Posterolateral limited open approach to the distal tibia
1. Introduction
This approach lends itself to fracture patterns that are primarily displaced fractures of the posterior tibia with little or no involvement of the anterior tibial surface. It has the advantage of allowing fixation of both the fibula and tibia through the same incision. It is also useful when the soft-tissue injury prevents use of the anterolateral or anteromedial exposures. The patient is placed into prone or lateral position.
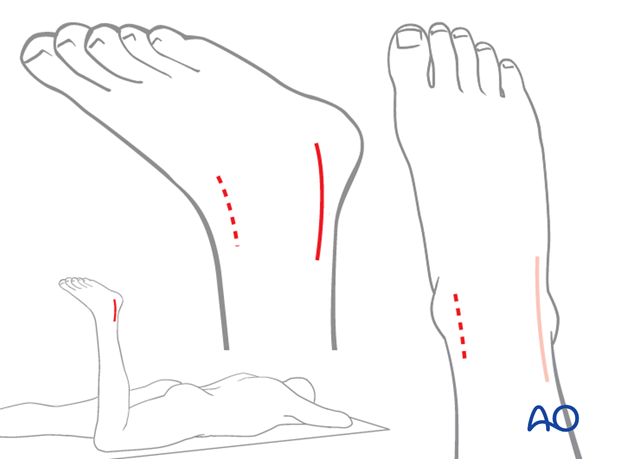
2. Skin incision
The skin incision is made along the posteromedial border of the fibula and can extend from the tip of the fibula as far proximally as is required. It should never be more medial than the lateral border of the Achilles tendon.
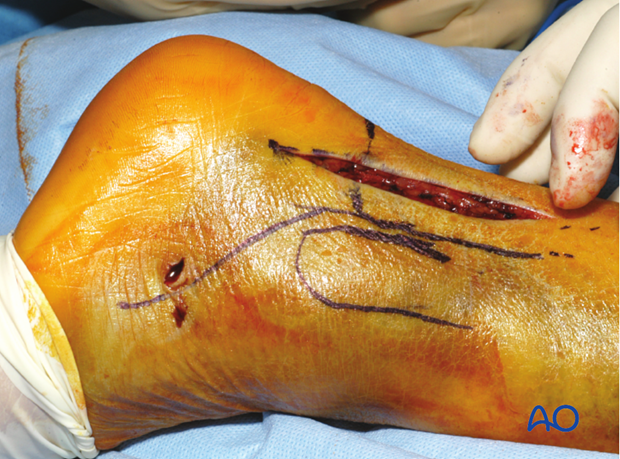
3. Protect the sural nerve
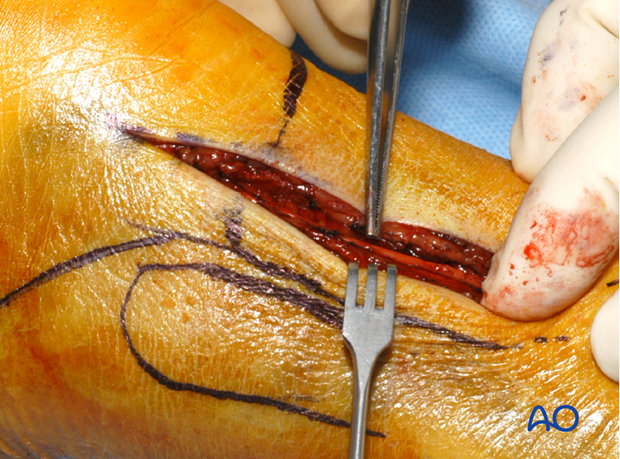
It is important to be aware of the course of the sural nerve as it courses from the posterior midline of the calf proximally to just posterior to the fibula distally.
The sural nerve is identified under the superficial fascial layer and it is usually included in the lateral flap. If the dissection is extended more proximally, it may be necessary to work on either side of this nerve.
4. Exposure of the fibula
Superficial surgical dissection to the fibula
If the fibula requires fixation, this option is chosen. Full thickness superficial flaps should be maintained to reduce the risk of skin necrosis.
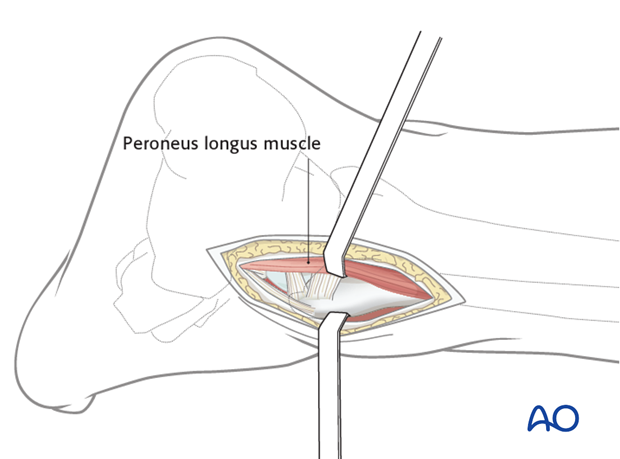
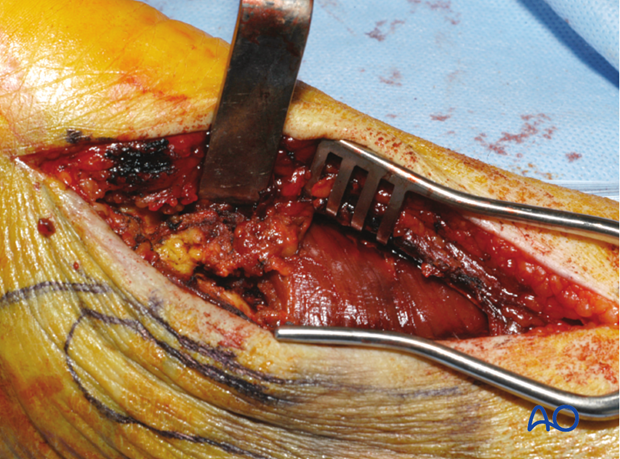
Superficial dissection should be taken down to the attachment of the peroneal fascia on the posterolateral border of the fibula. The fascia is incised, and the peroneal muscles are retracted medially.
Deep surgical dissection to the fibula
Exposure of the fibula is completed by releasing the posterior periosteum where the peroneal fascia inserts on the bone.
The fibular fracture fragments can then be reduced, preserving their soft-tissue attachments. The fibula reduction and fixation are usually completed before tibial exposure.

5. Approach to the tibia
Surgical dissection to the tibia
Access to the tibia is through a separate plane which is developed on the posteromedial border of the peroneal muscles. These are now retracted laterally.
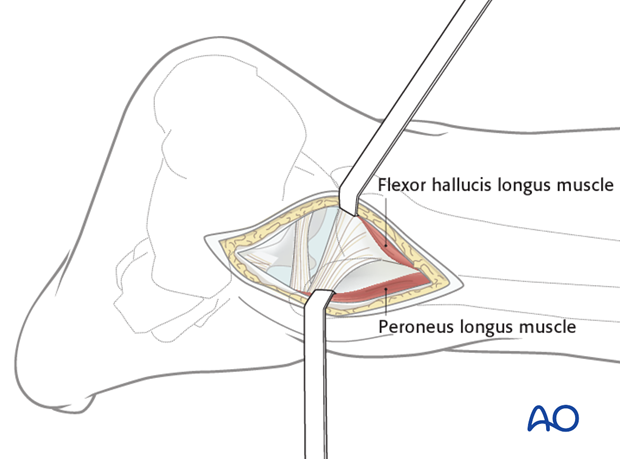
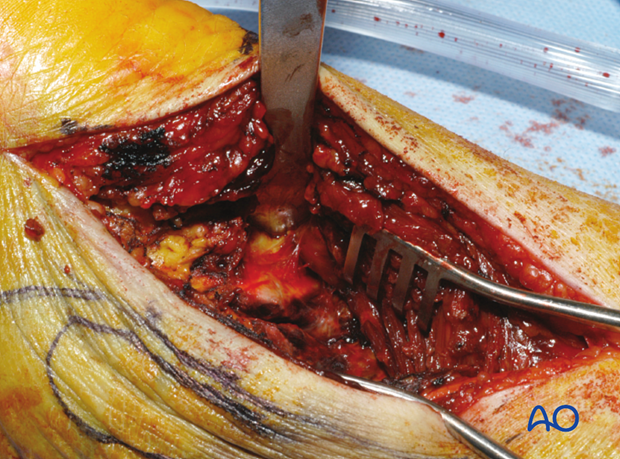
Exposure of the posterior aspect of the tibia is achieved by developing the interval between the peroneal tendons and muscles laterally and the flexor hallucis longus (FHL) medially.
Deep surgical dissection to the tibia
Flexor hallucis longus (FHL) is recognizable from the very distal extent of its muscle belly. It can also be identified by moving the great toe. With sharp dissection of the FHL along its lateral border, the entire posterior aspect of the tibial surface can be exposed by retracting this muscle medially. This also provides protection of the posteromedial neurovascular bundle.
Note: Either the peroneal artery and vein, or a significant branch, can be injured in this part of the exposure. If a tourniquet is used, it is wise to deflate the tourniquet before closing this layer to ensure hemostasis has been achieved.
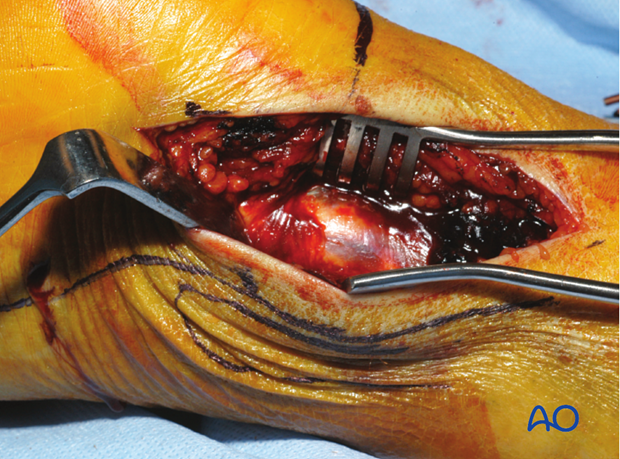
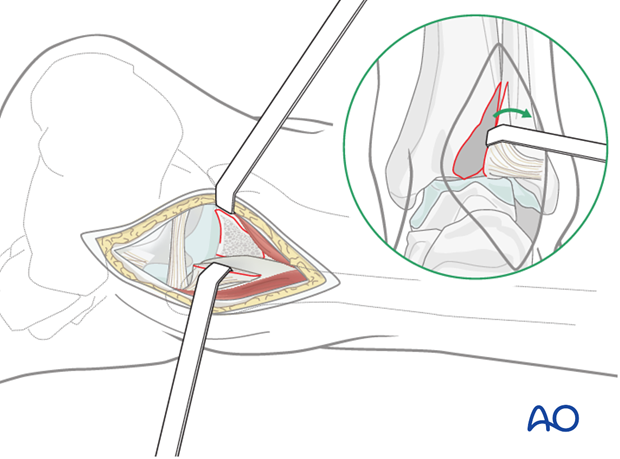
6. Tibia: Exposure of the joint surface
Visualization of the articular surface or small fragments preventing reduction of the articular pieces can be difficult.
The posterolateral fragment is rotated laterally around the usually intact posterior tibiofibular ligament. The interval between the bony fragments is developed giving access to the center of the fracture.
7. Access to other parts of the tibia
With prone positioning, this exposure can be used in combination with a medial exposure of the tibia without repositioning the patient. However, occasionally an anteromedial or anterolateral fragment will need to be exposed through a separate small incision. This can be achieved once provisional fixation and stabilization of the posterior tibia has been completed by flexing the knee to at least 90 degrees to allow access to the anterior part of the joint. This is sometimes also useful for placement of a reduction clamp as part of the surgical procedure.