ORIF - Buttress plate and lag screws
1. Preliminary remarks
Partial articular split fractures of the distal tibia
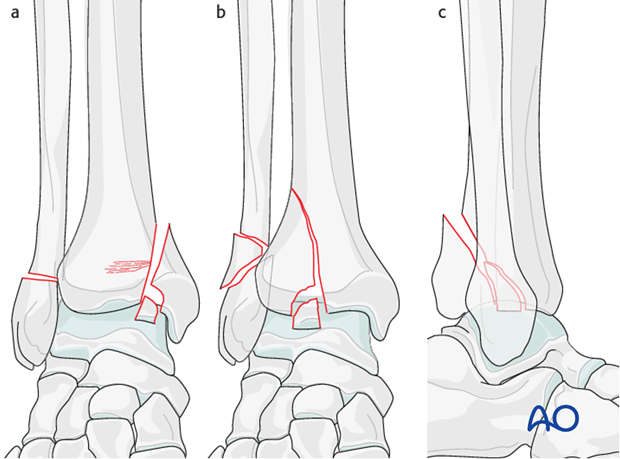
These fractures are partial articular, involving both splitting and depression of the joint surface. The surgical approach is dependent on the fracture location and the associated articular impaction or comminution. Common fracture locations include:
- Sagittal medial split fractures (fig. a) with associated articular impaction. In these patterns, impaction and comminution at the medial shoulder of the ankle joint is common. Frequently there is an independent osteochondral fragment at the fracture entry site into the ankle joint. Additionally, there can be impaction of the medial aspect of the stable distal tibial articular surface that must be addressed at the time of fixation. An anteromedial or direct medial approach is usually used for these patterns, but if it is a more oblique fracture involving the posteromedial tibia a posteromedial approach may be preferred.
- Sagittal lateral split depression fractures (fig. b) that separate the anterolateral (Chaput) fragment that remains hinged on the anterior tibiofibular ligament. Comminution and impaction may be present at the fracture site, in the distal tibiofibular joint, or at the lateral aspect of the distal tibial articular surface. An anterolateral approach is usually used for these patterns.
- Posterolateral fractures (fig. c). The displaced fracture fragment usually remains attached to the posterior tibiofibular ligaments. Comminution and impaction may be observed at the articular margin of the fractured fragment or, more commonly, at the posterior aspect of the distal tibial articular surface. A posterolateral approach is usually used for these patterns.
Soft-tissue condition
Often, the swelling associated with these patterns is less than that observed in some complete articular patterns. Primary fixation of both the fibula and tibia can be performed acutely in circumstances where the soft tissues allow the multiple surgical approaches.
However, if significant swelling is present, a staged protocol should be employed. This consists of fibular fixation combined with temporary and strategic ankle joint spanning external fixation followed by delayed definitive fixation of the tibial articular surface.
2. Fracture configuration and surgical strategy
Fracture configuration
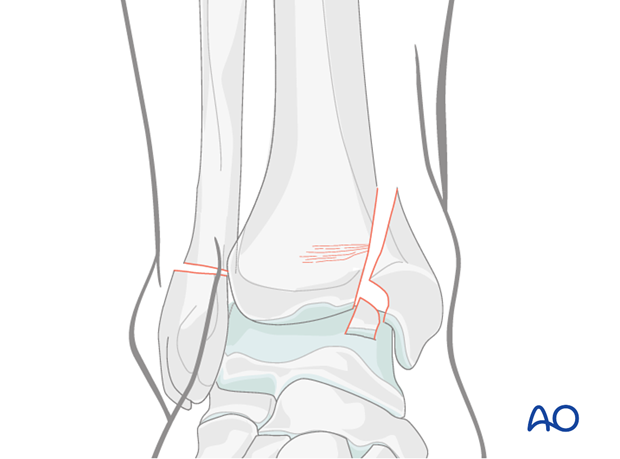
The surgical sequence will be demonstrated for an example of a vertical fracture of the medial malleolus (supination-adduction). The typical fracture pattern is demonstrated and consists of a tension failure (transverse) fracture of the lateral malleolus combined with a vertical fracture of the medial distal tibia. There is frequently comminution where the fracture begins on the tibial plafond. This is caused by compression from the medial talar dome.
The comminution and impaction are typical: There is a free osteochondral segment at the junction of the medial segment and an impaction of the medial aspect of the intact tibia.
Surgical strategy
Typically, the two-part simple fibular fracture is reduced and fixed first. This will indirectly assist with centering the talus beneath the distal tibial articular surface, allowing for ease of reduction of the articular injury and the medial fracture. An implant that resists tension is used for the fibular fracture and typically consists of a lateral plate.
3. Patient preparation
Depending on the approach, the patient may be placed in the following positions:
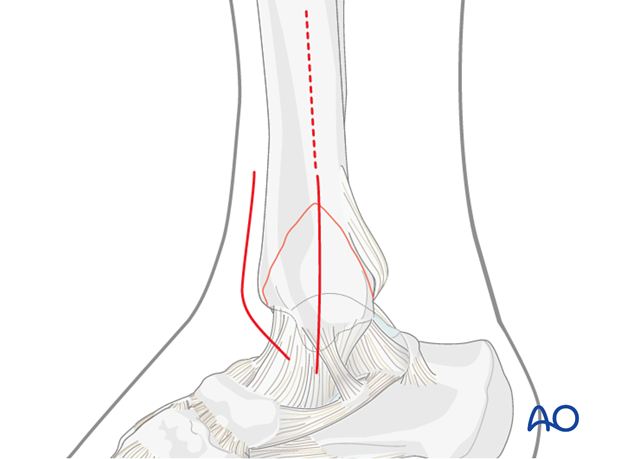
4. Surgical approach to the tibia
Resolution of the surgical swelling prior to definitive fixation of the tibial articular surface is necessary. A direct medial or an anteromedial approach is used for the tibial fracture.
The incision should extend proximally to allow for visualization of most of the cortical disruption of the fracture. Depending on the condition of the soft tissues, the incision can be extended proximally to allow for a direct plate application to the medial tibia. Alternatively, the incision can be limited to the necessary exposure for an accurate articular reconstruction followed by a minimally invasive plating technique of the medial tibia proximal to the fracture exit.
An anteromedial joint arthrotomy (anterior to the deltoid) is necessary to allow for reduction of the articular injuries.
5. Reduction
Exposure of the joint
The displaced medial fragment is rotated internally to open the fracture anteriorly and expose the joint. A small distractor can be placed from the tibia to the talar neck to allow improved visualization.
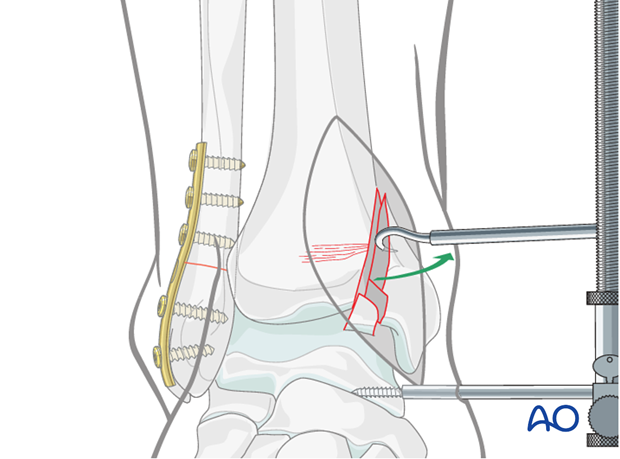
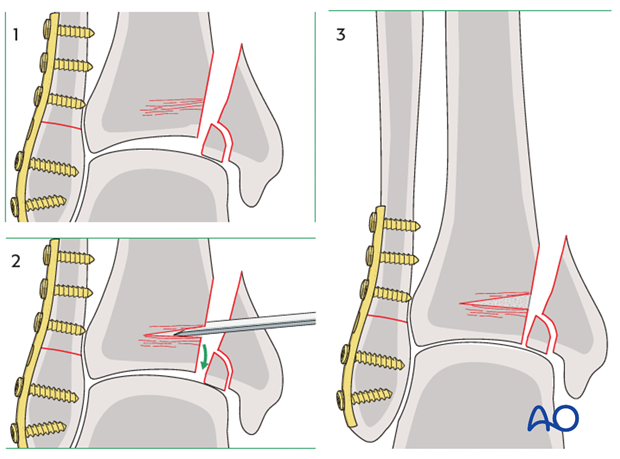
Reduction of the impacted segment
The impacted articular surface on the medial aspect of the distal tibia should first be addressed. An osteotome is placed into the cancellous bed of the distal metaphysis from medial to lateral, proximal to the impacted articular segment. The articular surface is “elevated” distally. Bone graft is placed into the defect to resist settling.
Reduction of a free osteochondral segment
The free osteochondral fragment (if present) is next addressed. This can be reduced to either the medial fragment, the “intact” tibial articular surface, or both. An accurate reduction of the medial fragment usually captures an osteochondral segment that is typically seen at the fracture as it enters the joint.
6. K-wires holding the reduction
The medial fracture fragment is temporarily held with k-wires in a reduced position. A combination of the available anterior cortical fracture line and the articular continuity are used to access the overall reduction. See also the content on assessment of reduction.
7. Fixation
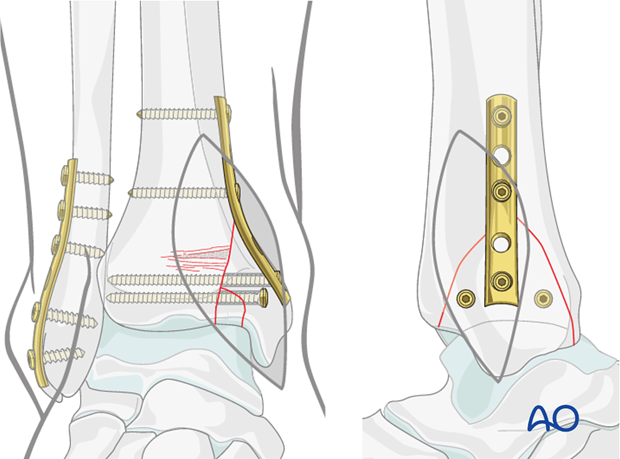
Plate preparation
A medial buttress plate should be used to definitely stabilize the vertical medial fracture. This can be placed directly through the surgical incision or can be slid subcutaneously using a minimally invasive approach.
The plate size is dependent on the fracture configuration and the degree of comminution. Typically, a one-third tubular (or a one-quarter tubular) plate is sufficient. The plate is undercontoured to allow for maximal compression. The first screw is placed just proximal to the fracture.
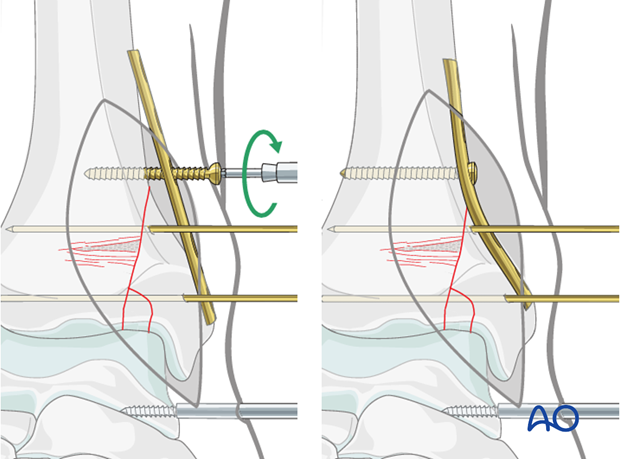
Insertion of the second and third screws
A second screw is placed in the proximal aspect of the plate.
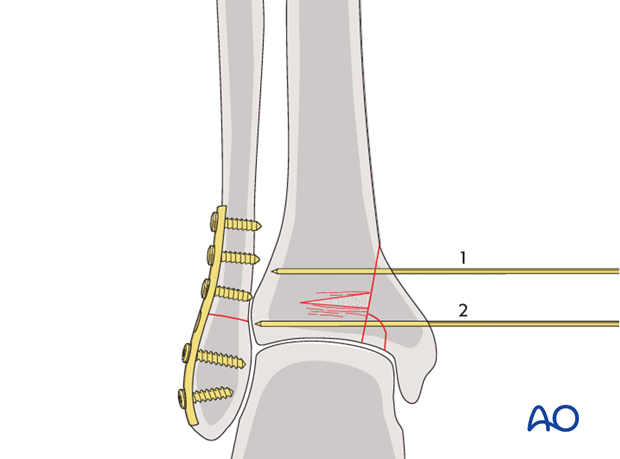
A lag screw can then be placed through the plate distally. See also the additional material on lag screw principles.
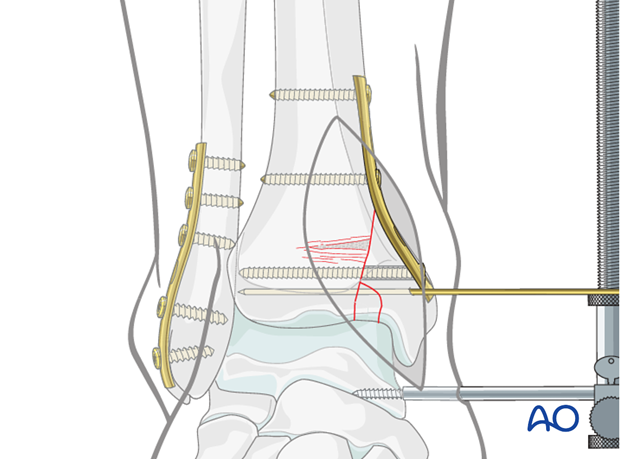
Finish fixation
Additional lag screws can be placed independently (anteriorly and posteriorly relative to the plate) or through the plate to finish fixation. Screw placement and overall reduction are confirmed under image intensification. See also the content on assessment of reduction.
8. Case example
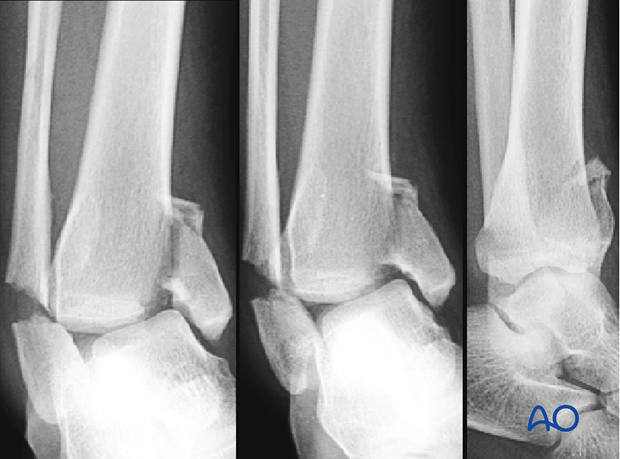
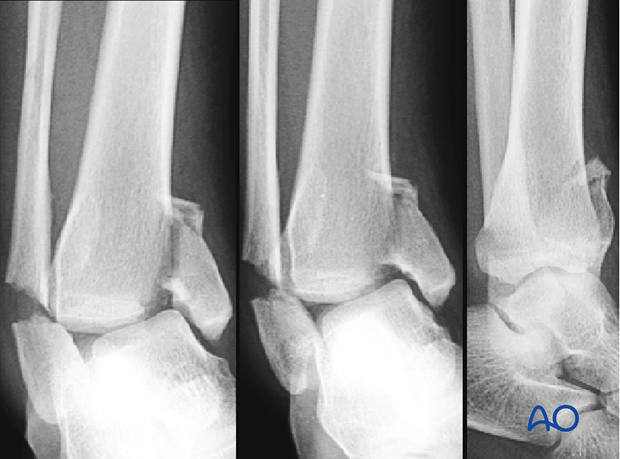
Preoperative images
Preoperative x-rays show a tension failure (transverse) fracture of the lateral malleolus combined with a vertical fracture of the medial distal tibia. There was a free osteochondral segment at the junction of the medial segment and an impaction of the medial aspect of the intact tibia.
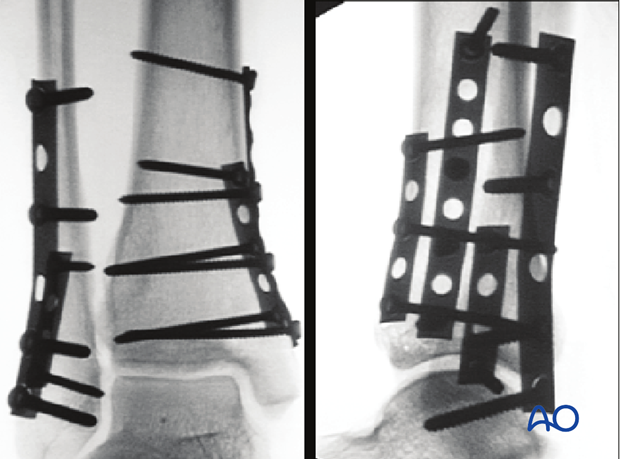
Intraoperative radiographs
Two plates were placed on the fibula (a one-quarter tubular plate and a one-third tubular plate) and two plates were placed on the tibia (both were one-quarter tubular plates). While use of more than one plate is not required for stable fracture fixation, it is an option. In most circumstances, one plate on the fibula and one on the medial tibia are sufficient.
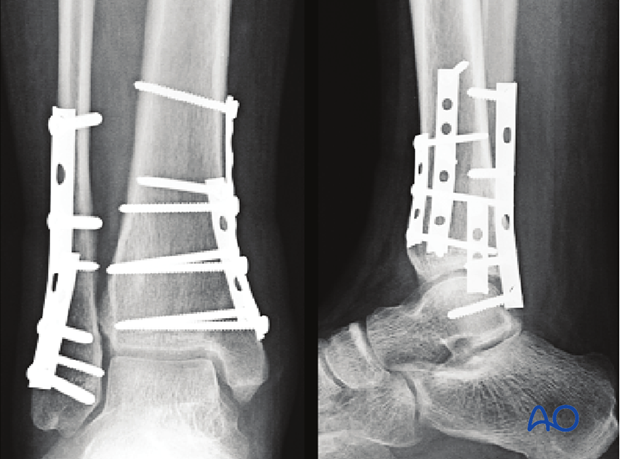
After six months
X-rays at 6 months show fracture healing.
9. Aftercare
A well padded short leg splint is initially placed to allow for resolution of swelling following surgery.
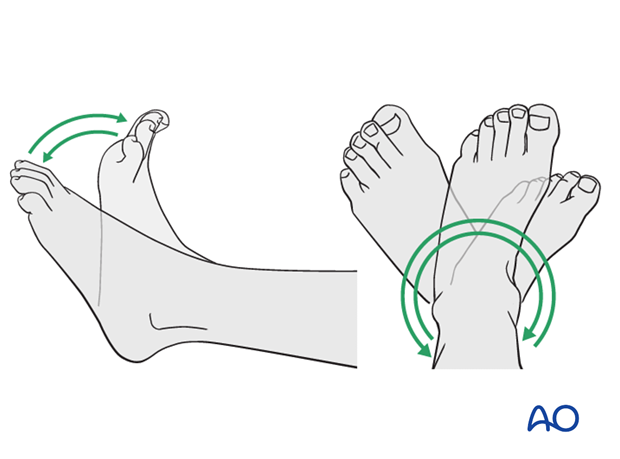
Mobilization
Early active range of motion exercises are initiated 2 to 3 days following treatment.
Weight bearing
Patients should remain non-weight bearing for 12 weeks following fixation.
Follow up
Radiographs are obtained at 6 weeks, 12 weeks, and 6 months.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implant. The best time for removal is after complete remodeling, usually at least 9-12 months after surgery.