Complications
1. General considerations
The mandible is the only facial bone that is movable. The results of mandibular fracture treatments are easily measurable. Unfortunately, there is a relatively high complication rate when dealing with mandible fractures.
The most common complications following mandibular fracture treatment are:
- Nonunion
- Malunion
- Malocclusion
- Ankylosis
- Infection
- Hardware failure
While hardware failure is covered below, all other complications are covered in the complications section.
2. Fixation failure
General consideration
Fixation failure results in fracture mobility that can subsequently lead to infection, nonunion, and/or malunion.
Fixation can fail by several mechanisms, which include:
- Insufficient amount of fixation
- Fracture of the plate
- Loosening of the screws
- Devitalization of bone around screws

Insufficient amount of fixation
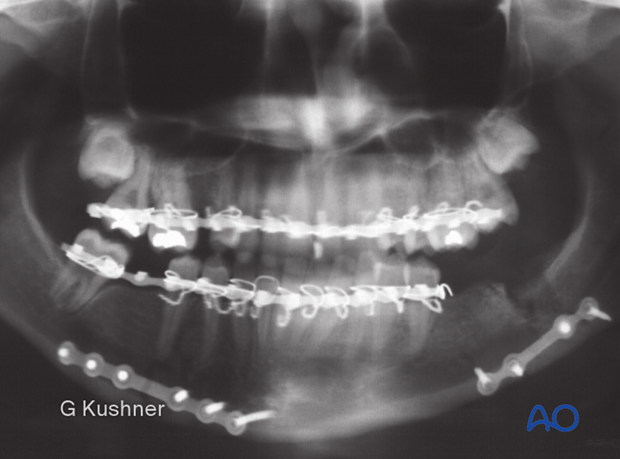
Left mandibular angle fracture was treated using a malleable 2.0 miniplate at the inferior border of the mandible. This fixation is insufficient for this fracture. The patient now has mobilty (non-union) and infection 6 weeks after treatment.
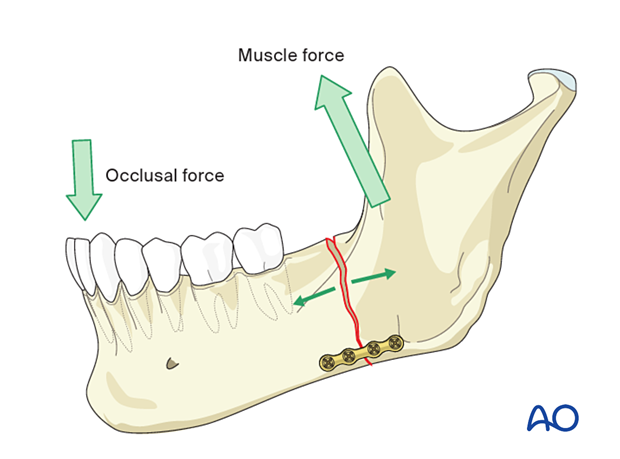
This illustration demonstrates the biomechanics of an angle fracture. A small plate applied at the inferior border provides insufficient stability as it cannot prevent a gap from opening at the superior surface of the mandible under function.
The patient developed an infection of the left angle fracture site. The patient was taken back to the operating room and stable load bearing fixation was applied. Subsequently, the fracture healed.

Fracture of the plate
X-ray shows a superior border miniplate.
This clinical situation (edentulous mandible at the fracture site, impacted third molar) is biomechanically demanding and not suitable for one miniplate osteosynthesis.
This X-ray shows the fractured plate. Segments were mobile, which required ORIF with a 2.4 locking reconstruction plate.

Loosening of screws
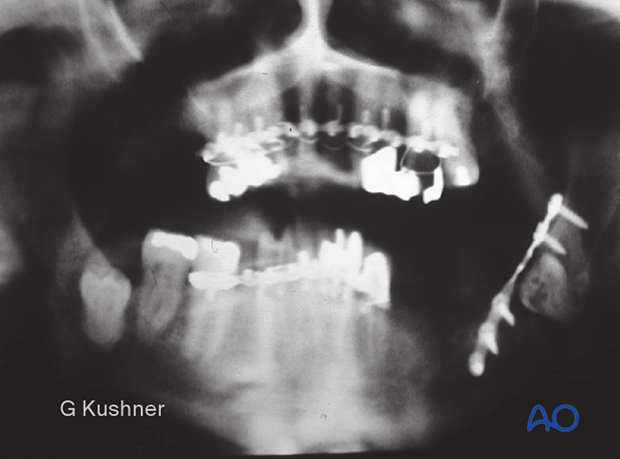
Four weeks after fixation of the right angle using two miniplates, the patient presents with a draining sinus tract through the skin.

X-ray shows at least one loose screw and loss of stability. This fracture is now an infected defect fracture requiring rigid load bearing fixation.
The patient was taken back to surgery, where a reconstruction plate was applied.
Devitalization of bone around screws
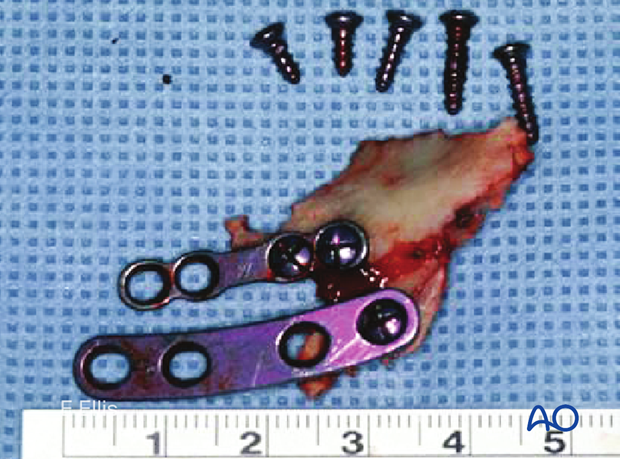
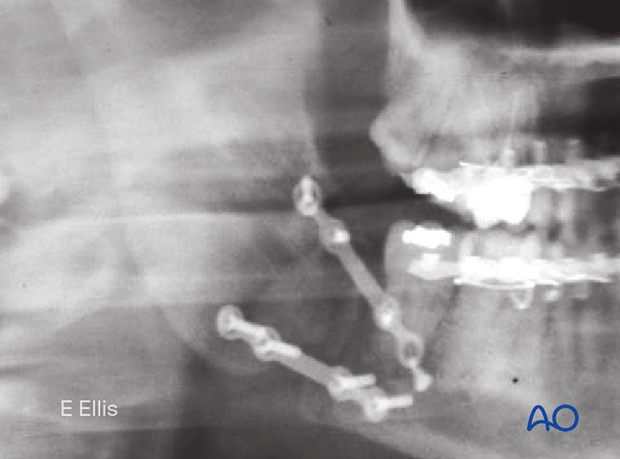
Six weeks after treatment of right angle and left body fractures with two compression plates, the patient presents with swelling. Panoramic x-ray shows loose hardware on the right side.

The fracture was opened, and hardware was still attached to portions of the buccal cortex, which was devitalized and had sequestered.
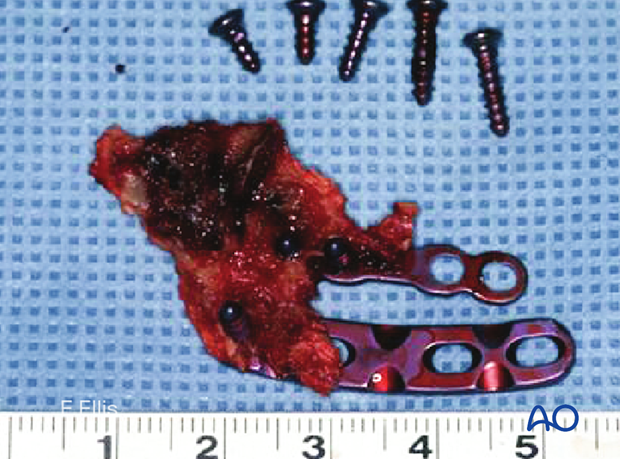
Fortunately, the lingual cortex had healed, and the occlusion was normal. Thus, no further treatment was necessary.