Submandibular approach
1. Introduction
This approach is selected for fractures of the mandibular body and angle regions unsuitable for intraoral treatment.
This applies to more difficult fracture patterns such as comminuted, atrophic, and defect fractures to allow optimal manipulation of the fragments, good control of the lingual cortex and inferior border, and the application of the internal fixation hardware.
Some have used this approach for treatment of sub condylar fractures.
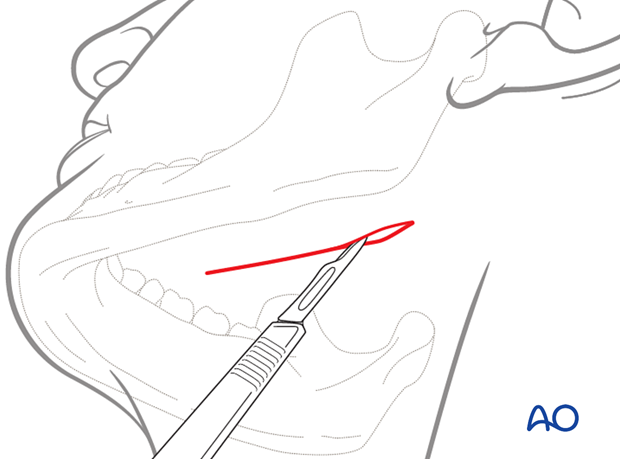
The incision can either be parallel to the inferior border of the mandible (A) or be placed in an existing skin crease (B) for maximum cosmetic benefit.
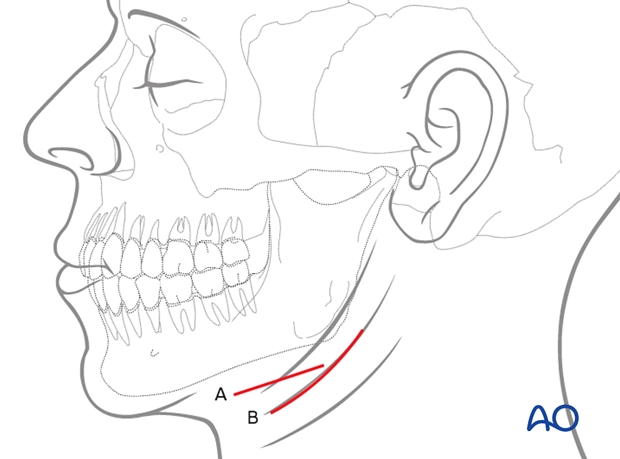
If using skin creases for the incision the orientation of the scalpel blade is parallel to the relaxed skin tension lines (RSTL).
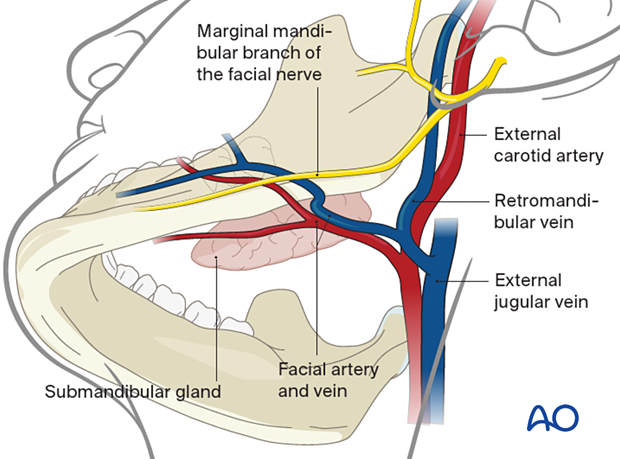
Neurovascular structures
The main neural structure is the marginal mandibular branch of the facial nerve (CN VII). The facial artery and vein can also be encountered during this dissection.
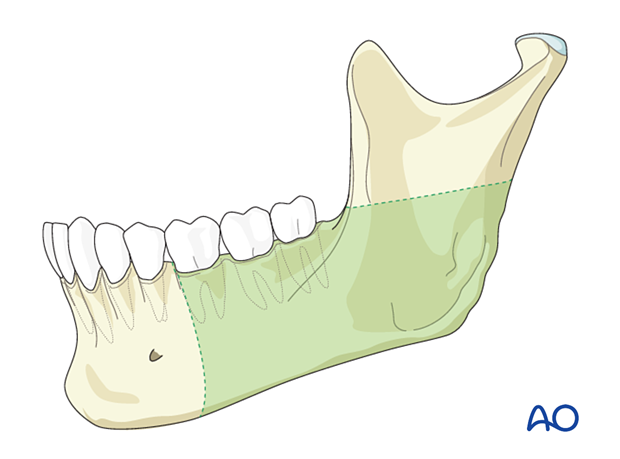
Exposure
Exposure offered by the submandibular approach.
2. Skin incision
Use of local anesthetic and vasoconstrictors
Use of a solution containing vasoconstrictors ensures hemostasis at the surgical site. The two options currently available are the use of local anesthetic or a physiologic solution with vasoconstrictor alone.
Use of a local anesthetic with vasoconstrictor may impair the function of the facial nerve and impede the use of a nerve stimulator during the surgical procedure. Therefore, consideration should be given to using a physiological solution with vasoconstrictor alone or injecting the local anesthetic with vasoconstrictor very superficially.
Muscle relaxants used in general anesthesia can also impair nerve function and must be avoided.
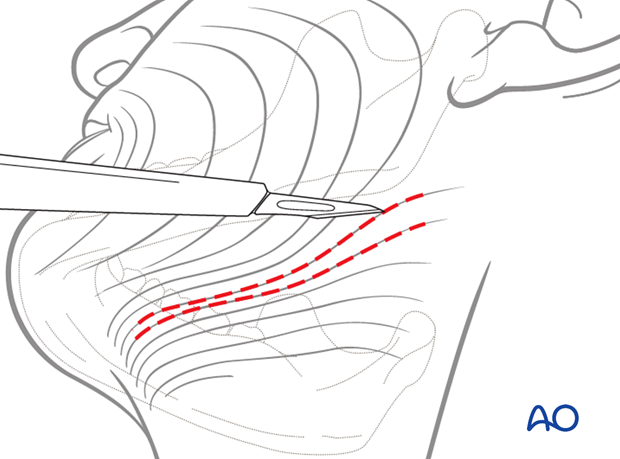
The length of the incision depends on fracture extension and the planned internal fixation technique. The diagram shows a skin incision 2-3 cm below the inferior border of the mandible. Incision of skin and subcutaneous tissues exposes the underlying platysma muscle.
3. Dissection
In order to protect the marginal mandibular branch of the facial nerve, the platysma is undermined bluntly with scissors prior to dividing it with a scalpel.
The platysma muscle is divided sharply, preferably 2-3 cm below the mandibular border, not necessarily at the same level of the skin incision.
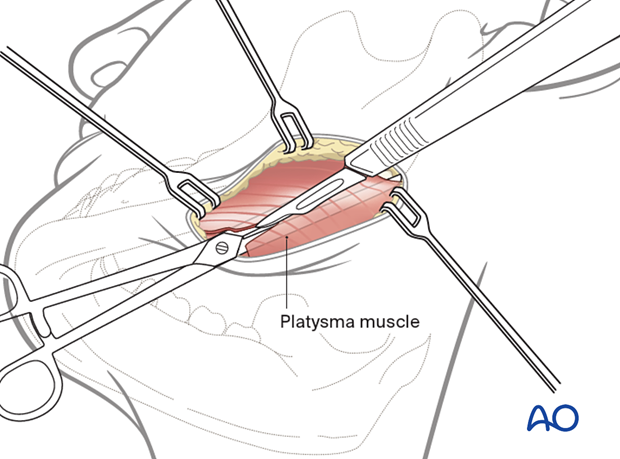
Superior subplatysmal dissection would expose the underlying marginal mandibular branch of the facial nerve (CN VII). This is not usually necessary.
A subfascial (superficial layer of the deep cervical fascia), supraglandular dissection avoids exposure of the nerve.
If ligation of the facial artery and vein is necessary, the retraction of the vessels superiorly protects the marginal mandibular branch of the facial nerve, which usually lays superficial to the facial vein.
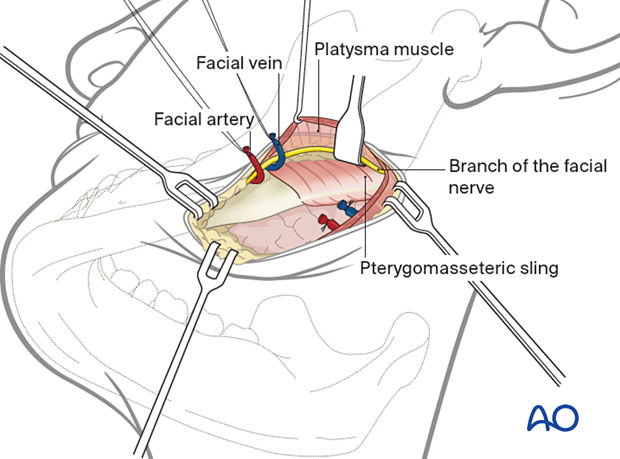
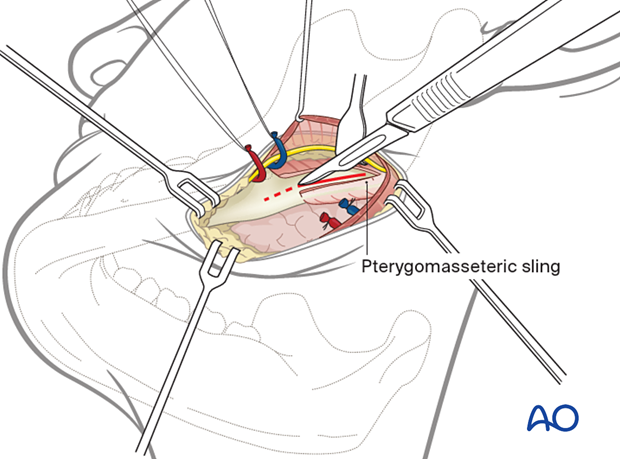
4. Exposure
Divide the pterygomasseteric sling and incise the periosteum at the inferior border to expose the ramus.
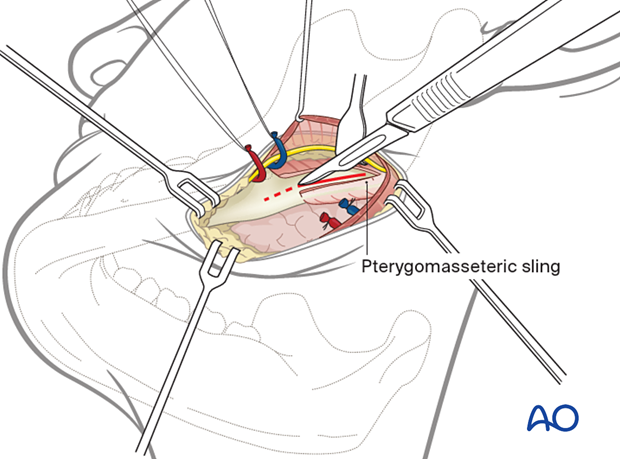
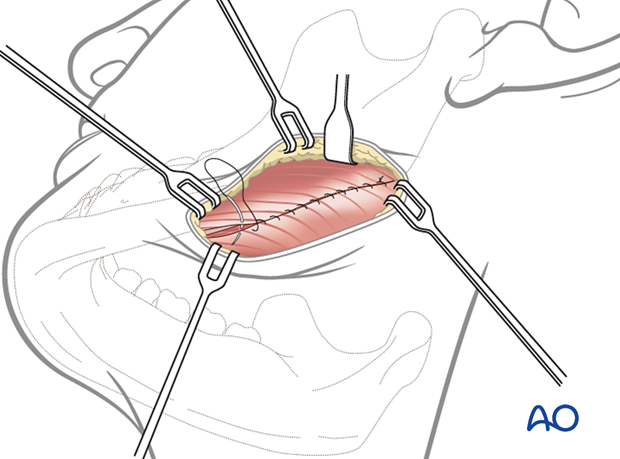
5. Wound closure
During wound closure, the pterygomasseteric sling is repaired.

The wound is then closed in layers to realign the anatomic structures and eliminate dead space. The platysma muscle is repaired. A variety of skin closure techniques are available based on surgical preference. A drain may be used if necessary.