Assessment of reduction of type B distal tibial pilon fractures
1. Principles
During the different steps of the operation, the reduction has to be assessed repeatedly using visual and fluoroscopic control. Angulation, length of both tibia and fibula, and joint surface anatomy need to be considered, as does the integrity of the ankle mortise.
Partial articular distal tibial fractures involve the articular surface which requires an anatomical reduction. Careful direct inspection and well-positioned radiographs are essential.
There is a considerable amount of anatomic variety of the ankle region, considering tibial shaft alignment, length of the fibula in relation to the medial malleolus, and width of the syndesmosis. Therefore, when there is a question of whether the joint reduction or the tibial alignment is acceptable, intraoperative fluoroscopy of the opposite (uninjured) leg should be obtained.
Acceptable reduction:
Joint surface: <1 mm intraarticular step and <2 mm intraarticular gap.
Axial alignment: <5º of varus or valgus and <10º of anterior or posterior angulation.
Fibular length and width of syndesmosis: <2 mm difference to the opposite, uninjured side.
2. Articular surface
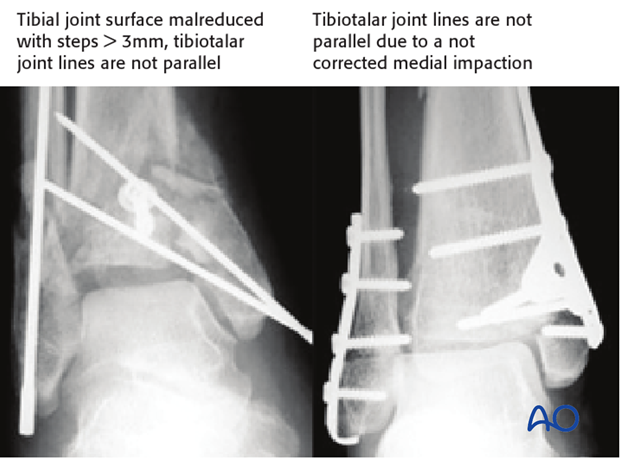
The tibiotalar joint lines should be parallel on the entire length in the AP as well as in the lateral view.
Larger intraarticular gaps can lead to a widened ankle mortise resulting in a side-to-side unstable talus with early cartilage degeneration and osteoarthritis. Intraarticular steps of more than 1-2 mm will lead to a talar tilt or shift which is demonstrated in the two examples with malreduction below.

3. Pitfall - Malreduction
Intraarticular gaps
Larger intraarticular gaps can lead to a widened ankle mortise resulting in a side-to-side unstable talus with early cartilage degeneration and osteoarthritis. Intraarticular steps of more than 1-2 mm will lead to a talar tilt or shift.