Transoral approach to the symphysis and body
1. Principles
Vestibular incisions
The transoral approach is the usual access for simple fractures of the body, symphysis, and angle regions.
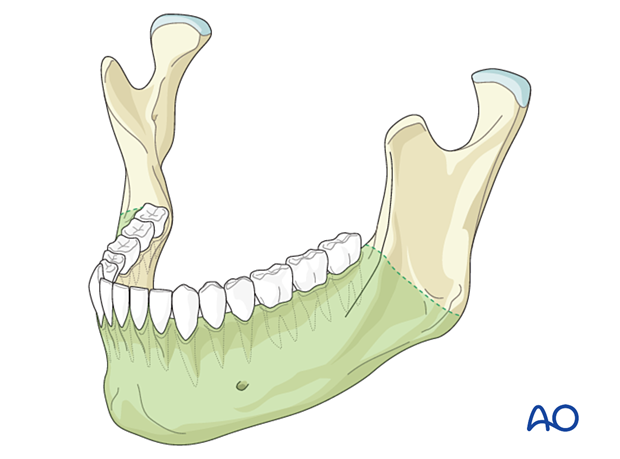
The approach can be extended posteriorly (dashed line) to better access the posterior body, angle, and ramus regions.
In complex fractures, including comminuted, edentulous, and avulsive fractures requiring the placement of load-bearing reconstruction plates, a transfacial approach may provide better access.
Oral contamination is not a contraindication for a transoral incision.
Neurovascular structures
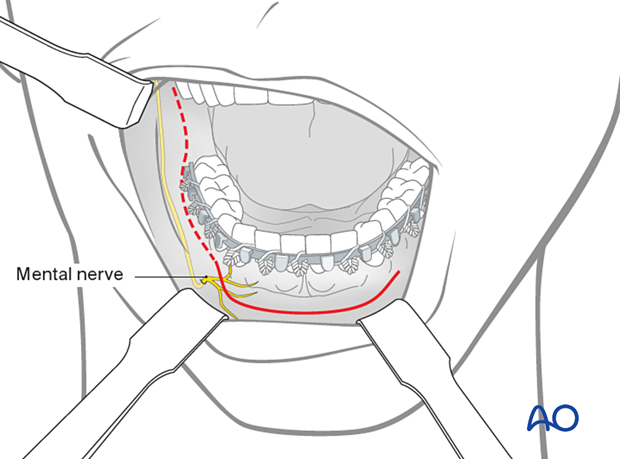
The mental nerve is a branch of the fifth cranial nerve (trigeminal nerve). This nerve provides sensation to the anterior mandibular vestibule, lip, and chin.
When the incision is extended posterior to the canine teeth, the mental nerve can be damaged. Therefore, keep the incision superior to the mental nerve in the body region.
Particularly in the extended transoral approach, care must be taken to protect the mental nerve in the anterior body region.
2. Transoral incision
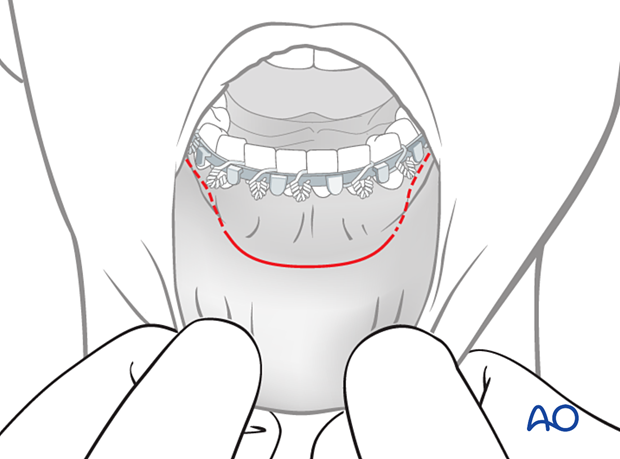
Mucosal incision
Unless contraindicated, infiltrate the area with a local anesthetic containing a vasoconstrictor.
Make an incision through the mucosa in the vestibule. The incision between the canines is made 10–15 mm away from the attached gingiva in a curvilinear fashion. Posterior to the canine, the incision is only 5 mm away from the attached gingiva, staying superior to the mental nerve.
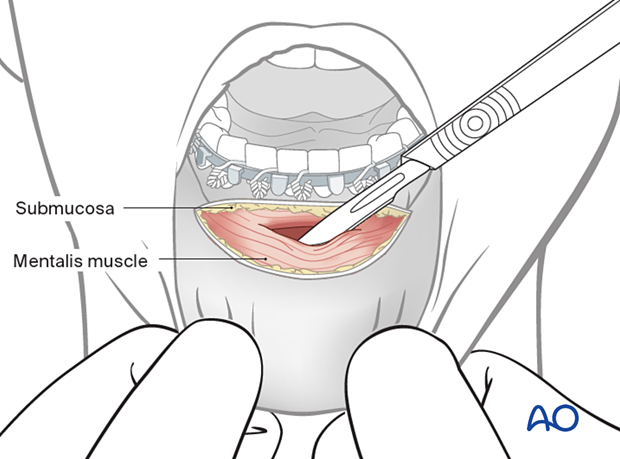
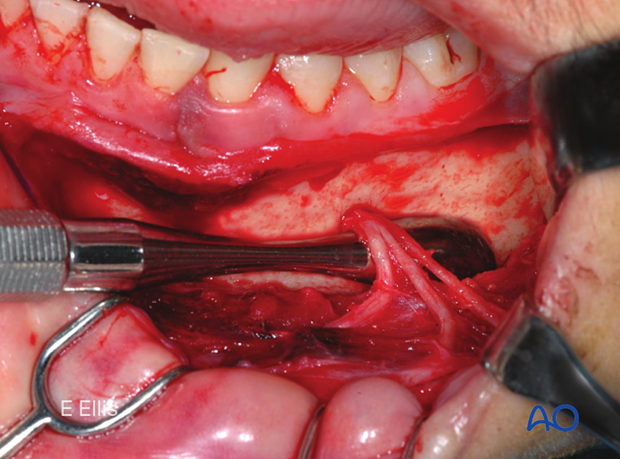
Surgical flap dissection
Carry the incision through the mucosal layer in the anterior region out into the lip away from the vestibular fold.
Perform a submucosal dissection to expose the mentalis muscle's surface. The mental nerve branches are located just underneath the mucosal flap and must be identified and protected.
The mentalis muscle is bisected, leaving enough muscle at the alveolar edge (cephalad), creating a stepwise approach that protects the mental nerve. Later, during wound closure, the mentalis muscle should be appropriately reattached.
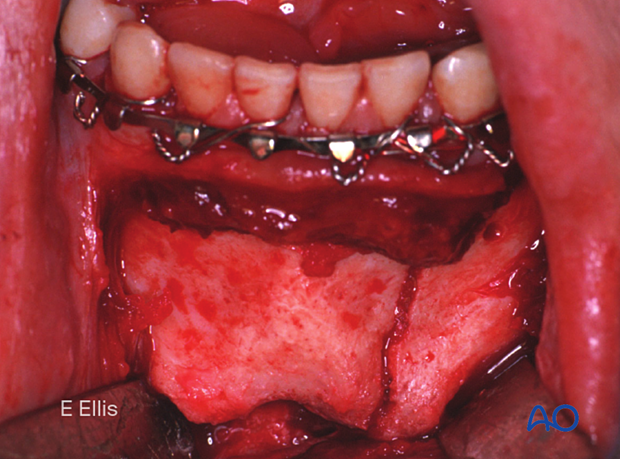
Fracture site exposure
Elevate a mucoperiosteal flap to expose the fracture.
3. Extension of approach
Lateral/posterior vestibular incision
The approach can be extended laterally and posteriorly to access the mandible's body, angle, and ramus regions.
Right-angled retractors are helpful to expose this area.
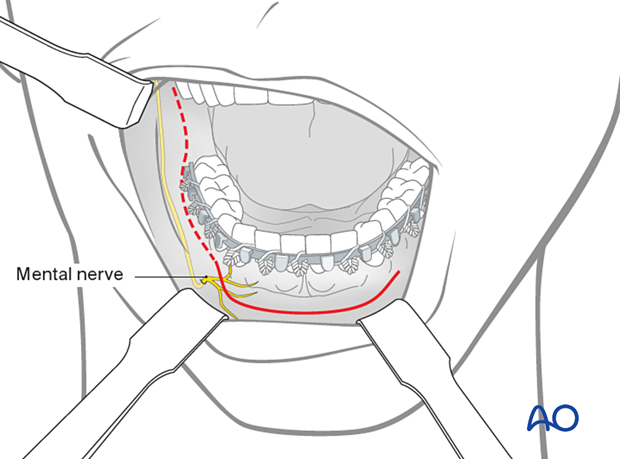
Dissection of the mental nerve
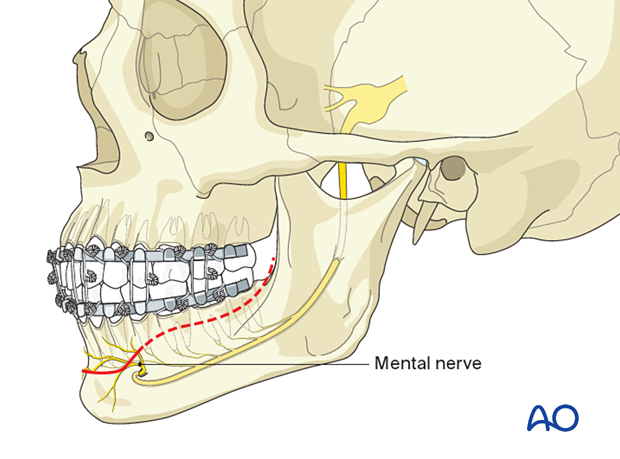
In the extended transoral approach, care must be taken to protect the trunk of the mental nerve, which exits in the anterior body region.
In the sagittal plane, the mental foramen is located at a level projecting between the first and second premolar apices.
Keep the incision superior to the mental nerve trunk.
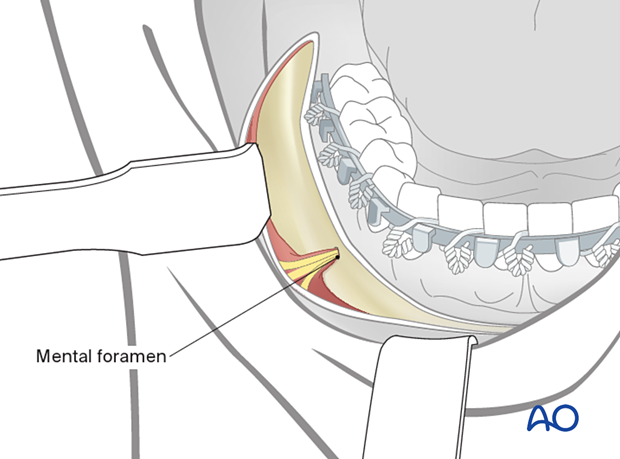
Freeing of the mental nerve allows for better soft-tissue retraction.
Tissue scissors are used to cut the periosteal sheath. Blunt dissection in a direction parallel to the nerve will allow for further retraction of the mucoperiosteal flap. Scalpels could be used but at the risk of injuring the nerve.
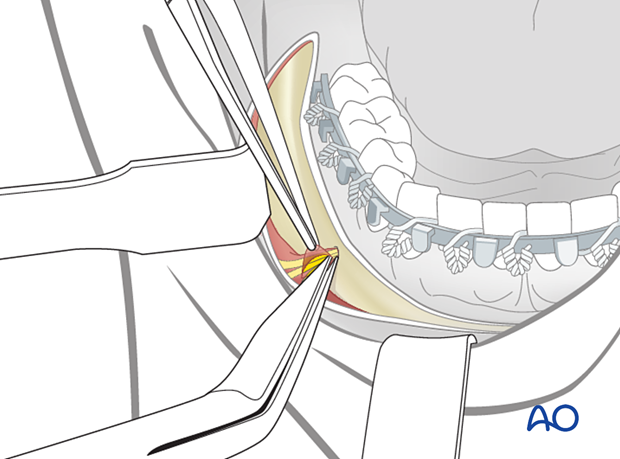
The mental foramen and mental nerves are exposed.
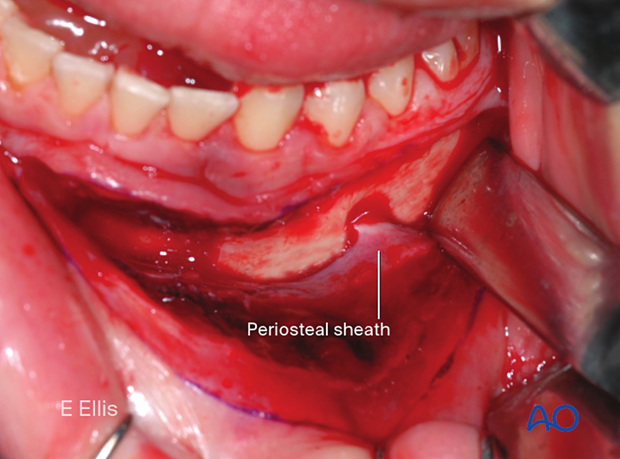
The soft-tissue envelope is released by incising the periosteal sheath and spreading the scissors parallel to the nerve (blunt dissection).
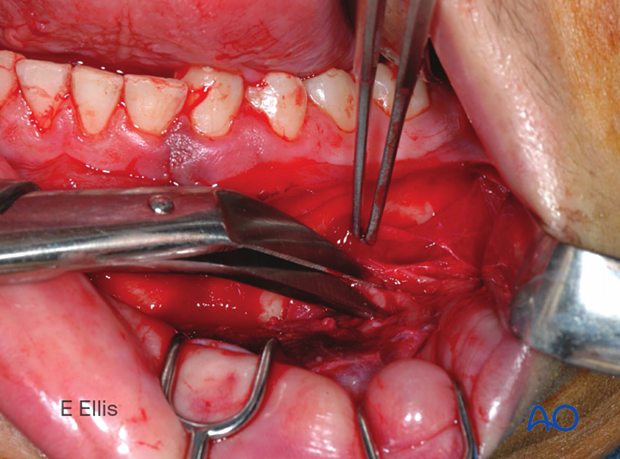
This image shows the skeletonization of the mental nerve.
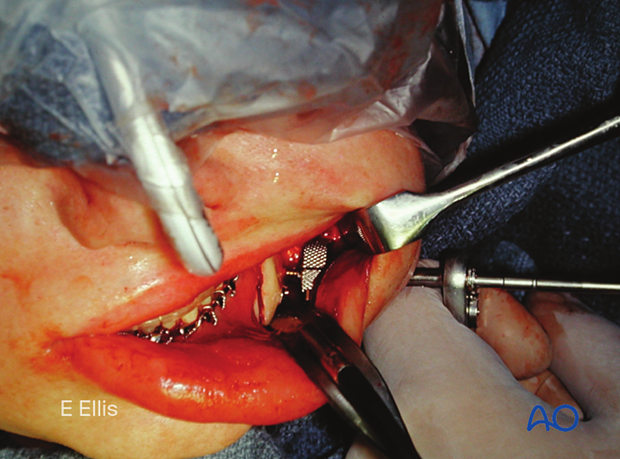
4. Combination with the transbuccal technique
The transbuccal trocar may assist the surgeon in
- inserting screws in the posterior region.
- minimizing mental nerve retraction.
- keeping the screws perpendicular to the plate.
Detailed description of the transbuccal technique.
5. Wound closure
After thoroughly irrigating the wound with saline solution and checking for hemostasis, the incision is closed. Anteriorly, the mentalis muscle is reapproximated to prevent drooping of the chin (ptosis). The mucosa is closed with interrupted or running resorbable or non-resorbable sutures.
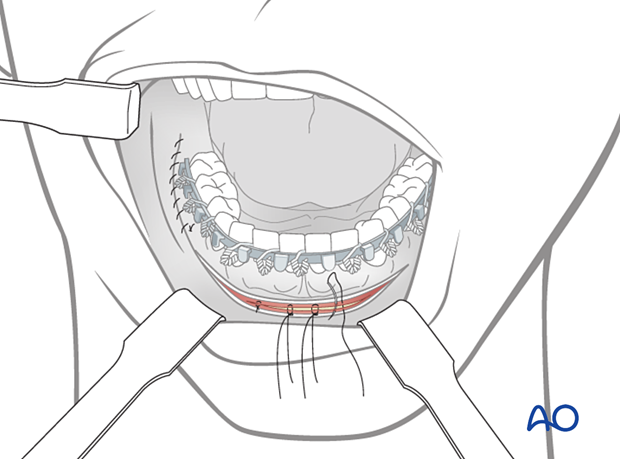
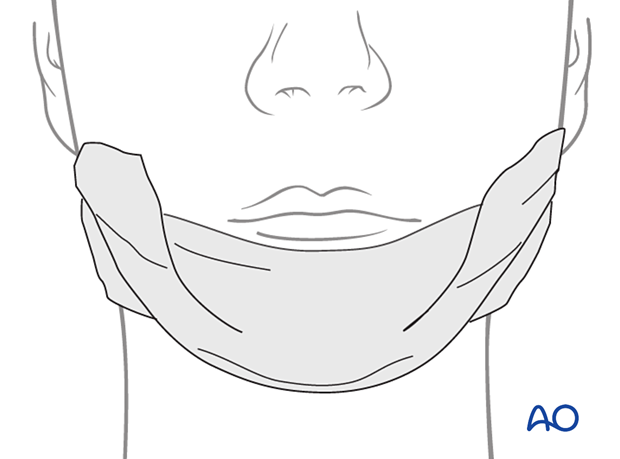
An elastic pressure dressing on the chin region helps support the soft tissues and prevent hematoma formation.