ORIF, load bearing plate
1. Principles
The different use scenarios
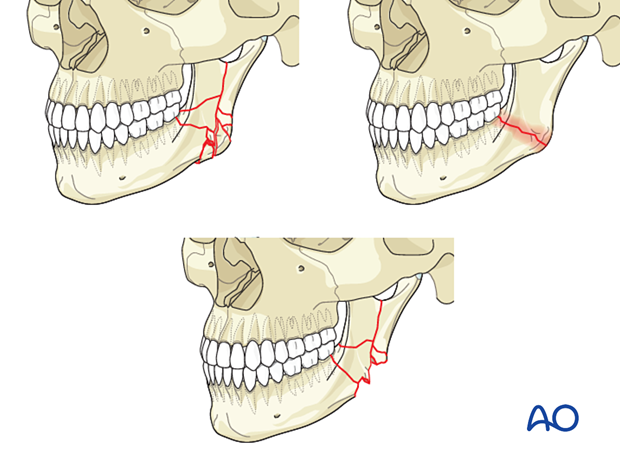
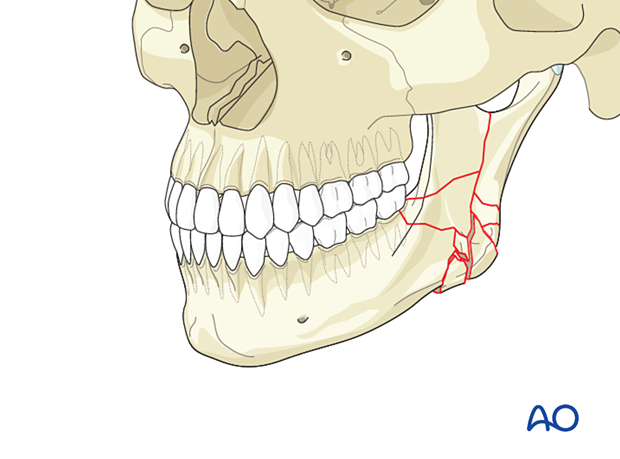
Load-bearing fixation is indicated for open surgical treatment in all types of complex fractures in the mandibular angle (comminuted or simple chronically infected fractures, defects).
- A detailed discussion of load-bearing versus load-sharing fixation
Further information on the fixation of chronically infected fractures with or without bone loss can be found here.
If a reconstruction plate is used because of a history of infection, the mandible's infected area should be spanned without using screws within that area. The placement of at least three screws in the uninvolved bone on each side of the fracture is required.
Although there is a risk of subsequent infection, sequestration, or bone loss, ORIF is the treatment of choice for comminuted fractures.
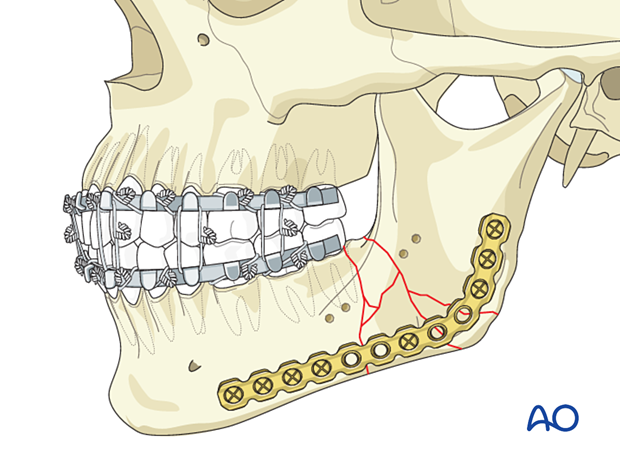
The load-bearing fixation bridges the area of comminution. The bone fragments within the comminuted area will usually not provide support to the construct. The reconstruction plate should be fixed with at least three, preferably four screws on each side of the comminuted area.
To illustrate the principles, the remainder of this procedure will focus on comminuted fractures.
Keys to success
The keys to a successful result are:
- Fracture simplification with adequate three-dimensional fragment reduction and fixation
- Proper alignment of the alveolar segments to restore preoperative occlusion
- Well-adapted reconstruction plate, bridging the fracture gap and restore the continuity of the mandbile
Other considerations
Following special considerations may need to be taken into account:
Click on any subject for further detail.
2. Fixation of comminuted fractures
Stepwise repair: simplification before load-bearing reconstruction
When treating comminuted mandibular body fractures, the surgeon should proceed in a stepwise fashion:
- Expose the fracture and remove indicated teeth
- Reduce the fracture, restore occlusion, and secure MMF
- Simplify comminuted fractures using miniplates
- Perform the load-bearing fixation
When simplification is performed, small fragments within a comminuted area are reduced and fixed to each other to build up larger bone compounds that will fit into the gap. These bone components are used to realign the overall bone shape and help to contour the reconstruction plate along the realigned lower mandibular border.
The use of one long plate spanning the entire superior segment would provide more stability than several smaller plates.
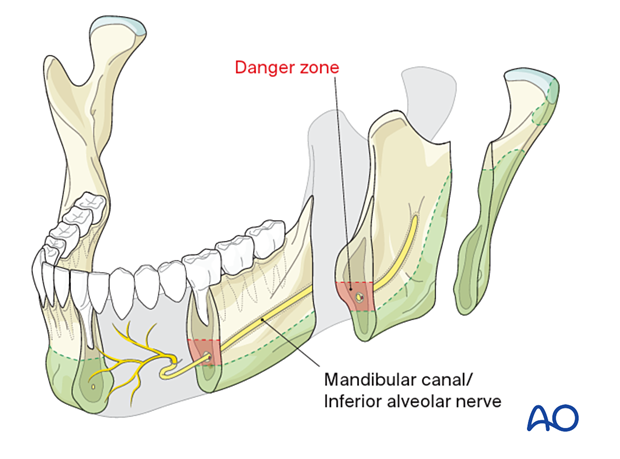
Zones for screw placement in the mandible
Two structures must not be harmed by screw insertion:
- the mandibular canal with the inferior alveolar nerve
- the tooth roots.
The ideal location for bicortical screw placement is along the inferior mandibular border (green). Monocortical screws should be used above the mandibular canal, still trying to avoid the root tips.
3. Patient preparation
This procedure is typically performed with the patient placed in a supine position.
4. Approach
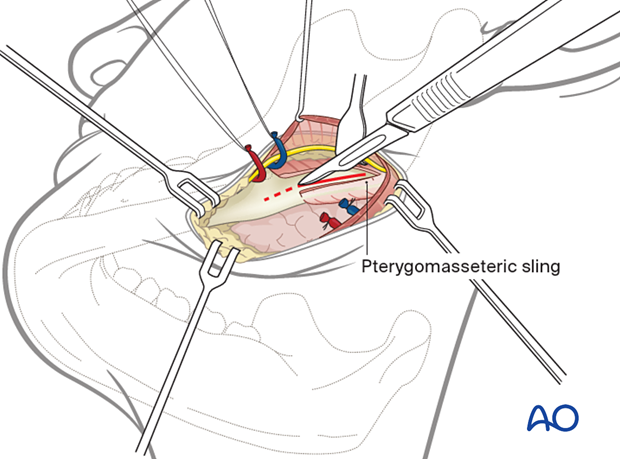
For complex fractures of the mandibular angle, the transoral approach to the angle can be selected by those surgeons experienced in the technique of placing a large plate at the inferior border of the mandible using transbuccal trocar instrumentation or an angulated screwdriver.
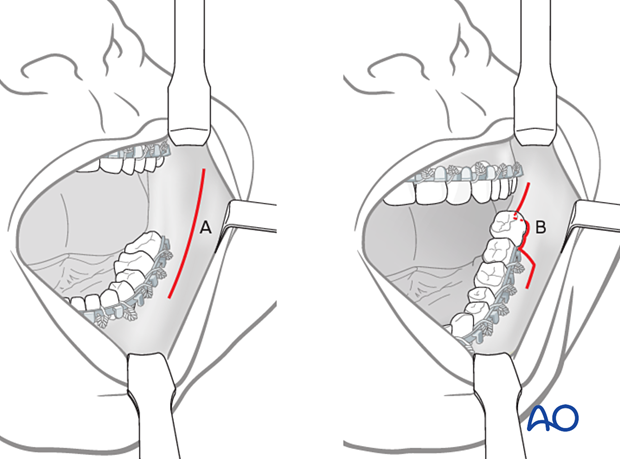
Incision A (vestibular incision) can be used when there is no third molar present, or when there is an unerupted third molar that may or may not require removal.
Incision B is used when there is an erupted third molar that must be removed during surgery. Incision B allows the development of a buccal mucoperiosteal flap that can be advanced to cover the extraction socket.
However, a transcutaneous approach (the submandibular approach) is often chosen because this access provides a better access. Existing lacerations may also be used.
5. Reduction
Tooth removal (if indicated)
Once the fracture has been exposed, teeth can be extracted if indicated.
Reduction
Forceps may be used to manipulate the mandibular fragments into proper reduction.
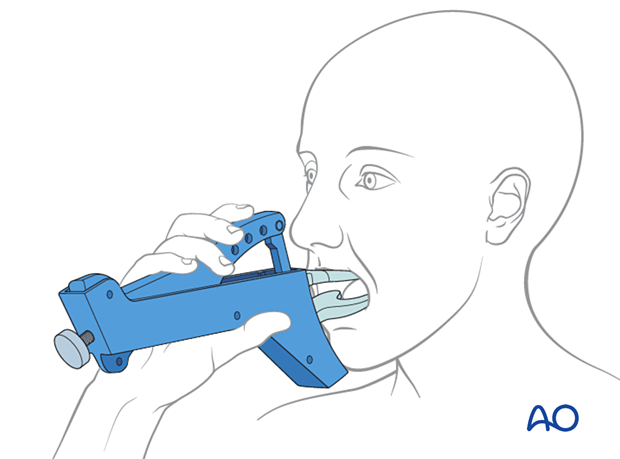
MMF
6. Fixation
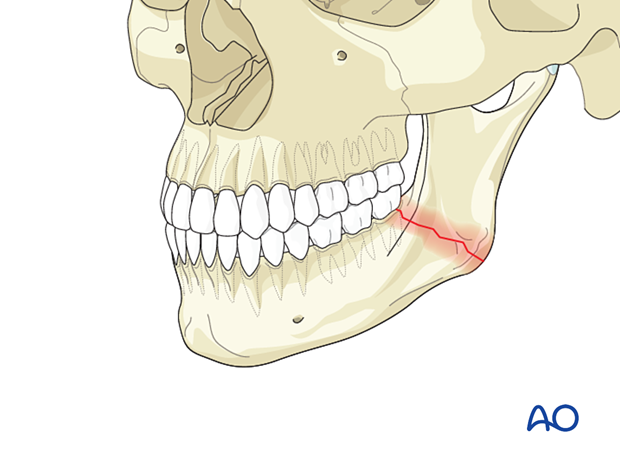
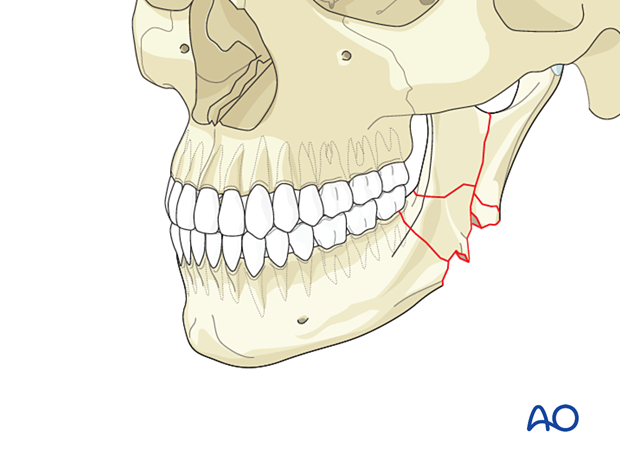
Simplification of the fracture
Temporary/initial fixation of mandibular fragments can be accomplished using small plates and screws applied in locations that will not interfere with the reconstruction plate.
The condyle fragment must be positioned appropriately and maintained in place during the application of the reconstruction plate.
The small plate(s) may be left in place or may be removed after the placement of the reconstruction plate
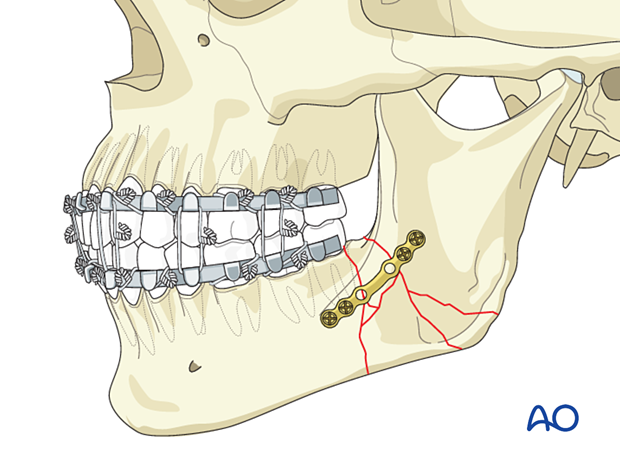
Plate selection
For load-bearing fixation, a 2.4 reconstruction plate should be used. The plate must be long enough to insert a minimum of three or preferably four screws into each stable fragment. Pre-angled reconstruction plates may be necessary to provide an adequate number of screw holes. There are several advantages to using a locking reconstruction plate system.
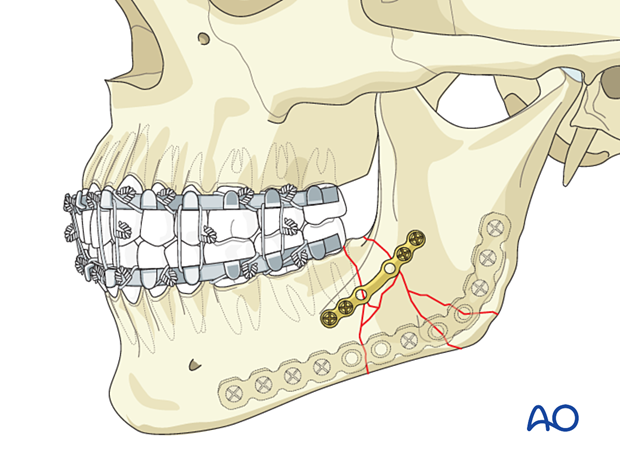
The plate must be contoured to the mandible's lateral surface, flush with the inferior and posterior borders to avoid injuring the inferior alveolar nerve.

Securing the plate to the bone with bone clamps
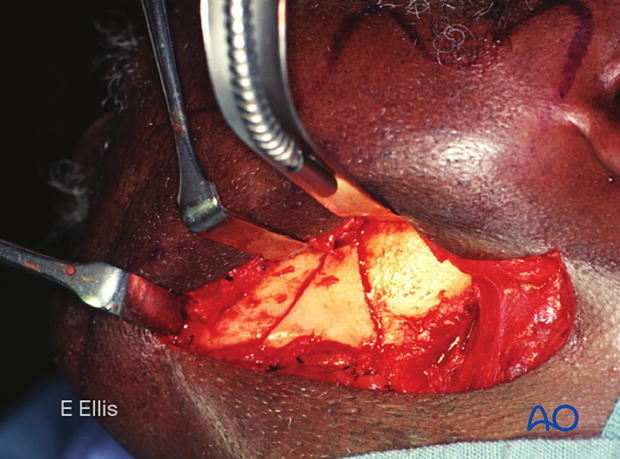
When using a transcutaneous approach, insert the properly contoured plate onto the mandible lateral surface and hold it there using ball pointed reduction forceps. Ideally, one set of forceps would be applied anterior, and one set posterior to the area of comminution.
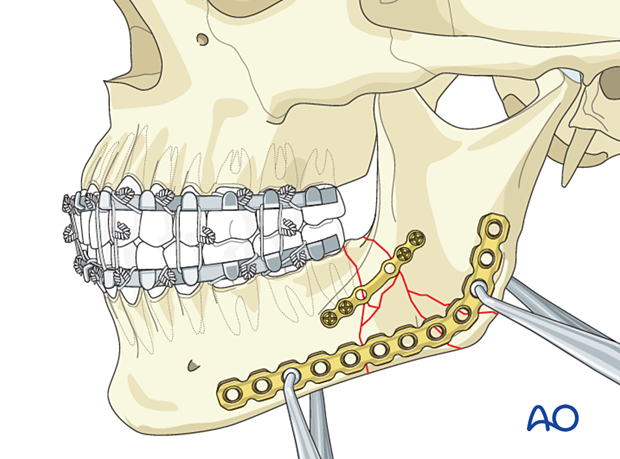
Inserting screws
The sequence of screw insertion is not important if the plate is securely clamped to the bone. Threaded drill guides should always be used to center the screw within the plate hole if one is using a locking screw/plate system.
Large fragments (like the triangular one in this photograph) can be secured to the reconstruction plate to hold them in position.
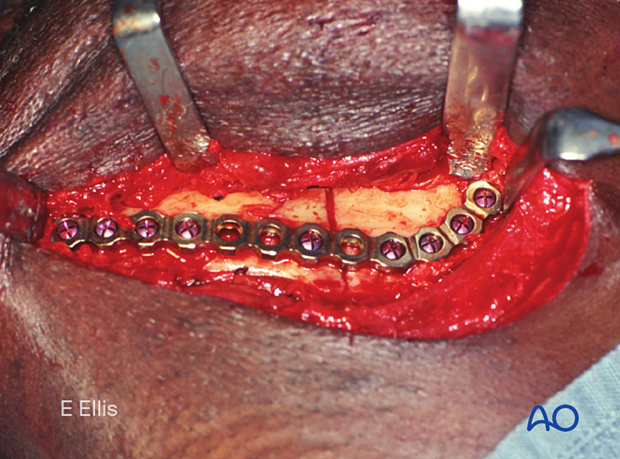
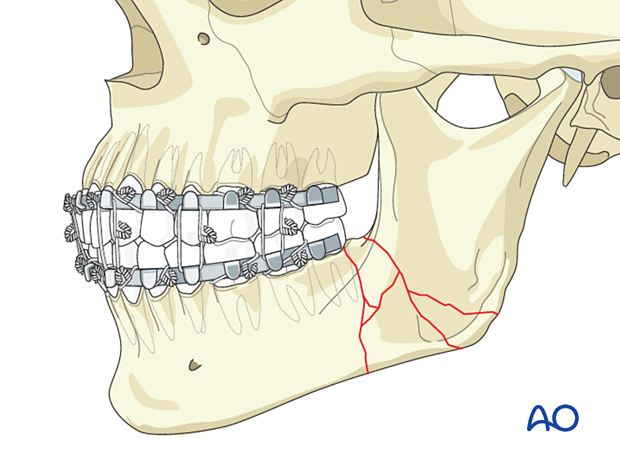
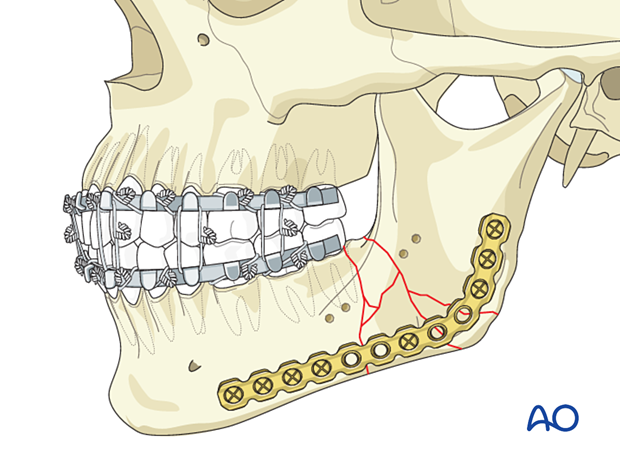
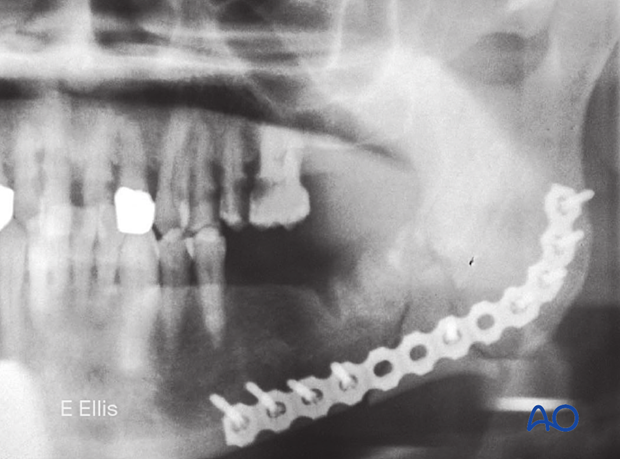
Completed osteosynthesis
This illustration shows the completed osteosynthesis after removing the simplification plate.
7. Final check
One should then release the MMF and check the occlusion for accuracy before proceeding with closure.
X-ray shows the completed osteosynthesis.
8. Aftercare following ORIF of mandibular symphysis, body, angle, and ramus fractures
Use of jaw bra
If significant degloving of the soft tissues of the mandible has occurred, there may be a consideration for using a jaw bra or similar support dressing.
Arch bars
If arch bars or MMF screws are used intraoperatively, they are usually removed at the conclusion of surgery if proper fracture reduction and fixation have been achieved. Arch bars may be maintained postoperatively if functional therapy is required or if required as part of the fixation.
X-Rays
Postoperative x-rays are taken within the first days after surgery. In an uneventful course, follow-up x-rays are taken after 4–6 weeks.
Follow up
The patient is examined approximately 1 week postoperatively and periodically thereafter to assess the stability of the occlusion and to check for infection of the surgical wound. During each visit, the surgeon must evaluate the patient's ability to perform adequate oral hygiene and wound care and provide additional instructions if necessary. Many patients need to be seen regularly for replacement of their intermaxillary elastics and to encourage range of motion in their TMJ in the later course of the treatment.
Follow-up appointments are at the discretion of the surgeon and depend on the stability of the occlusion on the first visit. If a malocclusion is noted and treatable with training elastics, weekly appointments are recommended.
The patient should be warned to continue routine follow up with their dentist. Fractures near the dental roots can often result in delayed loss of tooth viability, requiring periapical films and additional dental procedures.
Malocclusion
If a malocclusion is detected, the surgeon must ascertain its etiology (with appropriate imaging technique). If the malocclusion is secondary to surgical edema or muscle splinting, training elastics may be beneficial. The lightest elastics as possible are used for guidance, because active motion of the mandible is desirable. Patients should be shown how to place and remove the elastics using a hand mirror.
If the malocclusion is secondary to a bony problem due to inadequate reduction or hardware failure or displacement, elastic training will be of no benefit. The patient must return to the operating room for revision surgery.
Basic postoperative instructions
DietDepending upon the stability of the internal fixation, the diet can vary between liquid and semi-liquid to “as tolerated”, at the discretion of the surgeon. Any elastics are removed during eating.
Patients having only extraoral approaches are not compromised in their routine oral hygiene measures and should continue with their daily schedule.
Patients with intraoral wounds must be instructed in appropriate oral hygiene procedures. The presence of the arch-bars and any elastics makes this a more difficult procedure than normal. A soft toothbrush (dipping in warm water makes it softer) should be used to clean the surfaces of the teeth and arch-bars. Any elastics are removed for oral hygiene procedures. Chlorhexidine oral rinses should be prescribed and used at least three times each day to help sanitize the mouth. Chlorohexidine may cause staining of the teeth and should not be used longer than necessary. For larger debris, a 1:1 mixture of hydrogen peroxide (0.25%)/chlorhexidine (0.12%) can be used. The bubbling action of the hydrogen peroxide helps remove debris. A water flosser, providing a water jet, is a very useful tool to help remove debris from the wires. If a this is used, care should be taken not to direct the jet stream directly over intraoral incisions as this may lead to wound dehiscence.
Physiotherapy can be prescribed at the first visit and opening and excursive exercises begun as soon as possible. Goals should be set, and, typically, 40 mm of maximum interincisal jaw opening should be attained by 4 weeks postoperatively. If the patient cannot fully open his mouth, additional passive physical therapy may be required such as Therabite® or tongue-blade training.