Operative treatment
1. Introduction
Before proceeding with definitive repairs, the patient must be fully resuscitated, fully evaluated, and fit for anesthesia and surgery by a prepared team.
Successful definitive treatment requires reduction and fixation of both the posterior and anterior injuries, generally completed in a single definitive procedure.
Complete pelvic ring instability may be obvious when displacement is gross, but it may also be occult, when initial displacement has been hidden by elastic recoil, poor imaging studies, or successful reduction by a pelvic binder.
This illustration shows inlet and outlet oblique views, with posterior and proximal translational displacement of a right sacro iliac fracture dislocation, with associated pubic symphysis disruption. Rotational deformity and instability, may also be present.
Emergency care for pelvic ring injuries should be available and preplanned at every trauma hospital. Patients with complex pelvic ring injuries may need to be referred to a specialized center. Definitive care of complex pelvic ring injuries may be centralized so that patient referral may need to be considered.
Lumbo-sacral nerve root injury
Before undertaking definitive treatment of pelvic ring injuries. It is essential to know the functional status of the patient's lumbosacral nerve roots. A careful and detailed examination is necessary, to assess perineal sensation, voluntary anal sphincter contraction, and bulbo-cavernosus reflex. Cystometrography may be helpful to assess bladder neuromotor function.
Neurologic abnormalities should be correlated with anatomic site of injury:
If a sacral nerve deficit is present with a sacral fracture, the nerves should be decompressed with fracture reduction and/or sacral laminectomy.
Early pelvic realignment
Early recognition and at least partial correction of deformity is helpful, because the mobility of the pelvic fragments decreases with swelling and hematoma organization. Circumferential wrapping as soon as possible can help correct external rotation and lateral displacement. If proximal displacement is present, traction applied to the lower extremity can improve it. Such provisional corrections are best applied early during the patient's care, before swelling and hematoma consolidation progress. External fixation, if used for initial care may similarly aid subsequent definitive reduction.
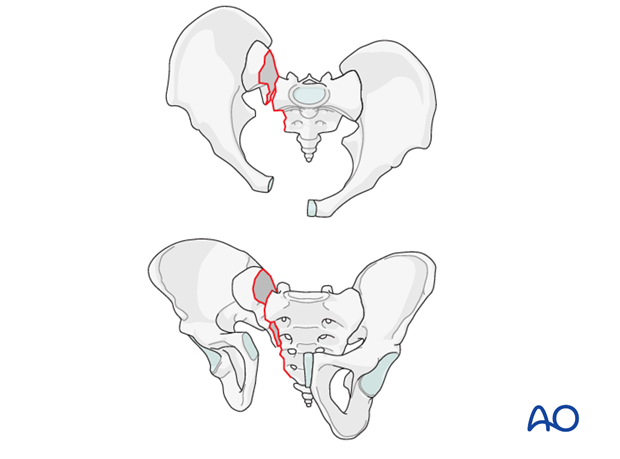
Posterior injury
The posterior component of this injury is a fracture through the sacrum.
The specific techniques of reduction and fixation will depend upon the sites of injury, the fracture pattern and displacement, as well as patient factors and available resources.
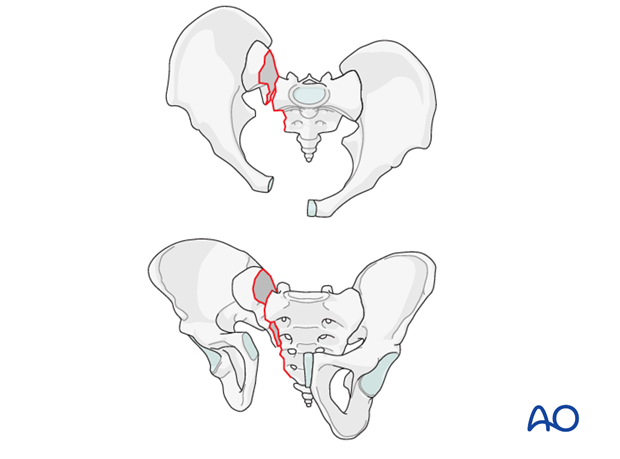
Anterior injuries
At least one site of anterior arch disruption is almost always present, involving
- pubic symphysis disruption
- body fracture
- pubic ramus fracture
Their displacement and instability range from slight to extreme.
In general, pubic symphysis disruption, especially with significant displacement, should be treated with open reduction and internal fixation. Pubic ramus fractures, whose instability may be limited by soft tissue restraints may be treated with internal or external fixation. Their reduction may help reduce posterior arch displacement, and their fixation contributes to overall pelvic ring stability.
2. Preoperative planning
An explicit, written pre-operative plan is strongly encouraged. The following provides an outline of recommended steps.
Assess and consider:
- Whole patient (physiologic status and other injuries)
- Pelvic region & organ systems (local details of pelvic region including soft tissues and related organ system injuries)
- X-rays and CT scans (reviewed in detail for patients individual anatomy, each injury, and overall pelvic configuration)
for patients individual anatomy, each injury, and overall pelvic configuration)
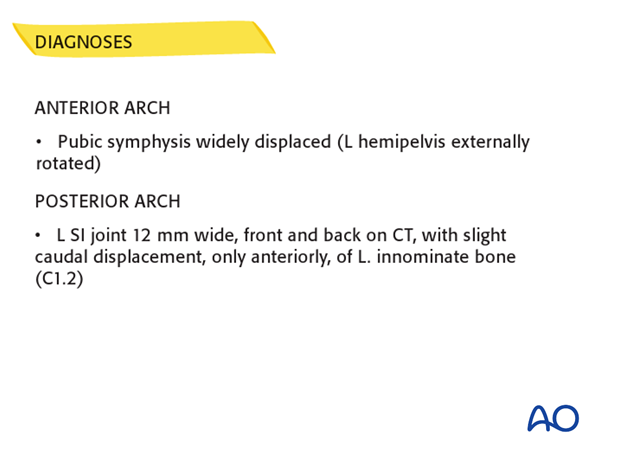
Identify and list each individual pelvic ring injury
For each injury, determine displacement, stability, and a strategy for reduction and fixation (relevant techniques are outlined and discussed below).
List, in order, each step of your planned procedure
Finally review the step-by-step list to:
- Confirm plan
- List equipment and implants
- Consider potential problems and solutions
- Share the plan with other members of the operative team – including nursing staff, radiographic technician, and anesthesia staff.
Note:
- Minimizing the amount of additional soft tissue damage and operative blood loss is important. Efficient use of surgical time is required to avoid excessively long procedures.
- Sufficient blood replacement must be available. Intraoperative blood salvage should be considered.
3. Patient preparation
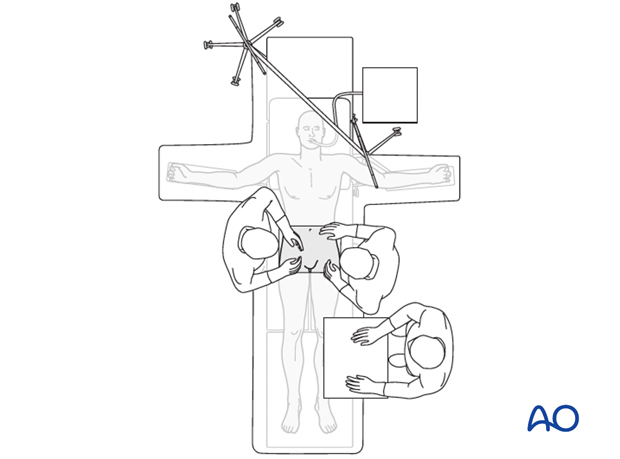
Combined supine and prone
If it is necessary to change positions intraoperatively (from supine to prone position or vice versa), the surgeon must choose the order for performing the procedures. This information must be communicated to the other members of the surgical and anesthesia teams.
In cases where both anterior and posterior approaches are required, simultaneous access is not possible. Thus, it is important not to apply fixation that might prevent satisfactory reduction of remaining ring injury components.
After completion of the initial procedure, in this example, the posterior one, the incision is closed, and a dressing applied.
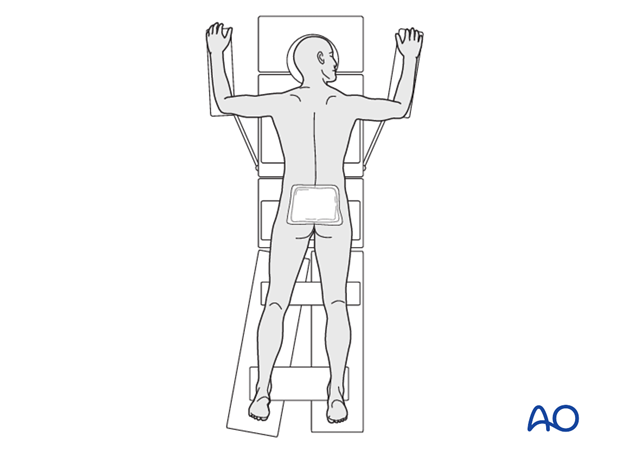
The patient is turned “like a log” supine onto an adjacent stretcher.
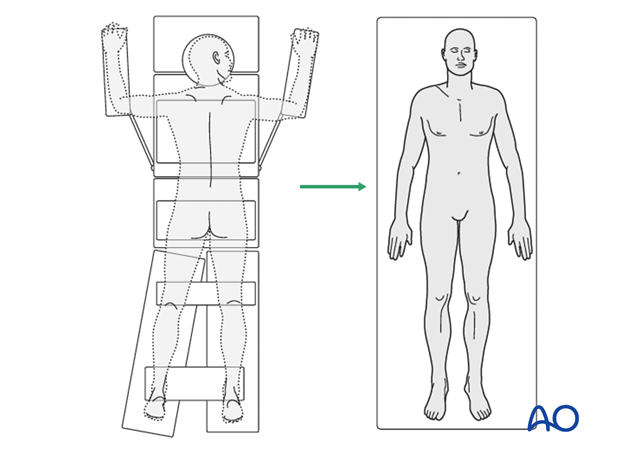
The patient is then transferred, with a roller, sliding board or sheet, back onto the operating table.
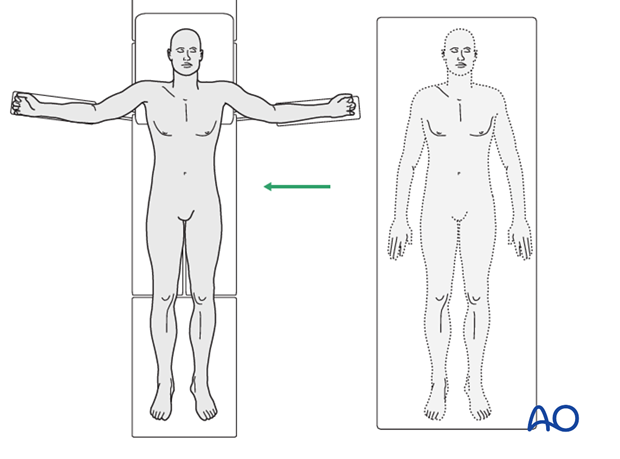
The anterior operative area is prepared and draped as necessary.
If an anterior procedure to be performed first, followed by a posterior approach, the sequence is reversed, and the patient turned and transferred in a similar fashion.
4. Reduction
General guidelines
Once the injury sites have been identified and clarified with appropriate imaging studies, the surgeon can prepare for definitive deformity correction and pelvic fixation.
Reduction maneuvers follow the sequence below until satisfactory reduction is achieved at each site of deformity:
- external manipulation
- percutaneous control and manipulation of displaced pelvic segments
- open reduction
If it is possible to obtain a satisfactory reduction without open exposure, and the bony injuries can be stabilized with percutaneous fixation techniques, this is preferable, to avoid additional blood loss and reduce the risk of wound healing problems.
Open surgery may be necessary to achieve satisfactory alignment or fixation. If so, the specific surgical approach should be planned according to the site of injury and chosen fixation technique. While preliminary reduction maneuvers may be helpful, the final direct reduction occurs after exposure.
It may be possible to achieve a satisfactory reduction of both anterior and posterior ring with initial ORIF of one site.
Restoration of overall pelvic alignment must be monitored with inlet and outlet imaging during reduction and fixation, and not lost sight of during repair of individual fractures.
Sacral fracture with minimal displacement and no neurologic deficit
Some completely unstable pelvic ring injuries involving the sacrum are undisplaced (< 5 mm displacement), but have a high risk of progressive deformity. Although reduction is not necessary, fixation is indicated to prevent loss of alignment which is much more difficult to correct.
Signs of sacral fracture instability are a complete fracture line through both anterior and posterior cortices, comminution for the sacral fracture, and gapping of the fracture throughout its length. Multiple, comminuted and displaced pubic ramus fractures also suggest greater sacral instability.
Reduction of completely unstable pelvic ring injury with major displacement and/or neurologic deficit
Because of neurologic deficit or risk thereof, decompression of the sacral nerve roots is performed before the definitive reduction. The procedure is planned from preoperative CT assessment as well as neurological evaluation.
5. Fixation
Sacral fracture with minimal displacement and no neurologic deficit
If alignment is satisfactory these fractures can be stabilized with percutaneous iliosacral screw fixation.
With significant instability, some form of anterior arch fixation, based on the injury pattern, should be added (see below).
Sacral fracture with complete instability, major displacement, and/or neurologic deficit
Exposure.
Sacral plate fixation is recommended.
Posterior sacral laminectomy with decompression of the sacral nerve roots, open reduction, and stable internal fixation is recommended.
If comminution is significant, interfragmentary compression should be performed with caution, if at all.
Following posterior plate fixation, it will be necessary to add anterior stabilization, with reduction if required. This is necessary to protect the posterior sacral fixation from cyclic loading and fatigue.
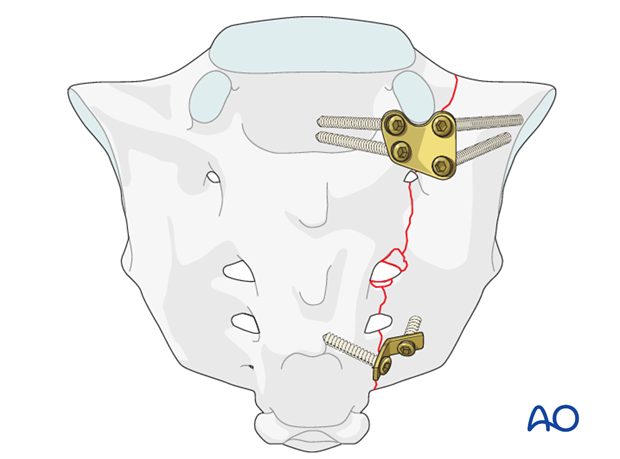
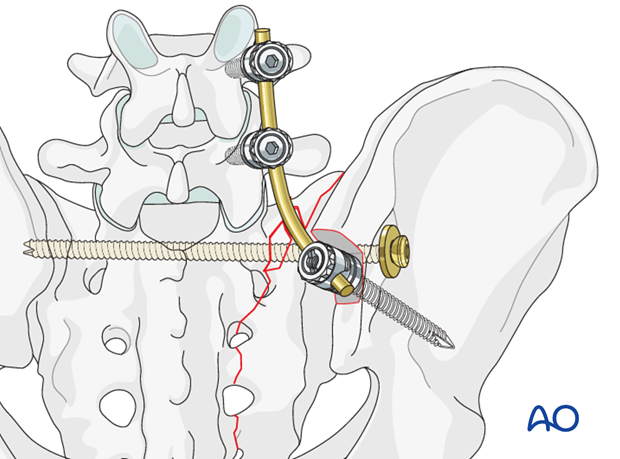
In the case of severe unilateral sacral fracture instability, or lumbosacral instability, supplementary triangular fixation should be considered.
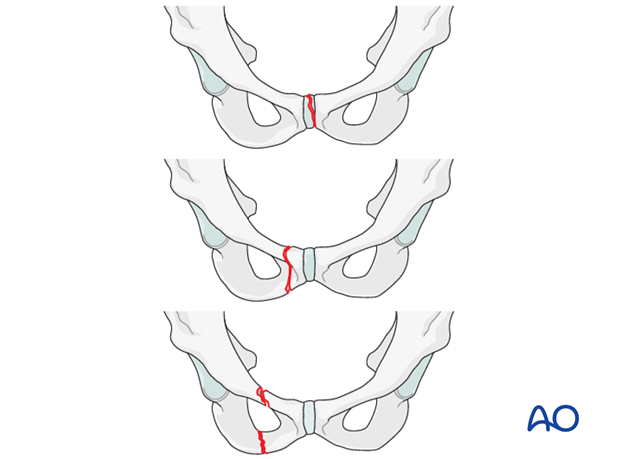
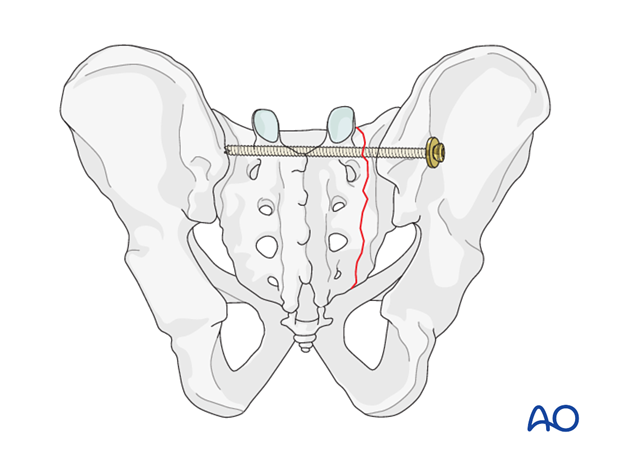
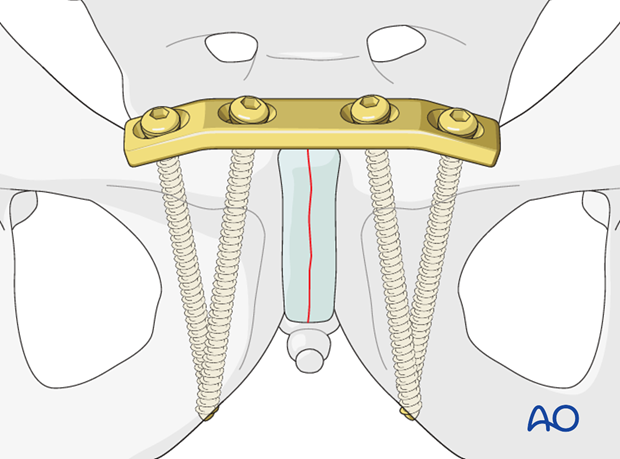
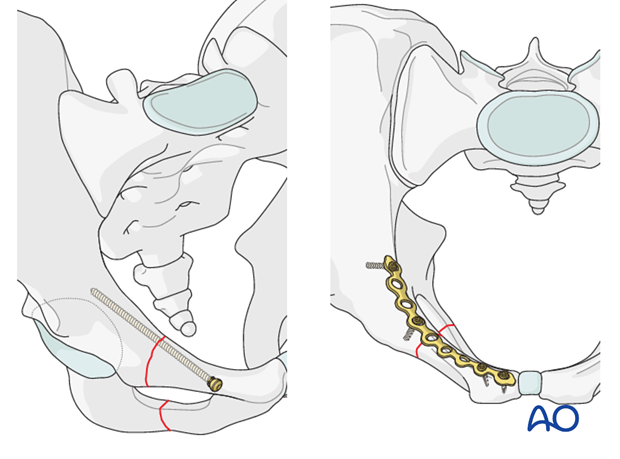
Pubic symphysis
The pubic symphysis plate is indicated for symphyseal disruption and/or pubic body fractures.
Fixation
Pubic ramus
Pubic ramus fractures have several options.
If alignment is satisfactory, they can be treated with external fixation until they are healed:
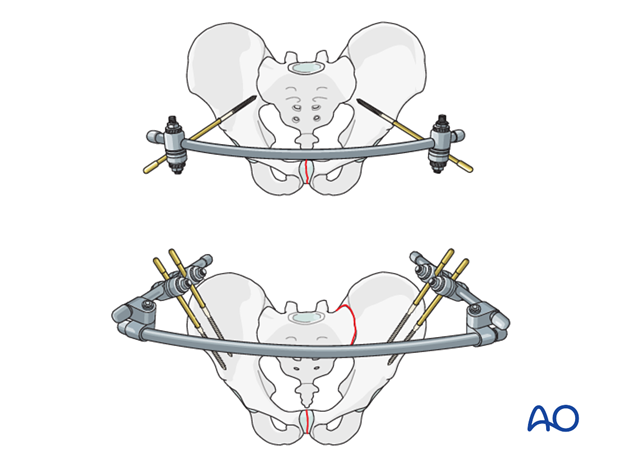
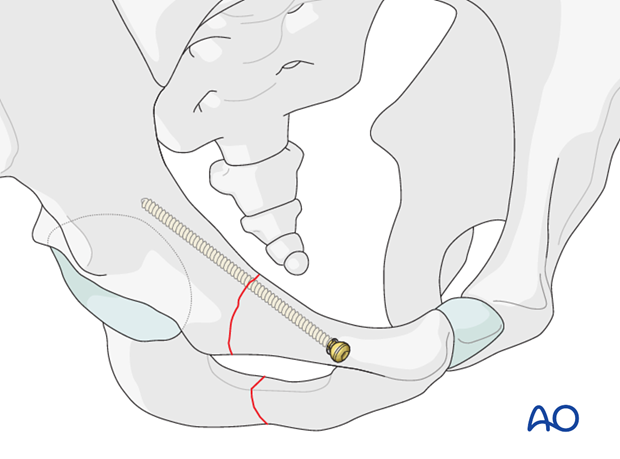
Alternatively, percutaneous intramedullary screw fixation can be performed to avoid external fixator complications and inconvenience.
If closed reduction of pubic ramus fractures is not satisfactory, open reduction should be considered.
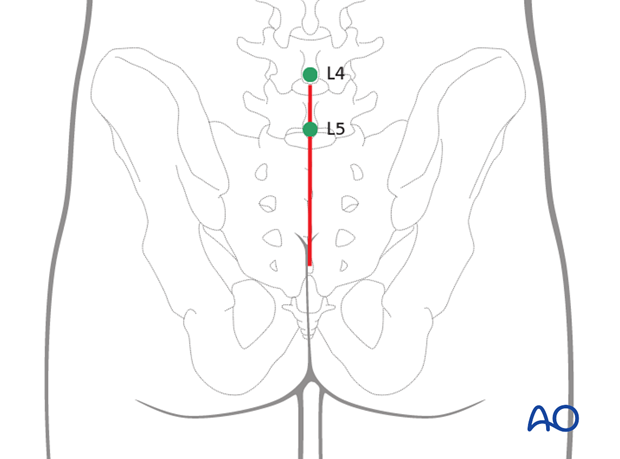
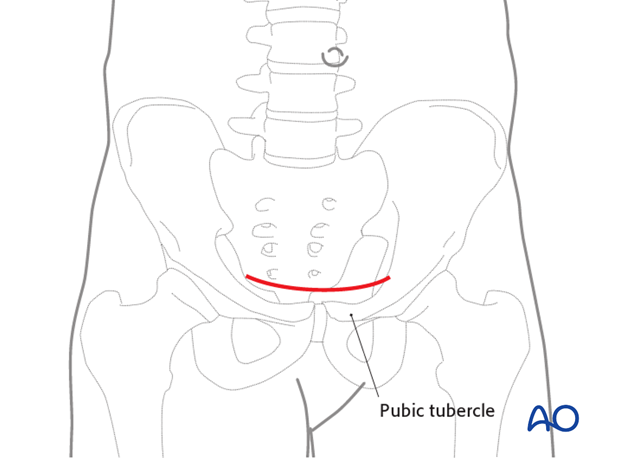
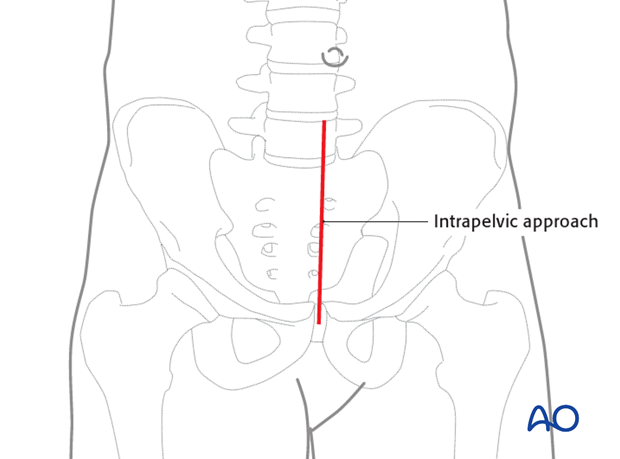
Exposure:
- Anterior approach to the symphysis (medial fractures)
- Modified Stoppa approach (lateral fractures, or posterior plating)
Fixation:
6. Check of osteosynthesis
Check the completed osteosynthesis with Imaging, and physical exam if there is any question about pelvic stability.
Using inlet and outlet views, with the C-arm, confirm that pelvic deformity has been corrected and that involved sacroiliac joints and pubic symphysis are anatomically reduced.
Unless a C-arm with a large field of view is available, it may be wise to obtain similarly oriented portable x-rays of the entire pelvis, to be certain about overall alignment.
Confirm that reduction of each fracture or joint injury is satisfactory, Make sure that all fixation devices are properly placed, and that each screw is of appropriate length. Multiple views are typically needed, including both axial and perpendicular views for questionable screws. If screws protrude from bone, consider risks to nerves, vessels, and adjacent viscera, especially urethra and bladder after pubic symphysis repair.

7. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













