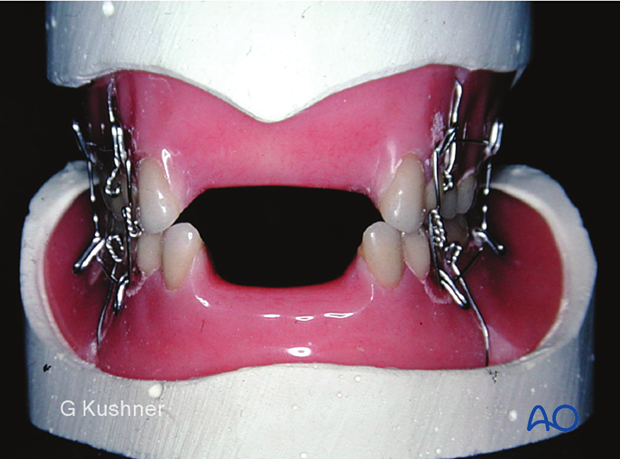
This photograph shows a Gunning style splint.

ORIF
Indication for ORIF is any displaced atrophic mandible fracture requiring surgical intervention.
Following the AO principles of anatomic reduction of fractures and immediate function, the ORIF of atrophic edentulous mandible fractures with load-bearing osteosynthesis has a distinct advantage for these patients. The technique has evolved to provide the patient with an excellent chance for bony union while mastication is preserved.
Literature supports the efficacy of this technique.
External fixation
Indications of an external fixator might be the temporary stabilization of a fracture while the patient is treated medically or if soft-tissue healing around the fracture site is required.
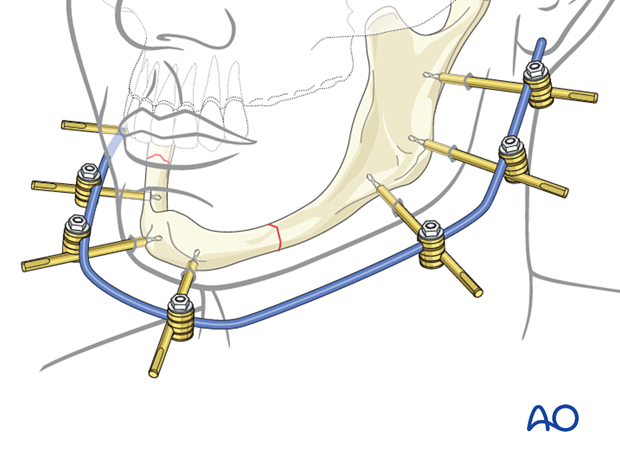
The incidence of complications, including malunion and nonunion, is significant when external fixators are used as they do not provide absolute stability at the fracture site.
3. Treatment of an edentulous atrophic fracture with a reconstruction plate
In the following, the treatment of an edentulous atrophic fracture with a reconstruction plate is described step-by-step.
4. Approach
Transcutaneous approach
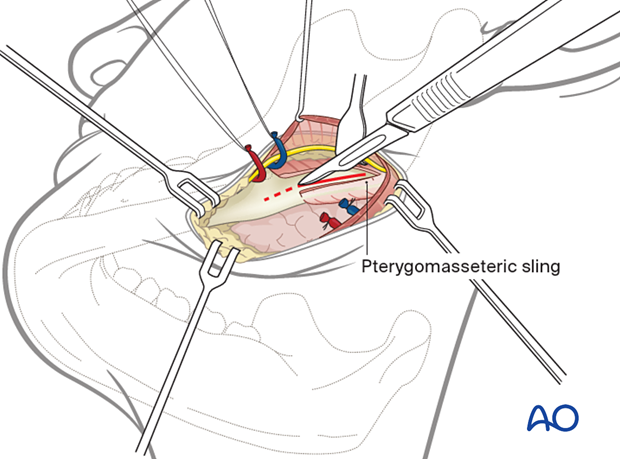
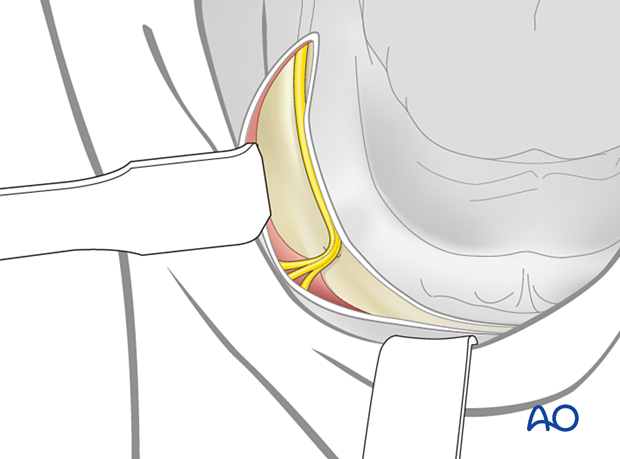
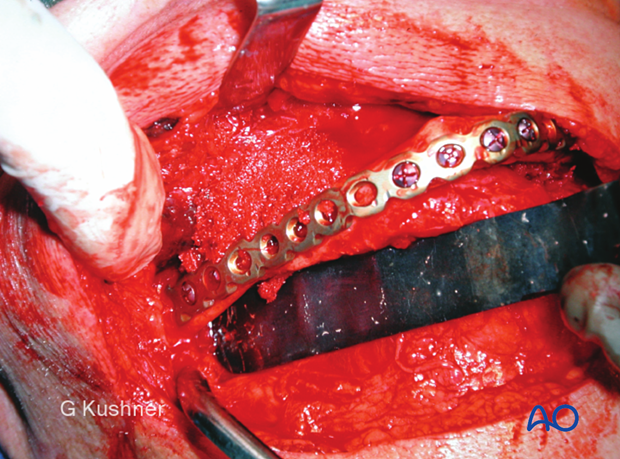
When treating atrophic edentulous mandible fractures, the surgeon will generally find it easier to use an extraoral surgical approach. The fracture fragments can be manipulated under direct visualization and stabilized while the reconstruction plate is bent and applied to the mandible.
Transoral approach
A transoral approach is possible but technically more difficult as the surgeon will need several sets of trained hands to retract the cheeks and tongue's soft tissues. Additionally, stabilization and fixation of the fractures are much more difficult via a transoral approach.
One should also be aware that the inferior alveolar nerve is located on the atrophic mandible's superior surface. Therefore, one must be extremely careful making intraoral incisions to expose atrophic fractures, or the nerve can be damaged.
5. Principles
The atrophic edentulous mandible fracture presents with several factors that make treatment very difficult.
- There is a lack of bone, which is generally cortical in nature and has lower healing potential.
- There are no teeth present to help reduce the fractures.
- Often the patients are elderly and medically compromised.
- Atrophic mandible fractures require transfacial open reduction, load-bearing internal fixation, and often immediate bone grafting.
- The biomechanical behaviour of an atrophic mandible is different to that of an edentulous mandible. This means that load sharing plates are not able to provide sufficient strength and load bearing plates must be used.
6. Choice of implant
General considerations
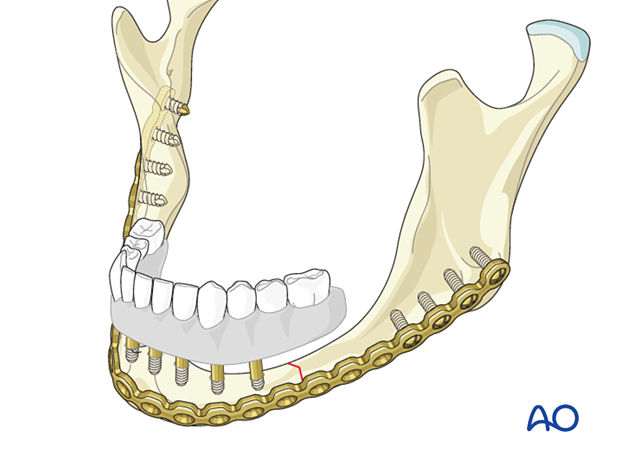
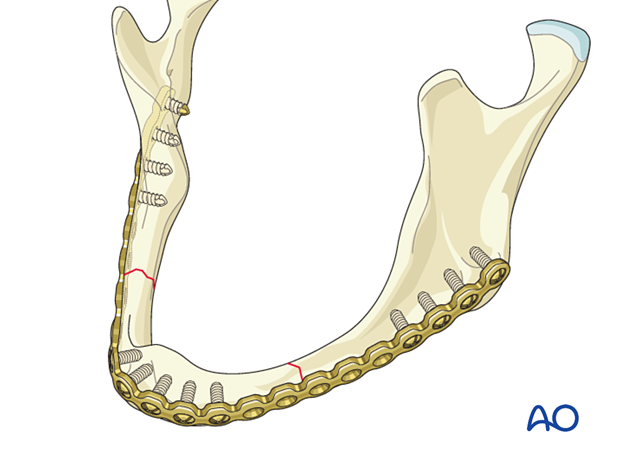
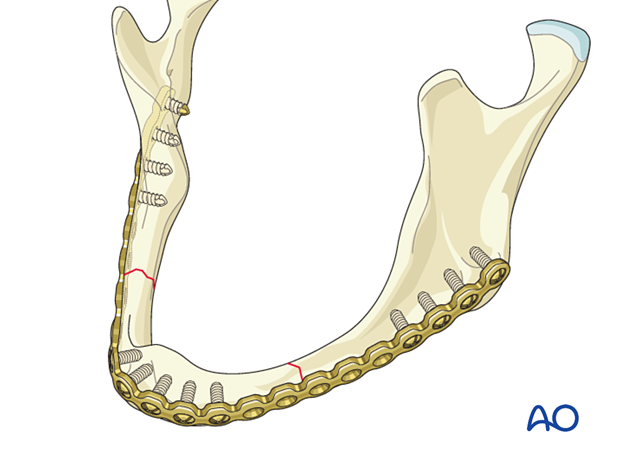
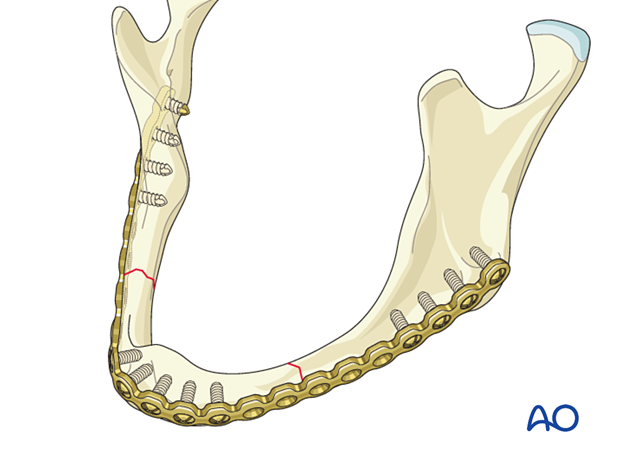
Load-bearing osteosynthesis is indicated in the treatment of the atrophic edentulous mandible fracture. Currently, it is recommended that load-bearing fixation is applied (2.4 mm locking reconstruction plate).
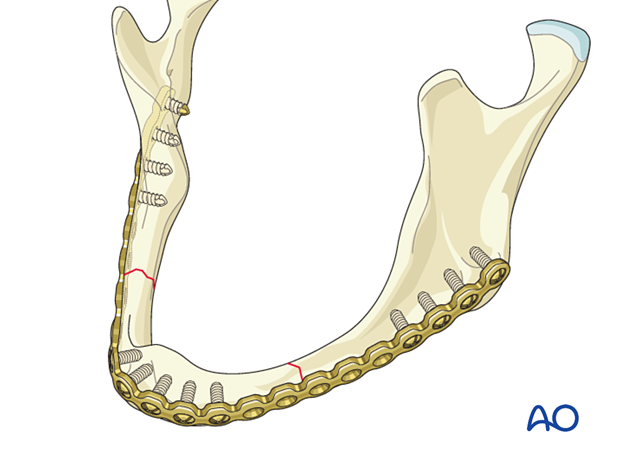
The plate must be of sufficient length to place screws in adequate bone, generally found in the symphysis and angle regions. Fractures commonly occur in the mandibular body, which typically has a bone of lower quality unsuitable for screw placement.
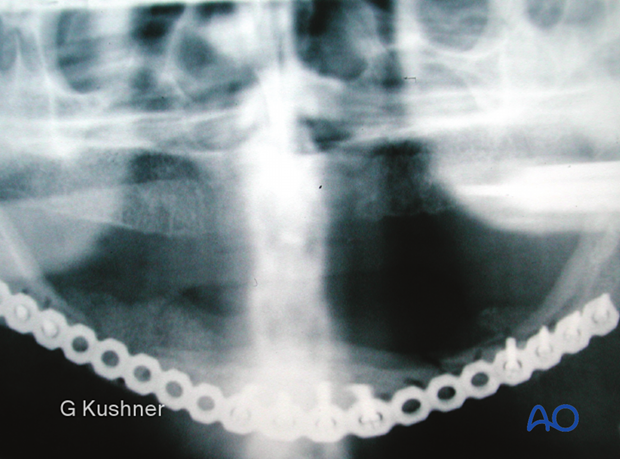
When dealing with bilateral fractures, the plate must span from angle to angle, covering the mandible's entire lateral surface.
At least three screws on each side of the fracture are recommended. Often more screws are necessary due to the low quality of the bone.
The locking reconstruction plate is generally left in place and not removed unless clinical symptoms require hardware removal.
Pitfall: insufficiently stable osteosynthesis
It may be tempting to use small plates when treating fractures in an atrophic "small" jaw. However, plate fracture and displacement are very common secondary to the muscle pull involved in the atrophic edentulous mandible when using small plates.
It is recommended that the smaller the jaw, the larger the bone plate.
This X-ray shows fractured plates and fracture displacement.
Alternatives to the locking reconstruction plate 2.4
There are fractures involving the edentulous mandibles, which are not atrophic in nature (> 20 mm in height). When there is sufficient bone to buttress the fracture and provide adequate healing, the surgeon may choose to use a smaller plate.
The 2.0 locking plate system (large or extra-large profile) provides all the advantages of the 2.4 locking reconstruction plate but has a smaller profile. Many surgeons have successfully used the 2.0 locking system on edentulous but not severely atrophic mandibles.
Templating
It is common to use large reconstruction plates that span from angle to angle. By using a template, the bending process is facilitated.
Bending
This clinical image shows the template and the reconstruction plate bent accordingly.

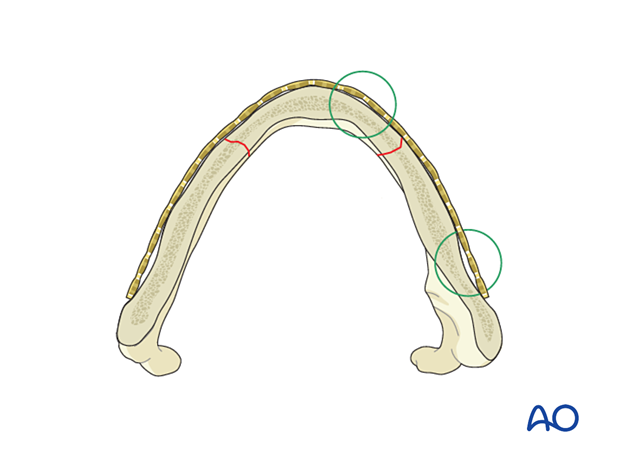
Perfect adaptation not needed
Perfect adaptation of the plate is not required (see green circles) as the 2.4 locking reconstruction plate acts as an "internal-external fixator."
If non-locking screws are used, perfect adaptation is needed. Otherwise, the reduction will be lost during the fixation.
7. Fixation
General considerations
The 2.4 locking reconstruction plate is fixed to the native mandible using either 2.4 mm or 3.0 mm screws. At least three screws must be present on each side of each fracture. In the atrophic edentulous mandible fracture, the screws are generally placed in the symphyseal region and the angular region.
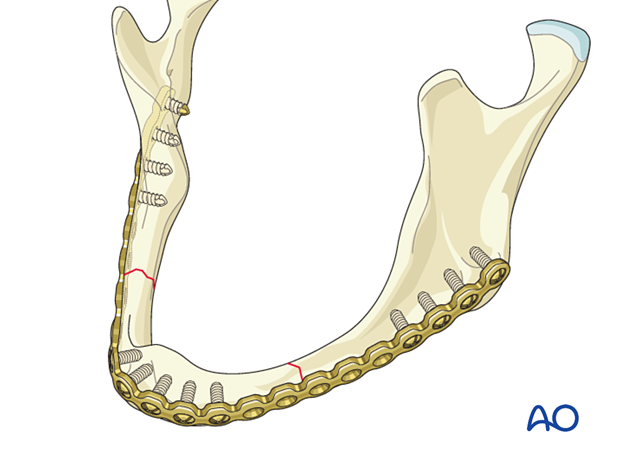
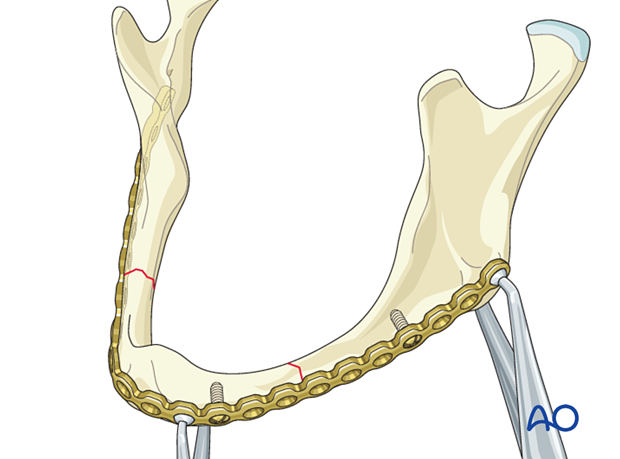
Plate application
Apply the plate and stabilize it either with digital pressure or plate-holding forceps.
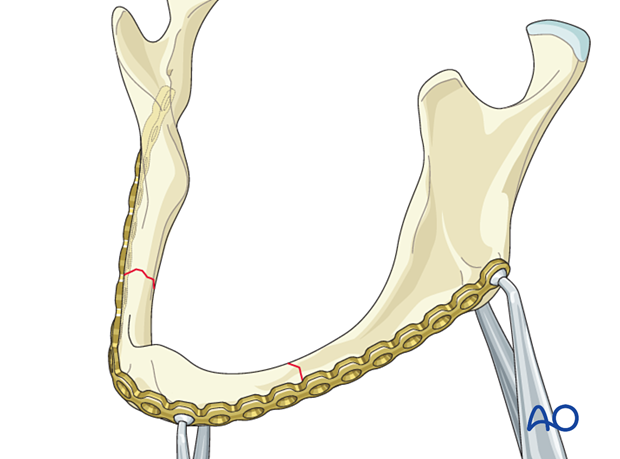
Placement of first screws
Place one screw on each side of each fracture in the planned holes closest to the fracture(s).
Click here for a detailed description of screw insertion in a reconstruction plate.
Copious irrigation must be applied to cool the bone.
Additional screw placement
The remaining screws are inserted to ensure stability across the fracture lines (at least three screws in each segment).
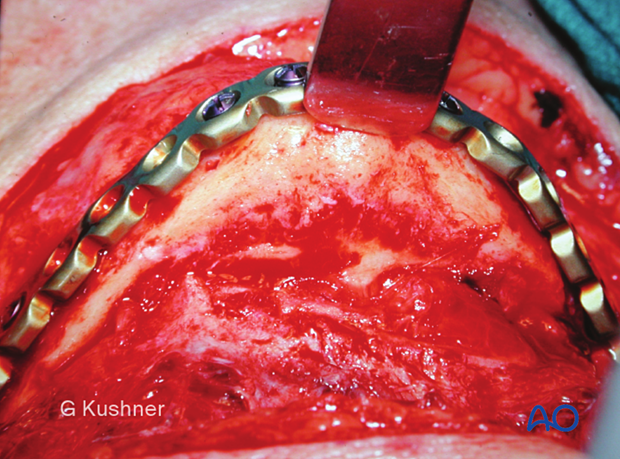
This clinical image shows the plate fixed to the mandible.
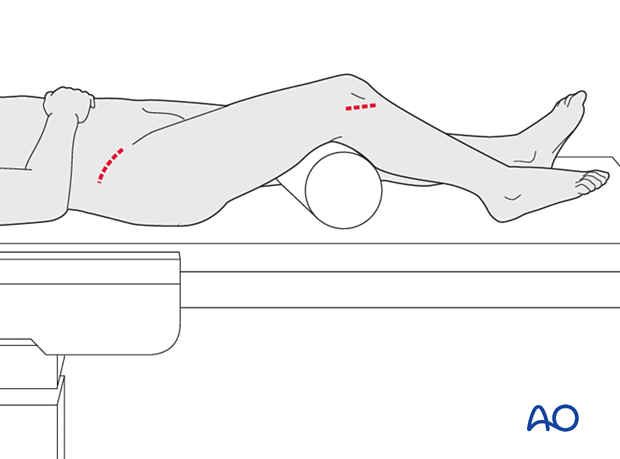
Harvesting of bone graft
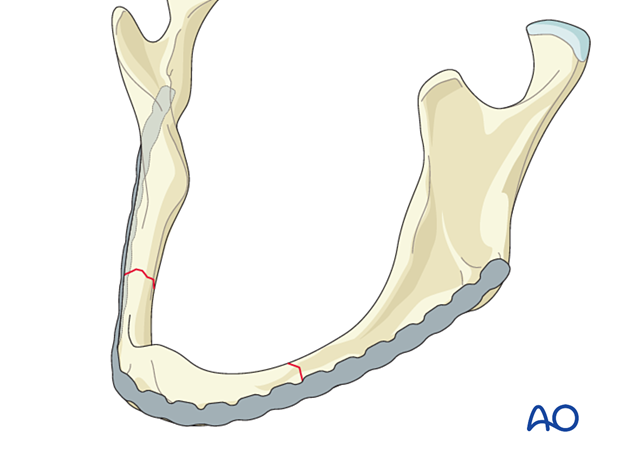
Due to the bone's poor healing quality, an autogenous bone graft is sometimes used to facilitate bony union. Common sites of bone graft harvest include the iliac crest or tibia.
The use of bone marrow aspirate concentrates, and bone morphogenetic protein may be useful to obviate the need for harvesting an autogenous bone graft.
Bone graft application
Autogenous cancellous bone graft has been added to fracture sites.
Completed osteosynthesis
X-ray shows the completed treatment.
8. Aftercare following treatment of an edentulous atrophic body fracture with a reconstruction plate
X-Rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken after 4–6 weeks.
Follow up
The patient is examined approximately one week postoperatively and periodically afterward to assess the fracture's stability and to check for infection of the surgical wound. Follow-up appointments are at the surgeon's discretion and depend on the mandible's stability on the first visit. Weekly appointments are recommended for the first four postoperative weeks.
Basic postoperative instructions
DietDepending upon the internal fixation's stability, the diet can vary between liquid and semi-liquid to "as tolerated," at the surgeon's discretion.
Patients with only extraoral approaches are not compromised in their routine oral hygiene measures and should continue with their daily schedules.
Patients with intraoral wounds must be instructed in appropriate oral hygiene procedures. Chlorhexidine oral rinses should be prescribed if the patient is not allergic to chlorhexidine and used at least three times each day to sanitize the mouth. For larger debris, a 1:1 mixture of hydrogen peroxide (0.25%) /chlorhexidine (0.12%) can be used. The bubbling action of the hydrogen peroxide helps remove debris.
Long-term dental rehabilitation
An existing dental prosthesis (denture) must often be remade. Dental implants may be placed in the anterior mandible. However, some of the locking plate screws may require removal to prevent interference with dental implant insertion. Implant reconstruction is undertaken when a bony union of the mandible has been achieved.