Pubic symphysis plate
1. Introduction
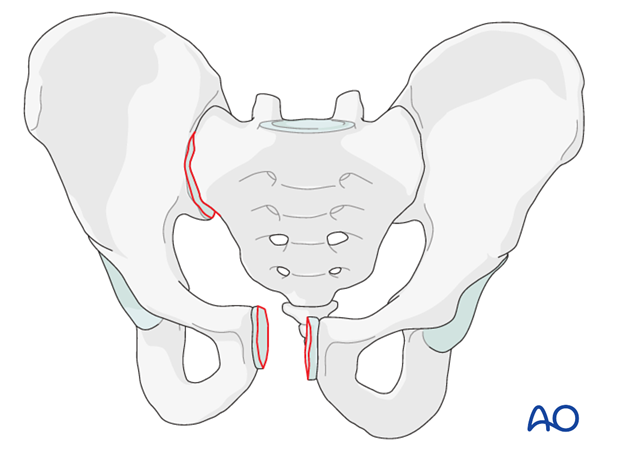
ORIF of pubic symphysis disruption is performed in cases of unstable pelvic ring injuries.
The procedure requires exposure of the pubic symphysis to allow for reduction and stabilization using plates and screws. For this procedure, the standard approach to the pubis symphysis is used.
Most anterior injuries have associated posterior injuries. In some cases, reduction and stabilization of the symphysis is sufficient to reduce and stabilize the posterior injury. However, some posterior injuries are severe enough so that their fixation might be required as well.
2. Patient positioning
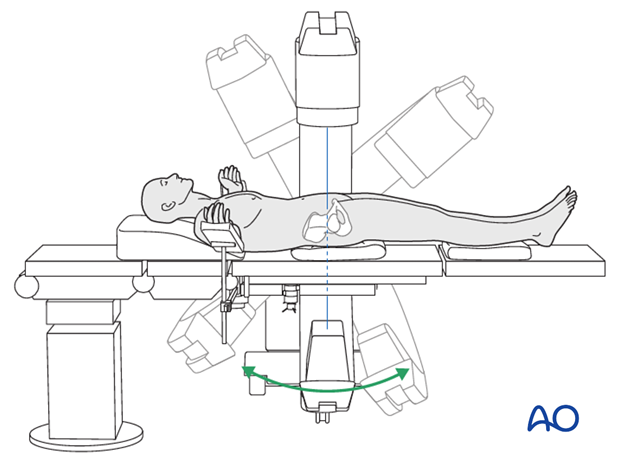
Place the patient in the supine position on a radiolucent table.
A urinary catheter should be inserted prior to beginning the procedure.
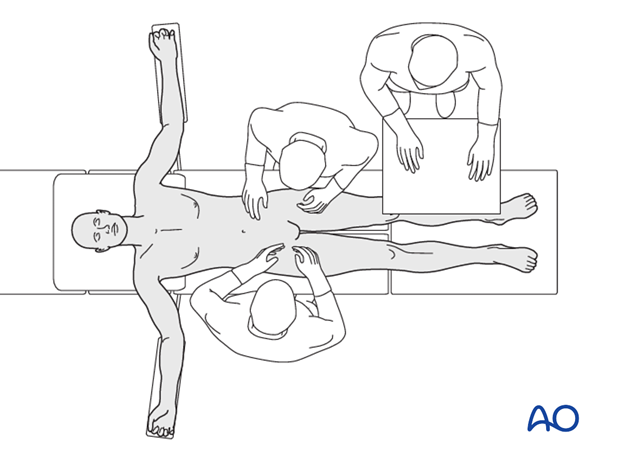
Prior to starting the procedure fluoroscopic AP, inlet and outlet x-rays should be obtained to ensure adequate visualization.
3. Reduction
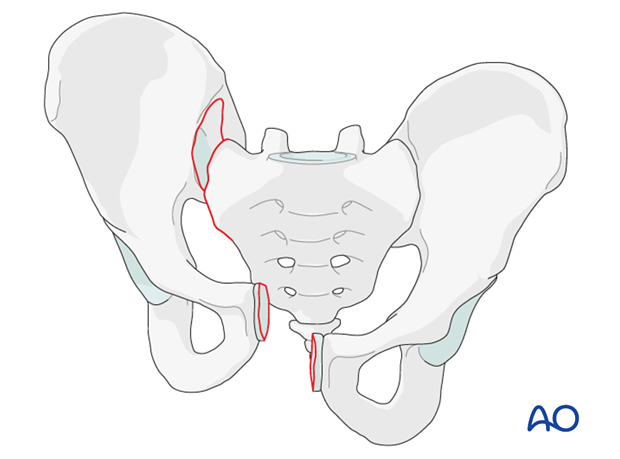
Order of reduction
Prior to beginning this procedure, it is important to analyze the radiographs and the CT-scan to determine the amount of posterior pelvic ring displacement.
If there is no vertical displacement (B-type injuries), and it is possible to reduce the entire pelvis with reduction of the symphysis, then anterior reduction should usually be first.
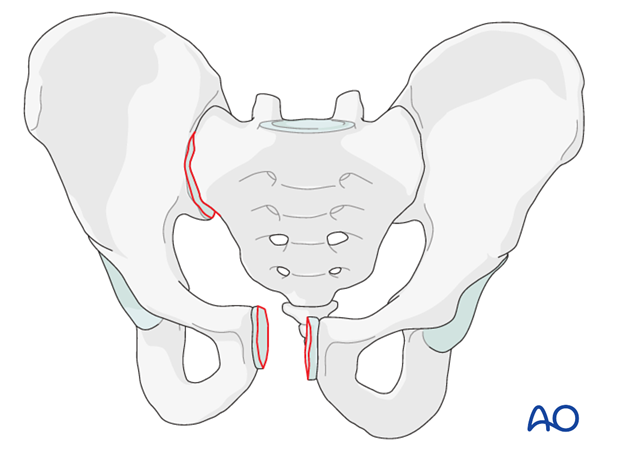
If there is vertical displacement (C-type injuries) or if anterior reduction fails to achieve posterior reduction, then posterior reduction should be performed first.
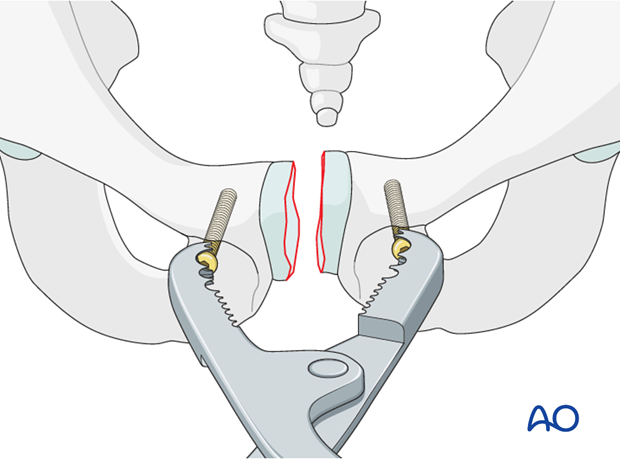
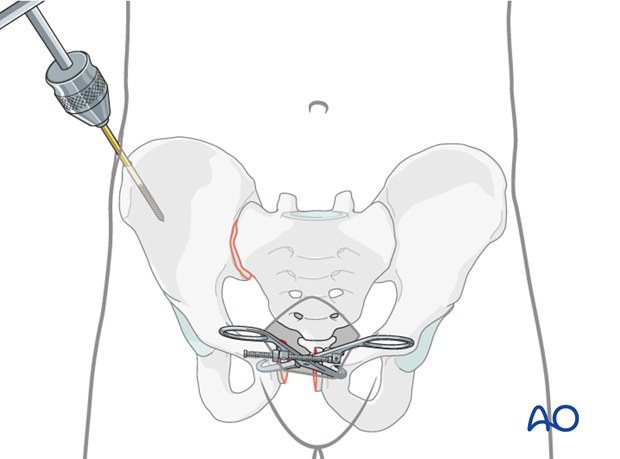
Use of a Farabeuf clamp for reduction
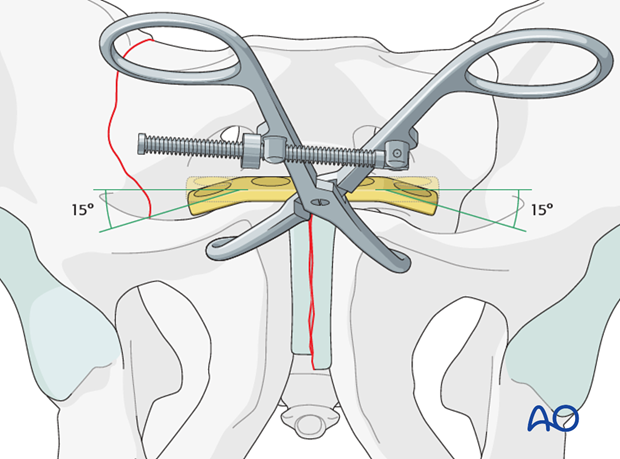
Introduce one 4.5 mm cortex screw into each pubic body on the opposing sides of the disrupted symphysis.
Apply the jaws of a Farabeuf clamp over the heads of these screws.
Manipulation of the clamp allows reduction in multiple planes and compression. Manual compression from both sides will aid reduction.
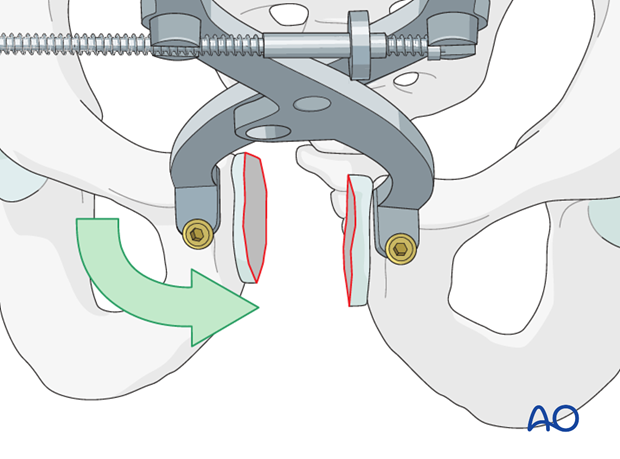
Anterior reduction should be confirmed by direct visualization and palpation. It is also important to ensure that posterior reduction is satisfactory.
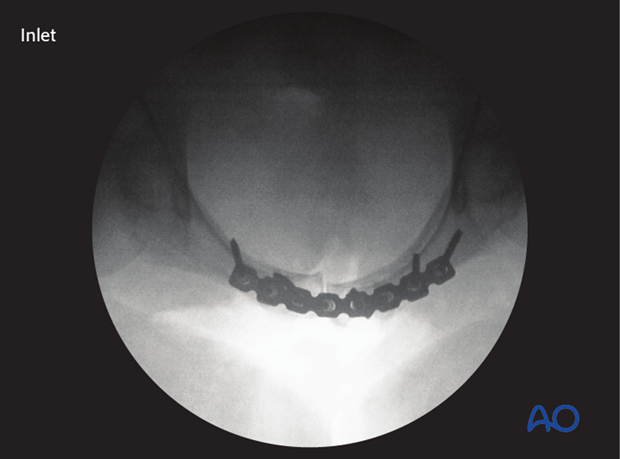
Image intensification is used to assess the reduction and external rotation displacement. Subsequent reduction is best judged in an inlet radiograph.
Rotation of the clamp is utilized to correct superior or inferior displacement of either hemipelvis.

The Jungbluth clamp may allow for better rotational control than the Farabeuf clamp.
The Jungbluth clamp requires greater exposure and might interfere with plate fixation.
Care is necessary to avoid bladder injury during insertion of screws for this clamp.
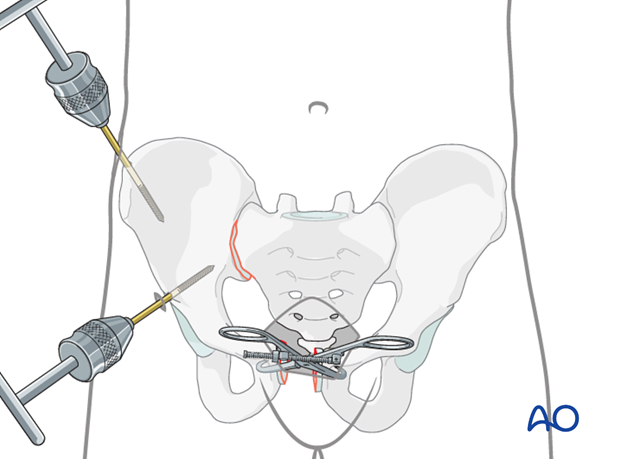
Use of pointed reduction forceps as an alternative device
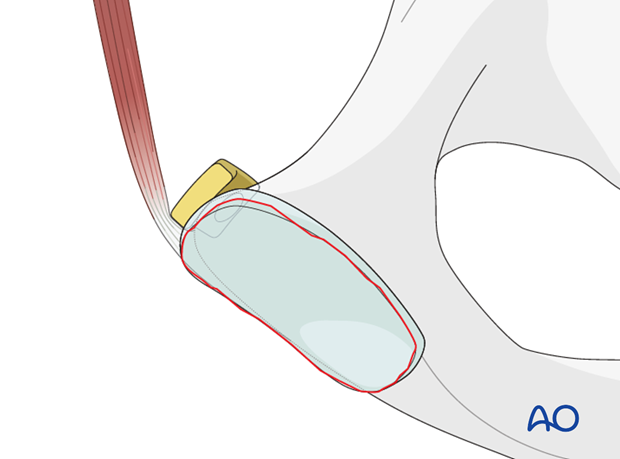
Place the reduction forceps tips either laterally to the pubic tubercles or onto the edges of the obturator foramina. To prevent slipping, predrilling the cortex may be necessary in case of hard bone.
Manual assistance, while the clamp is tightened, will help achieve reduction.
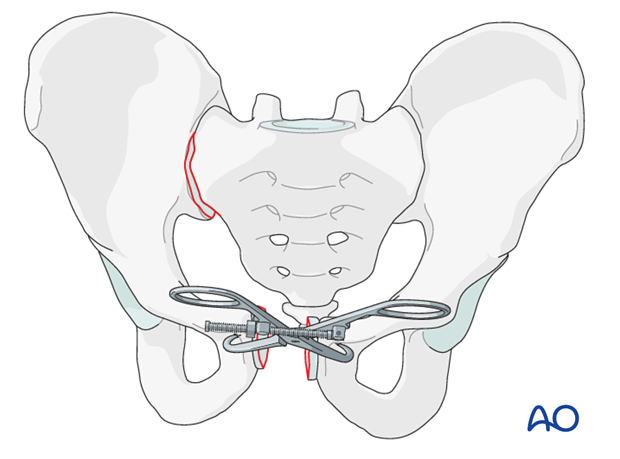
Pearl: rotational reduction
If indicated to correct rotational malalignment, use a Schanz screw additionally. This is inserted into the iliac crest as a joy stick.
The Schanz screw can also be placed in the supraacetabular region.
4. Application of the plate
Plate selection
After reduction is achieved and held provisionally with a clamp, the symphysis is fixed with a plate. Various types and sizes of plates have been utilized.
If available, a curved 3.5 mm, 4- or 6-hole pelvic plate should be used. Place it "on top" of the symphysis so that there are two or three holes on each side to control the rotation.
Although angular stable plates can be used, placing the screws at different angles may be more important.
Alternative
Alternatively, a 4.5 mm dynamic compression (DC) plate can be used.
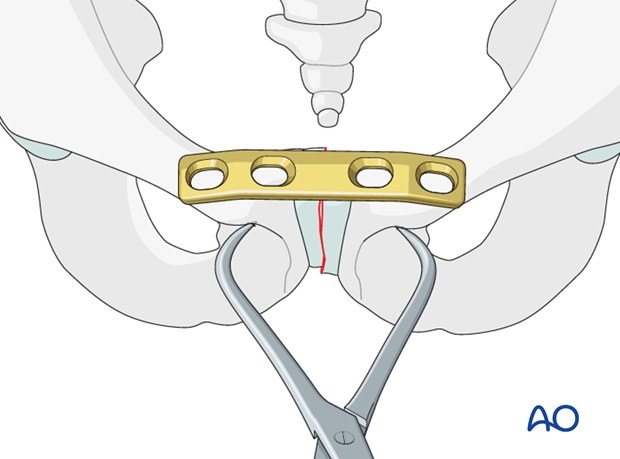
Plate positioning
Position the plate posterior to the muscle attachments.
Protect the bladder during fixation of the symphysis.
Contouring the plate for optimal fit
If a 4.5 mm DC plate is used, it may be necessary to contour both ends of the plate by creating approximately 15° angles for optimal screw direction.
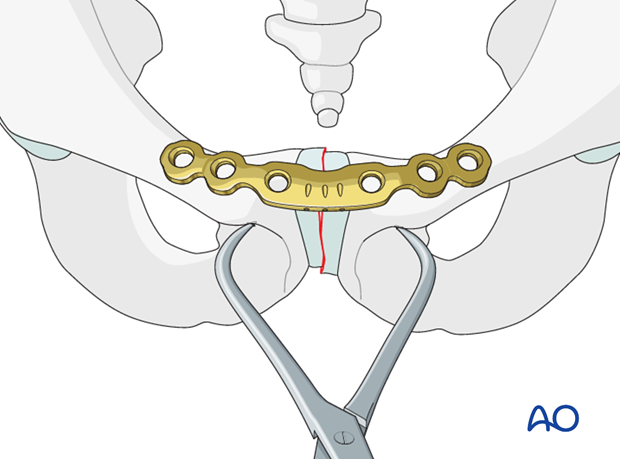
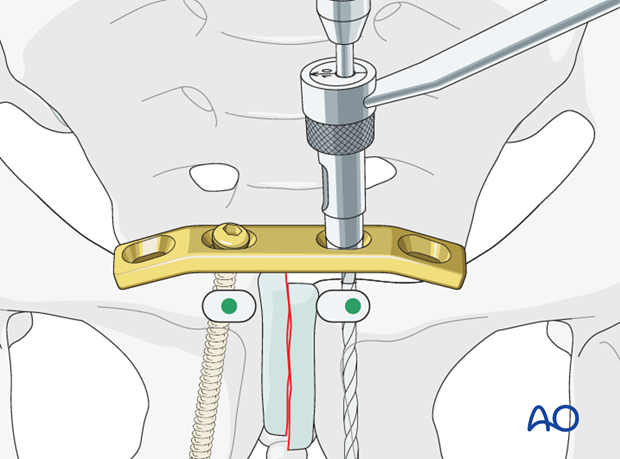
Drilling the first medial hole
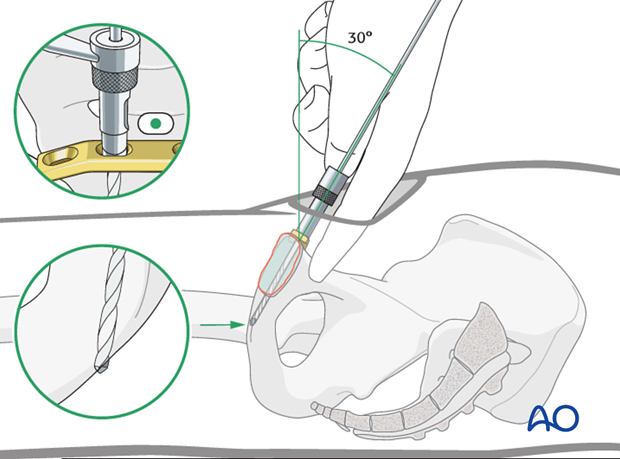
After reduction, the contoured plate is mounted on one pubic ramus.
Use the appropriate size drill bit with a drill sleeve.
To achieve the longest screw length in the plate, the drill should be oriented from proximal posterior to distal anterior. The posterior surface of the pubis is palpated to facilitate this trajectory. The drill should be run until it perforates the far or distal cortex.
The first drill hole may be made with the plate in position (as shown) or prior to placing the plate. Drilling the hole without the plate may allow better visualization and palpation of bony landmarks.
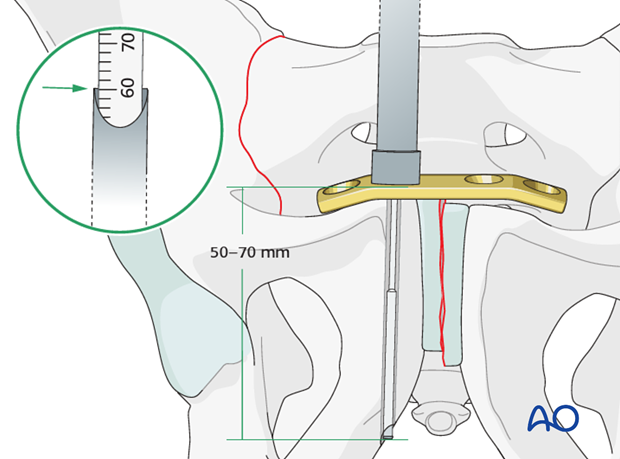
Measuring screw length
It is important to use long screws. The screw direction and exit site can be determined with a depth gauge during measurement.
Drilling the second medial hole
In eccentric position, drill the medial hole in the contralateral pubic ramus.
Eccentric drilling allows for compression across the pubic symphysis.
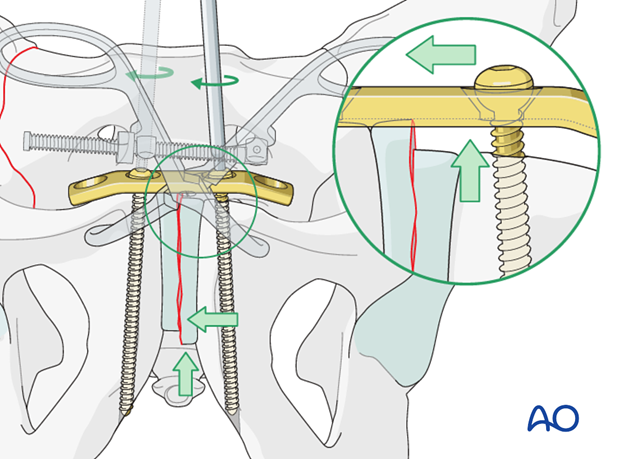
Fixation of the pubic ramus
If there is residual superior or inferior displacement, the plate may be utilized with manual assistance to correct this (as illustrated in the inset).
The screws are tightened in alternation until final fixation is achieved.
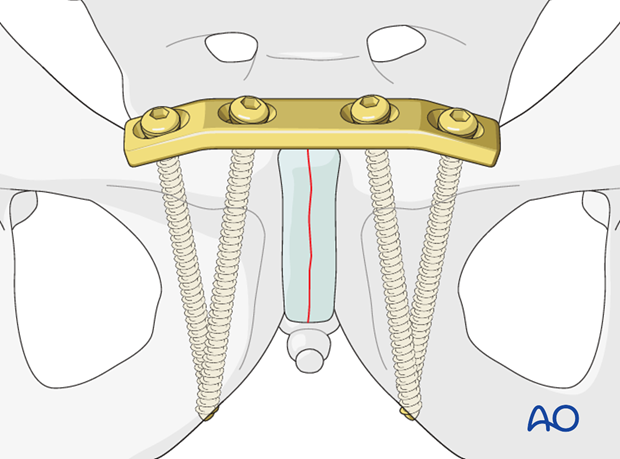
Insert the lateral screws
In order to improve fixation the surgeon should attempt to maximize the screw length. This can be achieved by placing the screws at different angles when utilizing a 4-hole 4.5 mm DC plate.
Choose a slightly convergent direction for the lateral screws.
Aim the drill bit towards the tip of the medial screw on each side for direction.
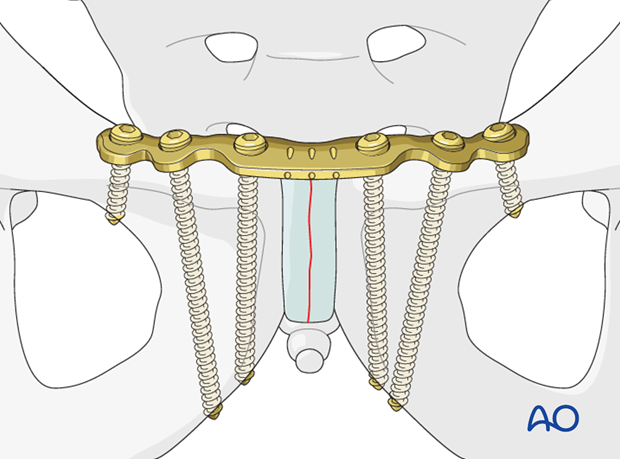
When utilizing a 6-hole 3.5 mm pelvic or reconstruction plate, screw length can be maximized by slightly diverging the medial screws and placing an additional bicortical screw in the superior pubic ramus.
Once all screws are placed, final tightening of all screws should be performed.
Note
Locking screws are advantageous in case of osteoporotic bone stock.
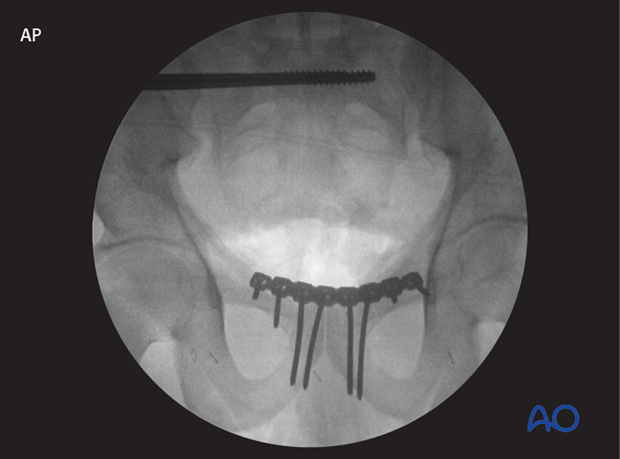
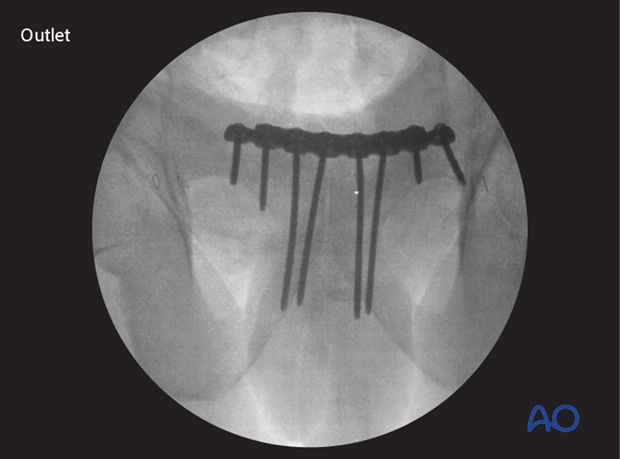
5. X-rays
Intraoperative image intensification
Intraoperative X-rays should be obtained in the following views to confirm reduction and plate position.
AP view
Outlet view.
Inlet view.
Postoperative X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.














