ORIF sacrum
1. Introduction
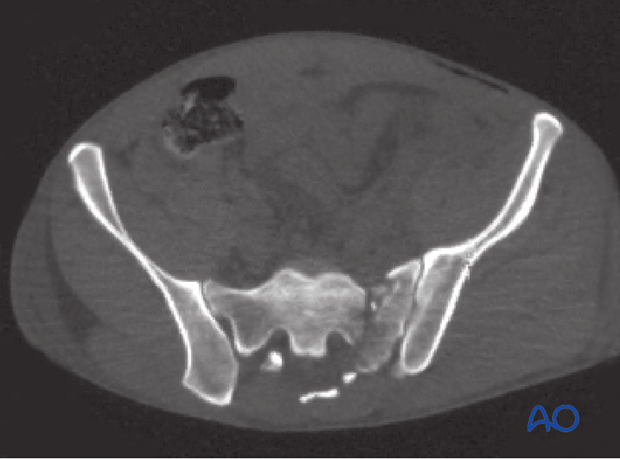
Vertical sacral fractures that do not involve the sacroiliac joint typically pass obliquely through the transforaminal region. They are often comminuted.
Because of the risk of nerve injury from compressing the comminuted fracture, interfragmentary compression may not be a good option in some patients.
Plate fixation of the sacrum must be performed posteriorly and typically involves the use of several small plates.
2. Preparation of the fracture site
Identify and remove small bony fragments from the comminuted fracture zone. They may be located in the transforaminal region and may hinder fracture reduction.
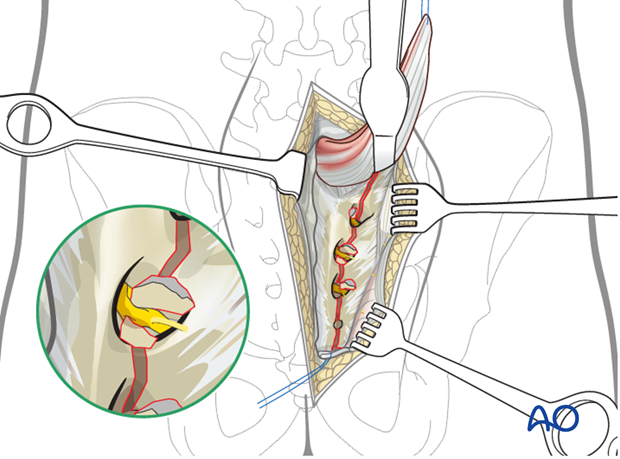
Sacral nerve root decompression
The complete fracture line has to be cleaned out and inspected.
Enhance the exposure by using a lamina (bone) spreader.
Extract fragments that may compromise the sacral nerve roots.
3. Reduction
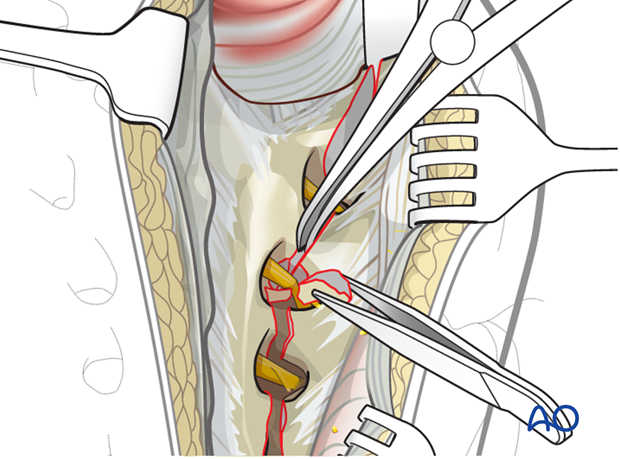
The typical displacements are cranial and posterior together with sagittal plane rotation.
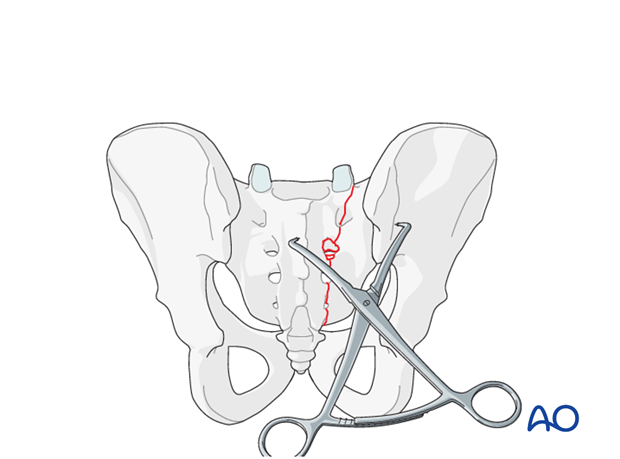
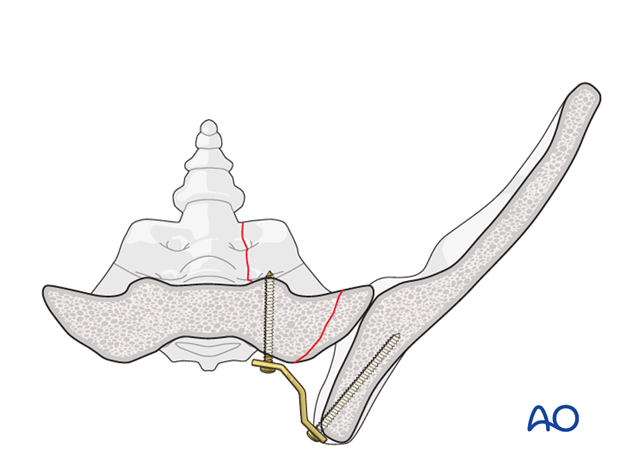
Preliminary fixation
The primary reduction maneuver typically involves the use of two pointed reduction forceps (Weber clamps).
These span from the spinous process to the lateral ilium and are used to incrementally obtain a step by step reduction by alternating translation and clamping.
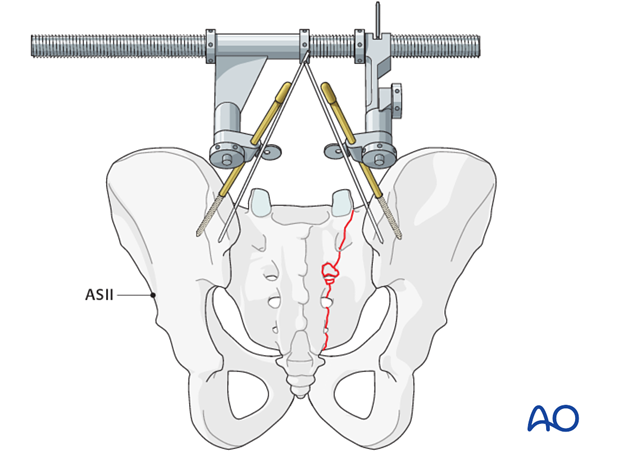
Additional reduction techniques
Preliminary fix the anatomic reduction with pointed reduction forceps.
If needed, insert Schanz screws to both posterior iliac crests as a reduction aid for better rotational alignment.
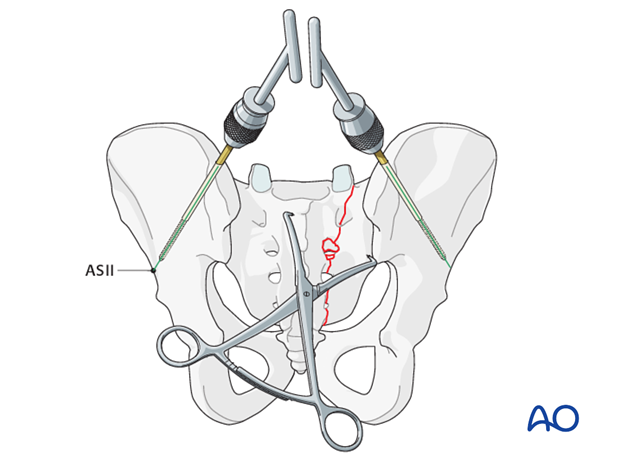
The AO distractor may be used as a distraction aid.
K-wires may be placed into the SI joints in order to determine the joint orientation.
4. Plate application
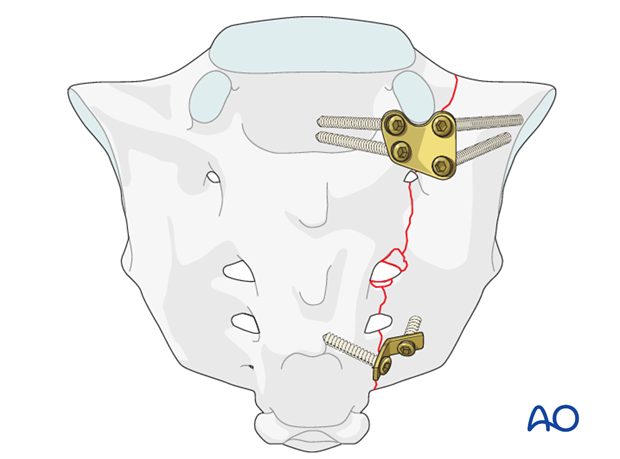
H-plate fixation
Implants for stabilization are standard H plates that are cut to the required length, and flattened.
One-third tubular plates and standard small fragment DC-plates are also possible variants in plate fixation.
Cross the fracture line by at least two implants, preferably at the S1 and S3 or S4 level.
The position of the implants is determined by the specific fracture pattern.
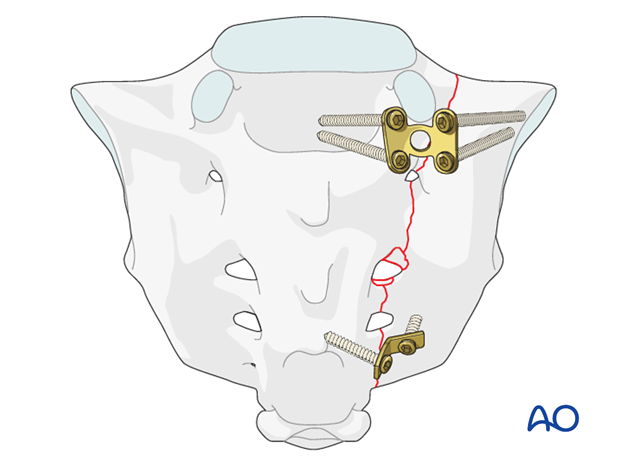
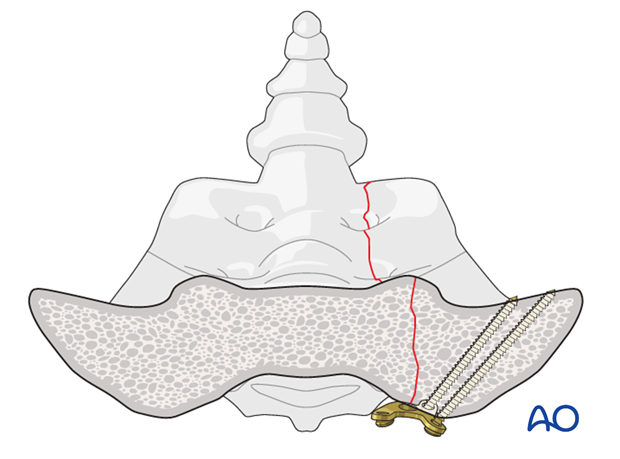
Lateral screw fixation (alar screws)
Apply the screw as far lateral as possible, using the more solid bony substance close to the SI joint.
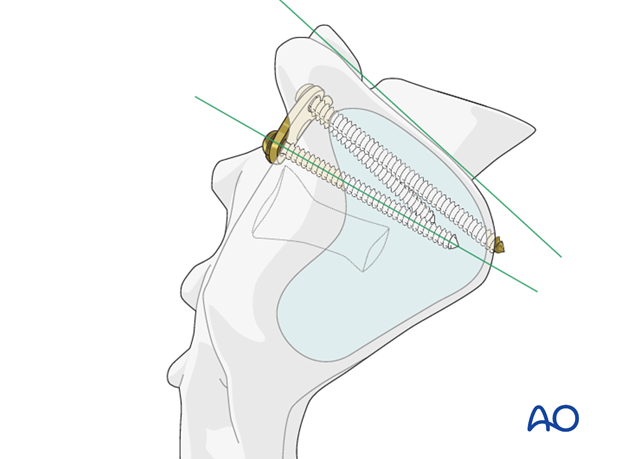
Position 3.5 mm screws in the sacral ala parallel to the plane of the SI joint.
Give special consideration to the internal iliac vessels located ventrally.
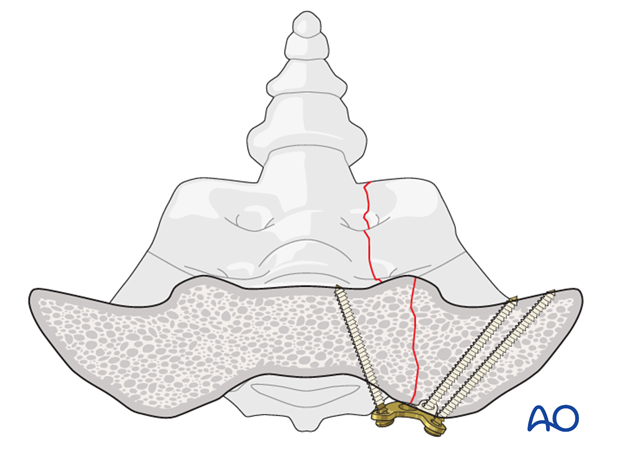
Medial screw fixation
Insert the medial screws perpendicular to the posterior aspect of the sacrum.
Diversify the direction of the screws according to the fracture line.
Medial screw fixation in the sagittal plane
When placing screws into the sacrum at the level of S1 take into consideration the cranial sacral border.
Completion of the H-plate fixation
Complete screw placement when H-plate is inserted with the application of the medial screws.
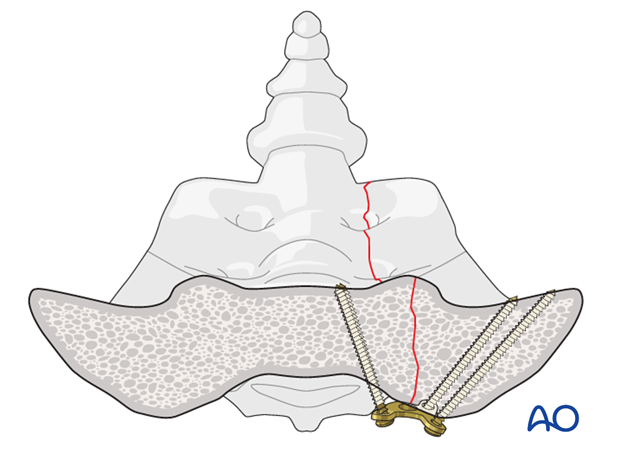
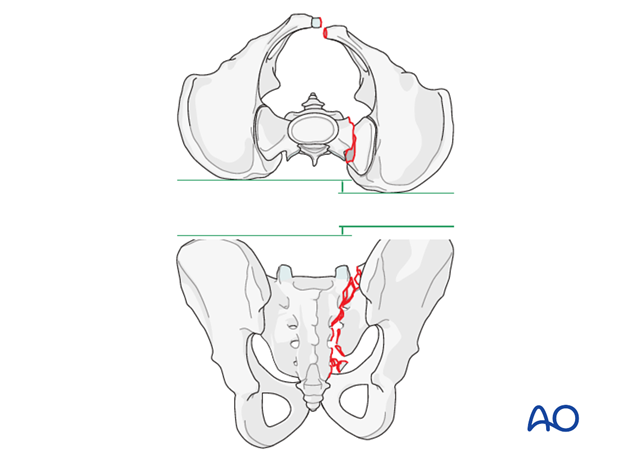
Iliosacral plating in transalar fractures
In case of a laterally located sacral alar fracture, it may be advisable to bypass the zone of comminution by placing screws in the posterior ilium.
5. Various options for plate fixation
Transforaminal fractures
The use of a special sacrum plate allows the placement of two lateral and two medial screws at the level of S1.
Additional dorsal fixation with one flattened and contoured 2-hole one-third tubular plate should be performed to provide additional stability at the level of S4.
Alternative fixation technique
Fixation may be spanned across the entire sacrum, extending from one sacral ala to the other.
Contour two 3.5-mm LC-DC plates to the posterior aspect of the sacrum as neutralization plates.
Position both plates parallel to each other at the S1 and S3 level.

6. X-ray control
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.














