ORIF - Buttress plate and lag screws
1. Single-stage or multiple-stage surgery?
Principles
The soft-tissue conditions usually dictate the choice of procedure: early single-stage, or multiple-stage surgery.
Displaced fractures with minimal, closed soft-tissue injury
(Tscherne classification, closed fracture grade 0, rarely grade 1)
Reconstruction may be done with a single-stage procedure, similar to the proposals of Rüedi and Allgöwer. This involves complete restoration of the ankle mortise including fibula and tibia. This may require bone grafting and usually a buttress plate. The goal is absolute stability of the joint surface, to permit early motion and achieve healing with anatomical alignment.
Grossly displaced fractures and / or fractures with moderate to severe closed soft-tissue injury
(Tscherne classification, closed fracture grade 2 or 3)
It is generally advisable to proceed in two or more stages:
- Closed reduction and joint bridging external fixation
- Definitive open reconstruction after 5-10 days (wait for the appearance of skin wrinkles)

Open pilon fractures
These are very severe injuries often requiring plastic surgery for soft-tissue reconstruction. The management includes the following stages:
Emergency management:
- Wound debridement and lavage
- Joint-bridging external fixation
- Fibular fixation may also be considered, but rarely adds benefit and may require another incision through badly injured tissue
- Open wound management with occlusive dressing (possible antibiotic bead pouch or vacuum dressing)
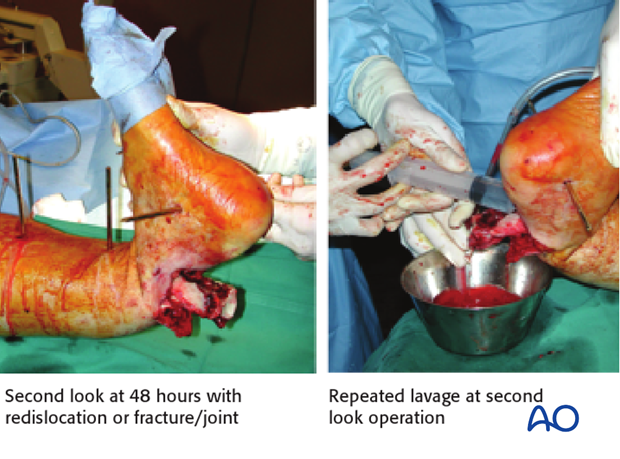
At 48 hours:
- Second look with repeated lavage (re-dislocation of fracture/joint!) and re-debridement if necessary
- Reconstruction of the tibial articular block
- Soft-tissue coverage, local or free flap, if possible. Significant delay of coverage increases infection risk
Definitive stabilization:
- Bridging of the metaphyseal comminution, with or without bone graft
- Definitive stabilization with internal or external fixation may be performed at 48 hours, or preferably later.
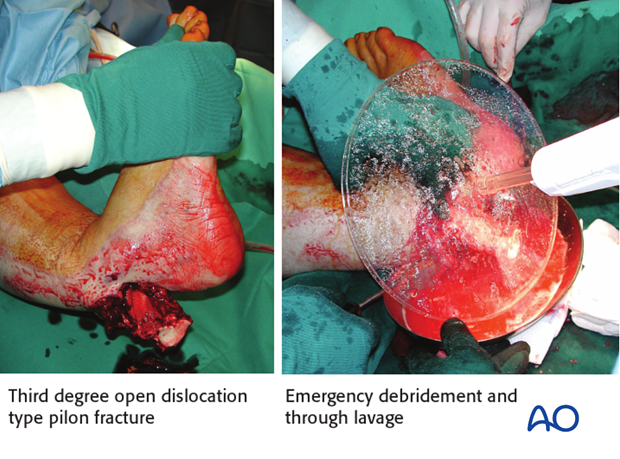
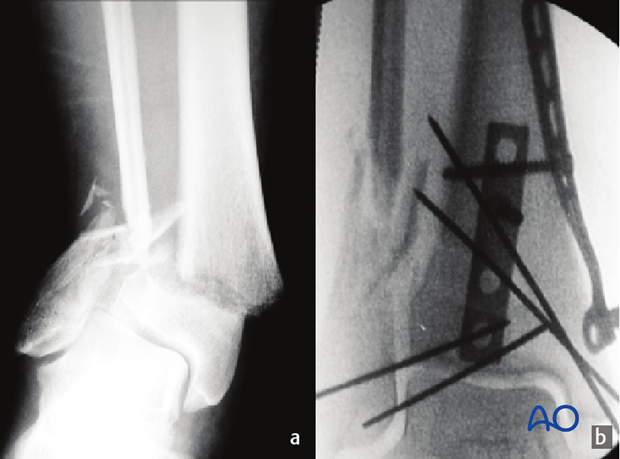
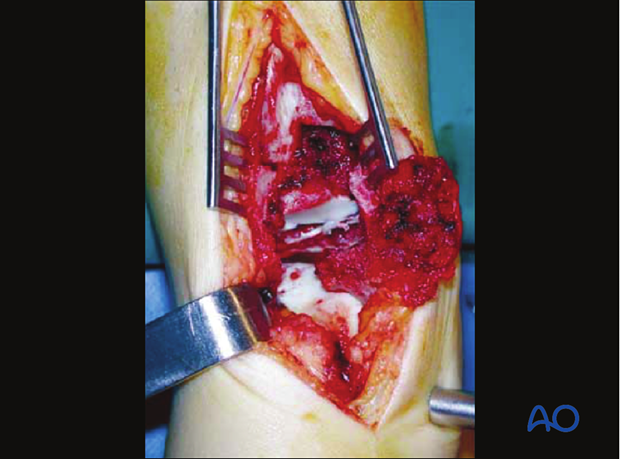
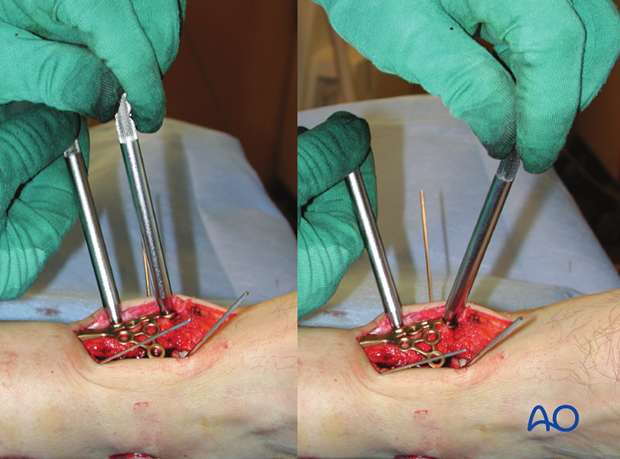
Image shows second look at 48 hours with redislocation of the fracture/joint and repeated lavage at second look operation.
2. Fibula or tibia first? Sequence of bone stabilization
Introduction
The ankle joint involves the tibial-fibular mortise and talus. If the fibula is not properly attached to the tibia, the joint will not be congruent. If there is a fibular fracture, it usually must be repaired. The surgeon must choose whether to do it first or later.
Simple fracture of the fibula
If the fibular fracture is simple, this fracture is fixed as a first step by open reduction and stable plate fixation. This indirectly reduces attached lateral fragments of the tibial articular surface through the usually intact syndesmotic ligaments. ORIF of the articular surface of the tibia and stable meta-diaphyseal fixation then follow.
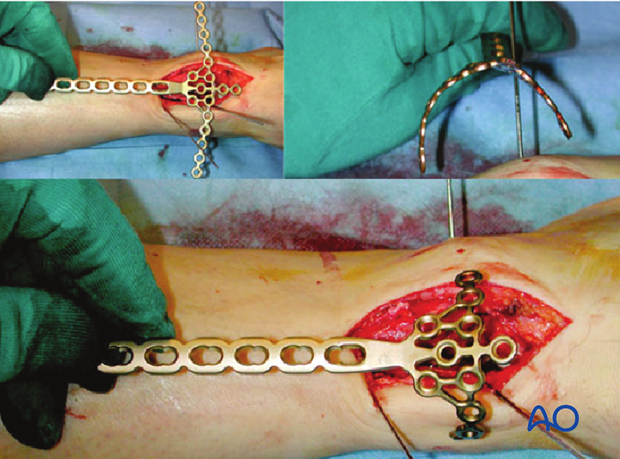
Multifragmentary fibular fracture
Comminuted fibular fractures (a) are difficult to reduce accurately. Any malreduction of the fibula will impede anatomic reconstruction of the tibia. In such cases it is usually better to reconstruct the tibia first and use the tibia and talus as guides for positioning the lateral malleolus, if necessary. This usually reduces the fibular fracture indirectly. Since the syndesmotic ligaments are usually intact, gross realignment of the fibula often occurs as the tibia is reduced (b).
The comminuted fibular fracture can often be stabilized with a subcutaneous plate, without exposing the fragments (c) using a long bridging plate (d). It is essential to achieve correct length, rotation, and axial alignment of the fibula.

3. Preoperative planning
Planning of reduction and fixation
Preoperative planning is an essential part of the treatment of all distal tibial fractures:
- Obtain good AP and lateral x-rays of both injured and uninjured side; CT if needed
- Careful study of the x-rays and CT scan
- Trace AP and lateral x-rays of normal side
- Identify the individual fracture fragments
- Draw the fracture fragments, reduced, onto the normal tracing
- Consider reduction techniques
- Choose and draw in fixation implants
- Choice of surgical approach
- Prepare list of operative steps
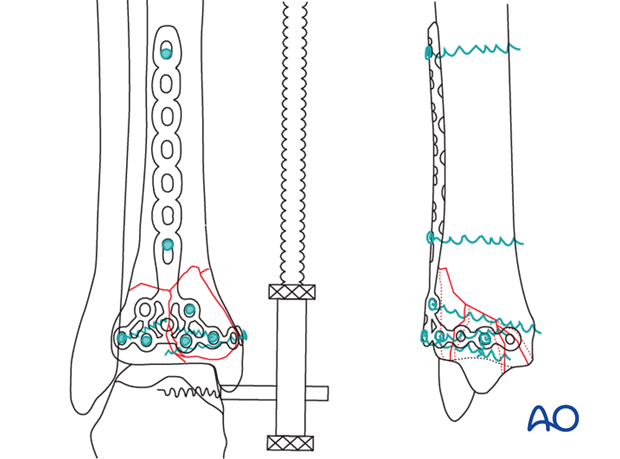
This anterior partial articular fracture requires open reduction through a limited anterior approach. Sufficient exposure is necessary for direct articular fracture reduction. Plate insertion proximally can be done subcutaneously.
For the reduction of all types of pilon fractures with displaced central fragments and/or impaction, the exact approach is most effectively planned from the axial CT scan. Depending on the fracture location and type, an anteromedial, anterolateral, or rarely posteromedial, posterolateral, or medial approach is required.
Ligamentotaxis does not reduce impacted central fragments. Direct manipulation with inspection of the joint is required. Therefore, at least a limited open approach is required for the reduction of the articular surface.

Partial articular fractures are usually fixed with lag screws and buttress plates without locking head screws. In the illustrated case, a locking distal tibial plate is selected.
Interfragmentary compression will be applied first with a conventional cortex screw. Locking head screws will then be inserted to maintain stability, while avoiding periosteal compression. Other options involve use of traditional plates. The drawing illustrates the planned final construct.
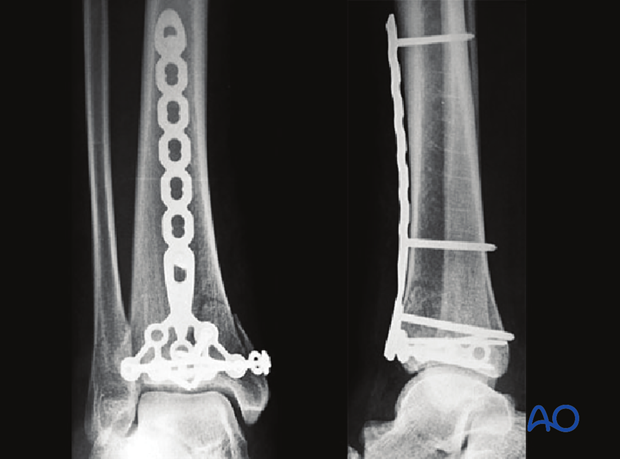
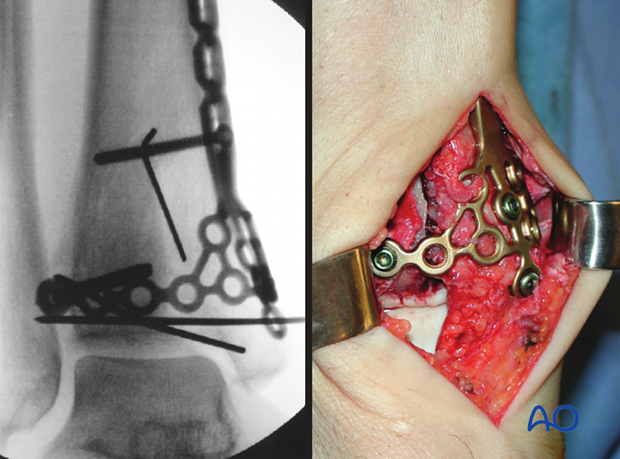
Executed final construct.
4. Patient preparation
Depending on the approach, the patient may be placed in the following positions:
5. Reduction
Application of a large distractor
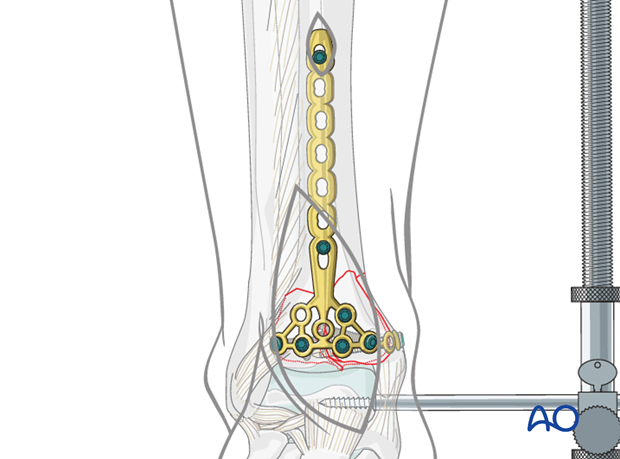
A distractor or external fixator is a very helpful tool for reduction. Medial positioning allows subcutaneous access to the tibia. A laterally based distractor requires a pin through the anterior muscular compartment but provides more efficient distraction of any associated fibular fracture, and correction of valgus deformities. Distraction can be used for open reduction and plate fixation of the fibula as first step and for the reduction and visualization of the articular surface of the tibia as a second step.
Schanz screws are positioned in safe zones of the tibial shaft and talar neck (or the calcaneal tuberosity). In case of previously applied joint-bridging fixator, the same Schanz screws can be used, but distraction applied directly to the talus provides the best control.
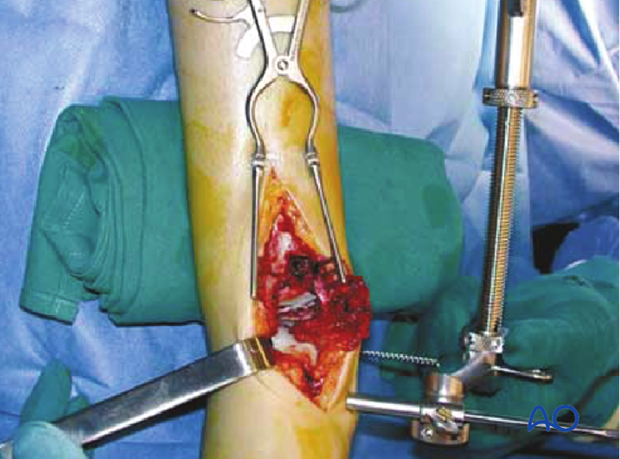
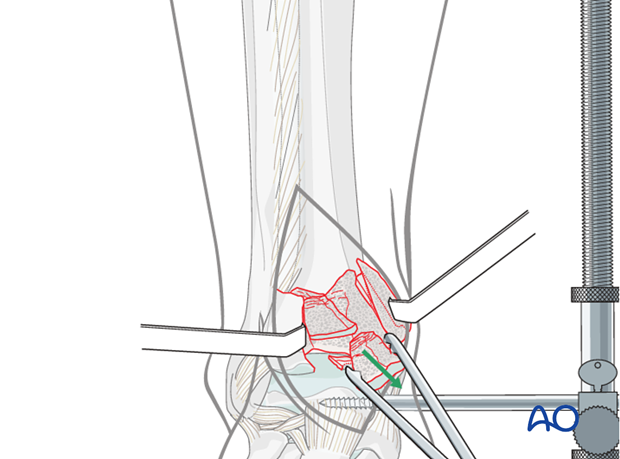
Exposure and cleaning of fracture area
The fracture zone is opened by separating the anterior fragments through the sagittal fracture line. The joint is washed out and freed from blood clots and small intraarticular osteochondral debris. Inspect and document any cartilage damage on the talar dome. The central part of the fracture with impacted fragments is now visible.
The large central fragment is removed and temporarily set aside.
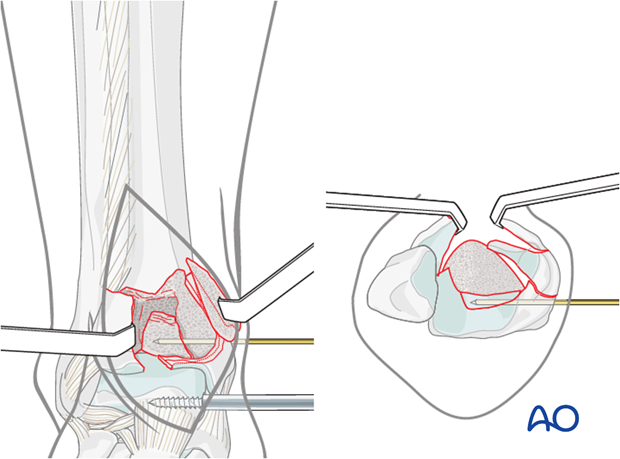
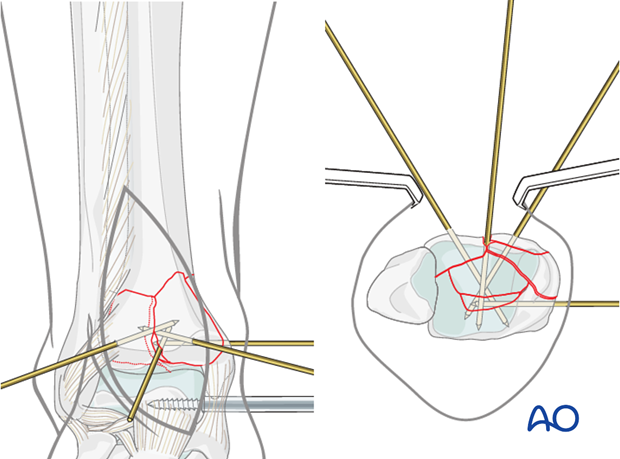
Reduction of posterocentral part
The central fracture lines are cleaned. The small impacted posterocentral fragment is reduced anatomically to the posterior joint rim under visual control. It is important to reduce any impaction of the most posterior fragment, if present, or joint surface visualized on lateral imaging before beginning reconstruction of the more anterior parts of the joint.
If the posterocentral fragment does not stay in place on its own, it has to be fixed either by a resorbable pin, or a temporary K-wire which is inserted through the posterior part of the medial malleolus, as shown in the illustration.
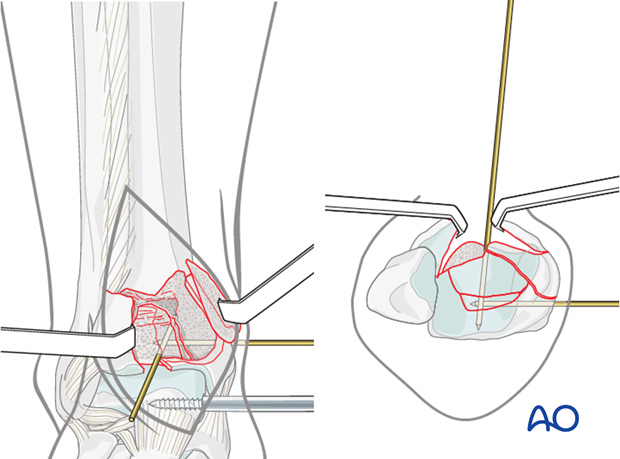
Reduction of central fragment
The large impacted fragment, that had previously been removed, is reduced anatomically to the posterocentral fragment.
A K-wire is inserted from anterior to posterior, or from medial to lateral to hold the reduction. Occasionally, it is necessary to cut off this K-wire and leave it in situ to maintain the articular surface reduction (“lost K-wire”).
Finish reduction
The anteromedial and anterolateral fragments are rotated back into their anatomical positions. This may require at least partial release of the distractor, since these fragments can be under tension from the joint capsule. The anteromedial and anterolateral fragments are held in their anatomic position with the help of a Weber clamp. K-wires are inserted for temporary stabilization. The correct reduction is assessed and documented by fluoroscopy. See also the content on assessment of reduction.
Bone graft could be inserted if necessary before reduction of the peripheral fragments. In the illustrated case, with good bone quality and quite large main articular fragments, it was not necessary.
6. Plate fixation - choice of implant
Choice of implant
In the illustrated case, a short LCP pilon plate 2.7/3.5 was planned for fixation. Other options would be a cloverleaf plate 3.5, a small T-plate 3.5 (conventional or locking), or two or more small plates (one-third or one-quarter tubular).
Periarticular plates are manufactured to fit different surfaces of the distal tibia. They still typically require final adjustment of contour.
Example of ORIF with a cloverleaf plate 3.5
Partial articular fractures are usually fixed with lag screws and buttress plates without locking head screws. The standard traditional plate is the cloverleaf plate 3.5, which can be placed medially, anteromedially or anteriorly, depending on the fracture pattern. As shown here, the distal tab of the plate can be removed so it doesn’t interfere with the joint.
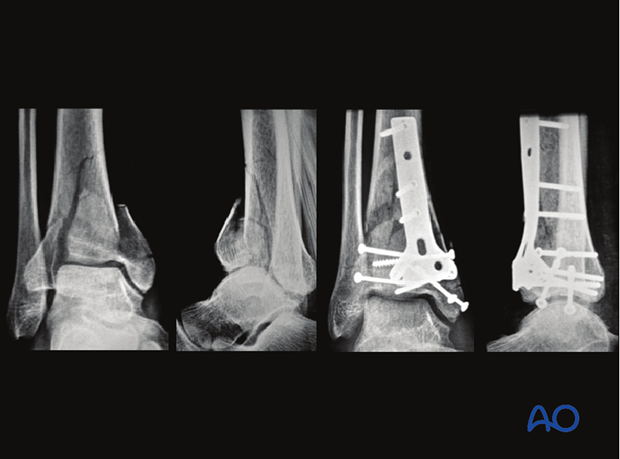
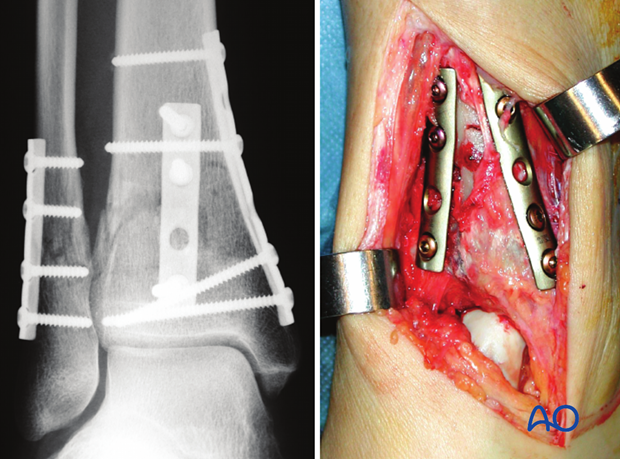
Example of ORIF with two one-third tubular plates
The illustration shows an example with a double plate technique for the distal tibia, using two one-third tubular plates, applied through an anteromedial approach, and another one-third tubular plate for the fibula.
7. Plate insertion
Plate preparation
In our example, the LCP pilon plate 2.7/3.5 was cut to fit the fracture and local anatomy. Periarticular plates are manufactured to fit different surfaces of the distal tibia. They still typically require final adjustment of contour.
The lateral branches of the plate are bent to hold the anterolateral and anteromedial fragments to fit the bone. The shaft of the plate should be contoured so that the middle part is not touching the bone. This will allow additional interfragmentary compression as the plate is tightened using a conventional screw before any locking head screws.
Proximal tunneling is performed with a blunt instrument. The prepared plate is inserted.
Depending on the fracture situation, the plate might be positioned on the anteromedial aspect, or much less frequently, on the anterior crest of the tibia.
K-wires can be cut 5-10 mm above the bone surface, if needed, to allow proper plate positioning. If this is not possible, the K-wires are replaced and then the plate is applied.
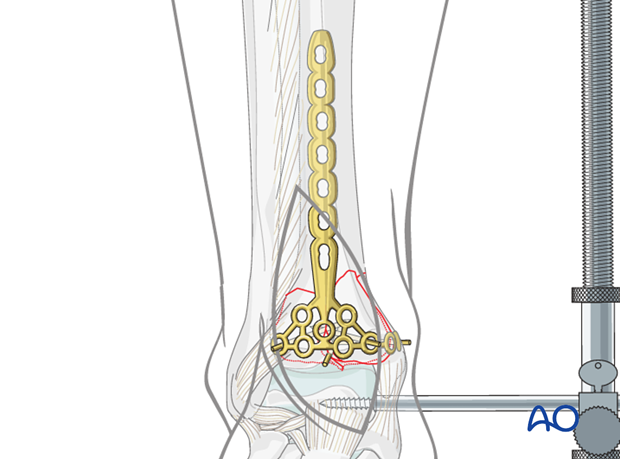
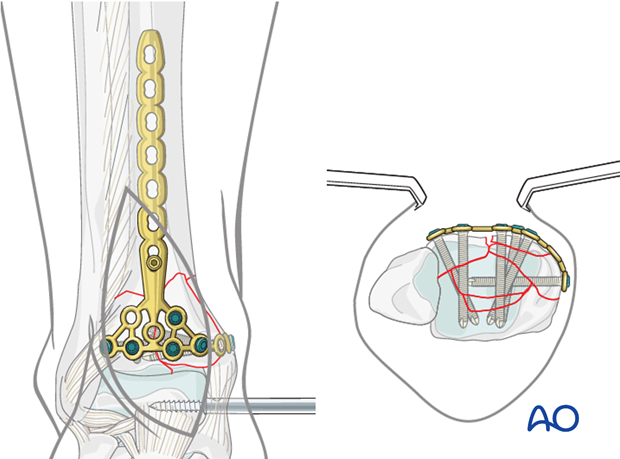
Illustration shows the LCP pilon plate 2.7/3.5 positioned on the anteromedial aspect of the tibia.
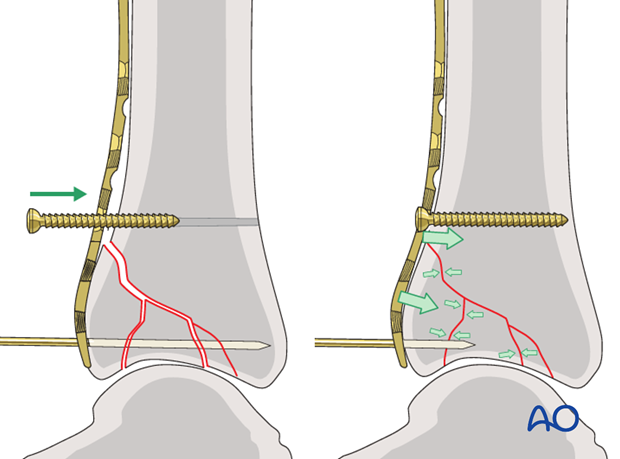
8. Compressing the plate
The undercontoured plate is compressed against the bone to add stability. A 3.5 mm cortex screw is inserted proximal to the fracture and tightened to compress the fragments with the inferior end of the plate. A locking head screw would not provide this compression.
9. Definitive fixation of the articular block
One or two lag screws can be inserted to increase interfragmentary compression before the first locking head screw is used on the plate.
Interfragmentary lag screws may be essential for articular fragment stabilization. They can be inserted either outside or through the plate. See also the additional material on lag screw principles.
Locking head screws are inserted into the joint block to hold the anatomical reduction in place. K-wires are removed stepwise as required for screw application. Using smaller diameter screws may allow better access for fixation (2.7 mm instead of 3.5 mm).
Note: Screws may intersect during insertion. The plate can be slightly twisted to avoid screw interference.
Pearl – fine contouring of the plate
Two bending bolts can be used to contour the side branches of the plate to:
- Precisely match bone anatomy
- Allow proper screw crossing
Fixation of anterolateral fragment
In case of a screw application through the center of the Tillaux-Chaput fragment, a small separate anterolateral incision might be necessary. Care has to be taken not to damage the superficial peroneal nerve.

10. Definitive plate fixation
Proximal plate fixation
A screw is inserted into the most proximal hole of the plate through a stab incision.
In osteoporotic bone additional screws, including locking screws, can be used.
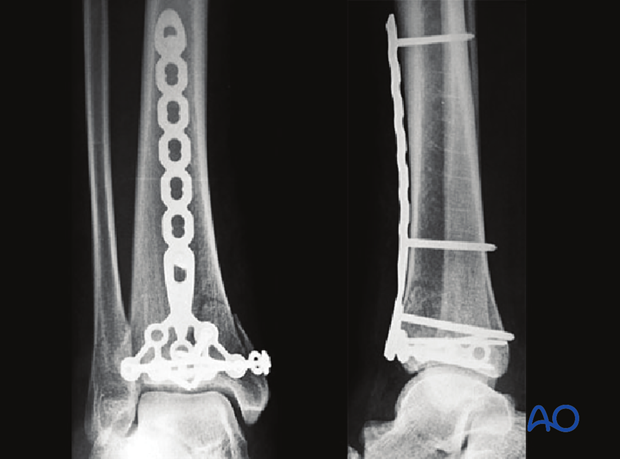
11. Final assessment
Radiographic documentation of joint congruity, length of tibia and fibula, and axial alignment is mandatory performed. This final operative x-ray confirms the anatomical reduction and the correct position of the plate and screws. See also the content on assessment of reduction.
The wound is closed in layers over the plate and fracture.
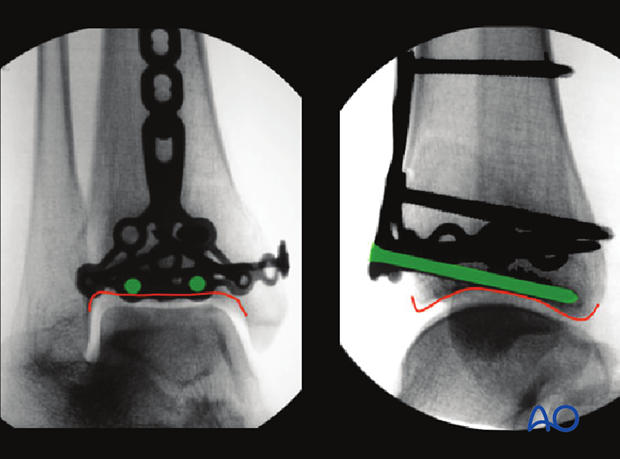
Pearl - Exclude articular penetration of screws
It is important to radiographically check that the screws do not enter the joint.
An x-ray aimed along the screws helps to show, as it does here, that they do not penetrate the articular cartilage. This is confirmed also by a perfect lateral X-ray tangential to the subchondral bone, as shown here.
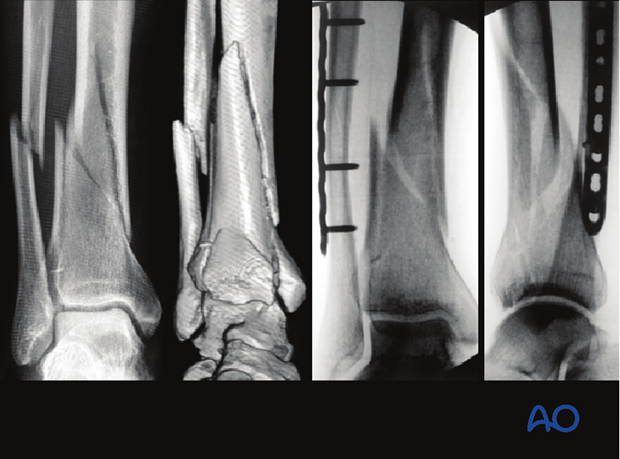
12. X-ray follow-up at 3 months
Image shows x-ray follow-up of the presented case at 3 months.

13. Aftercare following plating
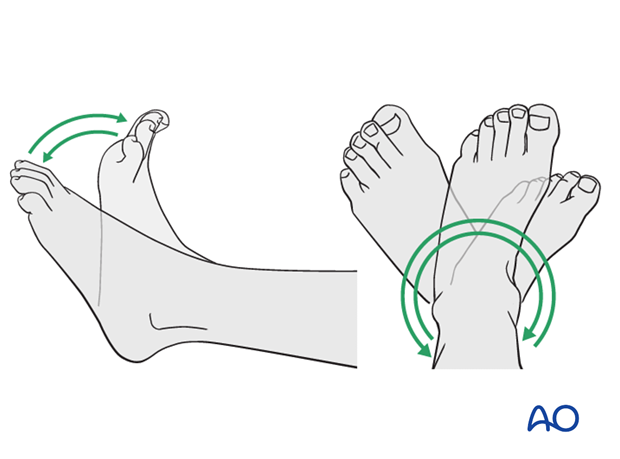
Leg elevation is recommended for the first 2-5 postoperative days. Physiotherapy with active assisted exercises is started immediately after operation. Immobilization is not necessary.
Mobilization
Starts depending on the wound healing with flat footed, weight of the leg weight bearing (10-20kg).
Follow up
Clinical and radiological follow-up is recommended after 2, 6 and 12 weeks. Depending on the consolidation, weight bearing can be increased after 6-8 weeks with full weight bearing usually after 3 months. Supervised rehabilitation with intermittent clinical and radiographic follow-up is advisable every 6-12 weeks until recovery reaches a plateau, typically 6-12 months after injury. Weight-bearing radiographs are preferable to assess articular cartilage thickness. Angular stable fixation may obscure signs of non-union for many months.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implant (plate and/or isolated screws). The best time for implant removal is after complete remodeling, usually at least 12 months after surgery.