Open reduction internal fixation
1. Introduction
Principles
For elbow dislocations with fracture of the radial head with or without fracture of the coronoid the following principles apply:
- The risk of re-dislocation is minimized by fixation or replacement of the radial head, reattachment of the lateral collateral ligament to the lateral epicondyle, and if need, coronoid fracture fixation.
- As long as the elbow remains located, the medial collateral ligament will heal and does not need to be repaired.
- If repair of the radial head, coronoid, and LCL does not prevent redislocation, the surgeon can consider repairing the MCL, applying an external fixator or cross pinning the elbow joint.
- The coronoid fracture is typically small and transverse and has the anterior elbow capsule attached. The most common fixation technique is suture lasso.
- Restoration of radiocapitellar contact is a key aspect of elbow stability, whether this is done by repairing the radial head (ORIF) or with prosthetic replacement.
2. Positioning
The patient is placed in a supine position with the arm on the table. If available, a sterile tourniquet may be advantageous as it increases the surgical field.
3. Approaches
Skin incision
Both the medial and lateral sides can be reached via a posterior incision because large medial and lateral skin flaps can be made. Alternatively, separate medial and lateral incision can be employed.
Exposure of the radial head fracture is facilitated by the LCL injury.
There may be a disruption in the fascia indicating where to make an interval.
If there is no traumatic fascial disruption available in the fascia, either a Kocher or Kaplan approach can be used.
Kaplan
A fascial incision at the equator of the capitellum which is roughly at the EDC/ECRB interval is advantageous because it protects the lateral collateral ligament.
Less important to know which muscle insertion you are releasing than where you are with respect to the LCL.
Kocher
Usually people describe using Kocher interval. Advantage is that fragments go posterior.
Disadvantage: Could further damage the LCL and it is difficult to get access to the fragments that displace posteriorly.
Coronoid approach from the lateral side
Exposure of the coronoid fracture is facilitated by moving or removing the radial head fragments. The best exposure is made in cases where the radial head is excised and the coronoid fixed. Prosthetic replacement of the radial head is performed subsequently.
Radial head exposure
Exposure of the radial head is improved by releasing the origin of the ECRL from the supracondylar ridge and elevating the brachialis from the anterior humerus. It may also help to split the supinator distally for a few centmeters.
4. Elbow dislocation with radial head or neck fracture only
Sequence of repair
The first step is exposure the radial head/neck to determine if it can be repaired or needs to be replaced.
When the radial head is fragmented into more than 3 fragments (more than the neck and two articular fragments), the radial head is excised and replaced by a prosthesis.
The following sequence of fixation is used:
- Fixation or replacement of radial head or neck
- Repair of ligament injury
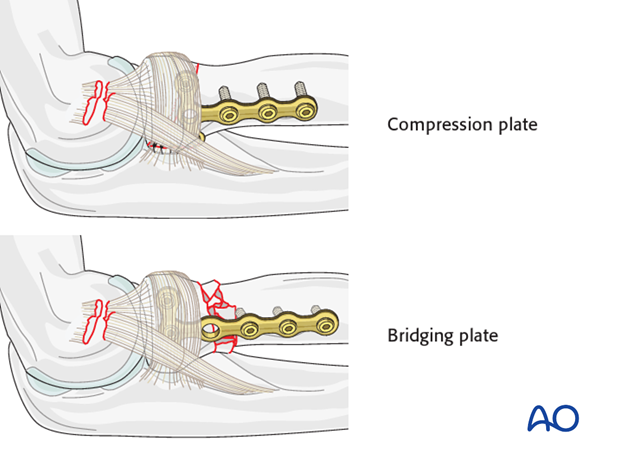
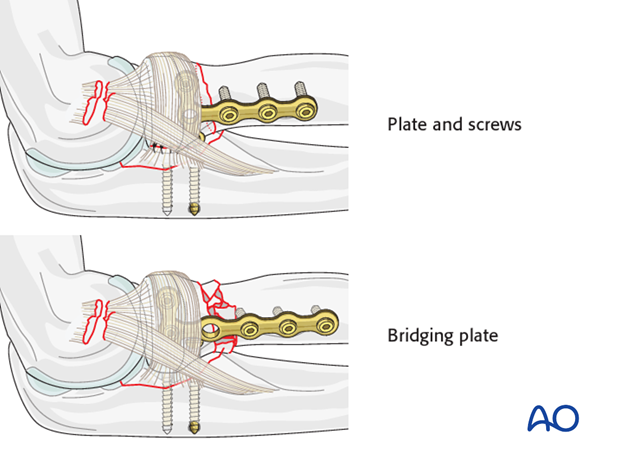
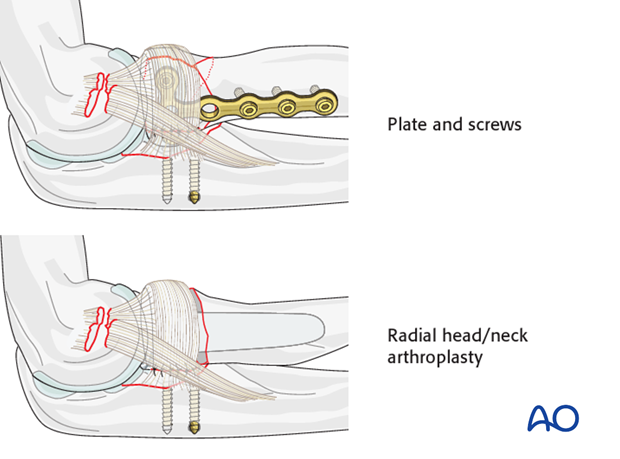
Radial neck fractures
If there is a fracture of the radial neck, repair with a plate and screws.
The treatment options are:
- Transverse fracture: Compression with T-plate and screws
- Multifragmentary fracture: Bridge plate
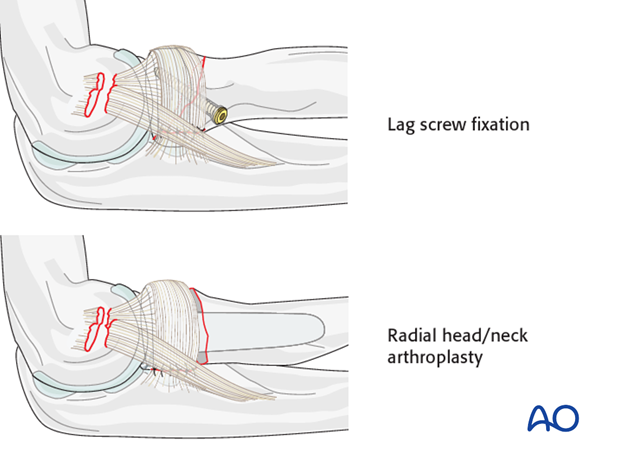
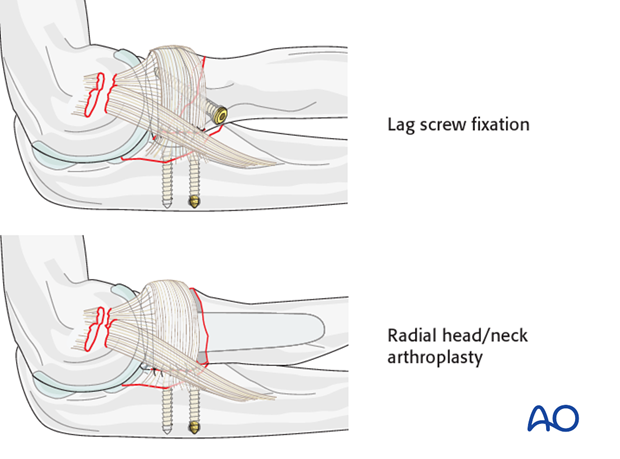
Partial articular radial head fractures
If there is partial articular fracture consisting of 1-2 fragments, screw fixation is used.
For greater fragmentation (> 3 fragments including the intact head) the radial head is excised and replaced by prosthesis.
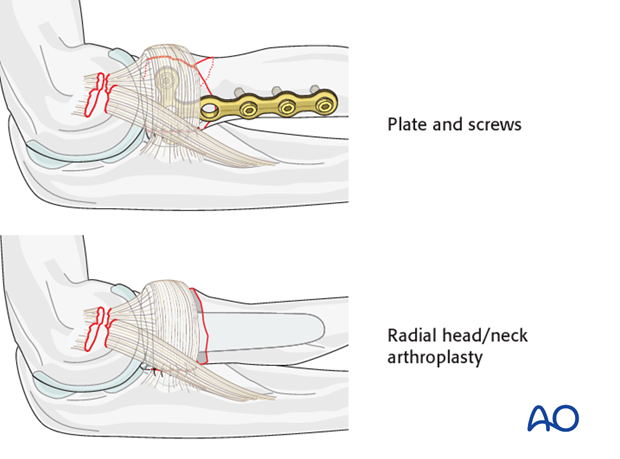
Complete radial head fractures
A complete articular fracture consisting of 3 or fewer fragments, large enough to warrant repair, plate fixation is performed.
If comminution exceeds 3 fragments, the head is not salvageable and should be replaced.
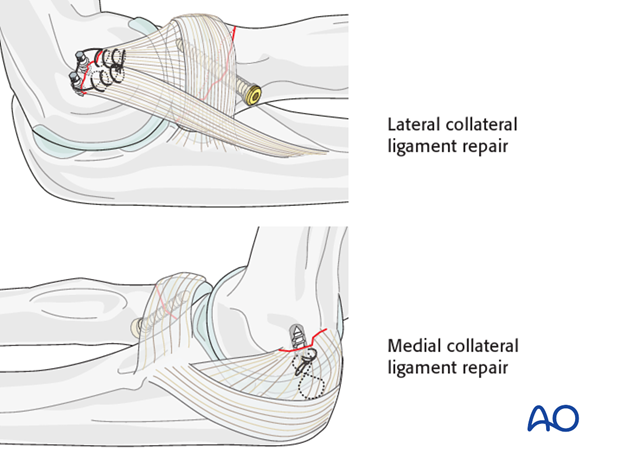
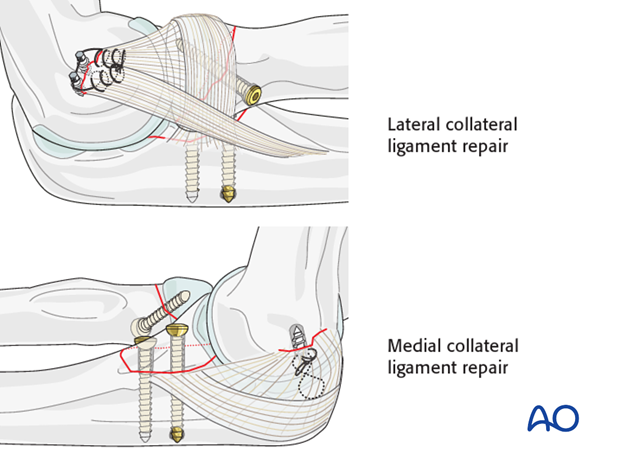
Ligament repair
Once the radial head/neck is either fixed or replaced, the collateral ligament injury is address by either suture anchors or sutures through drill holes:
For medial collateral ligament repair, a posterior midline incision with a medial flap can be used.
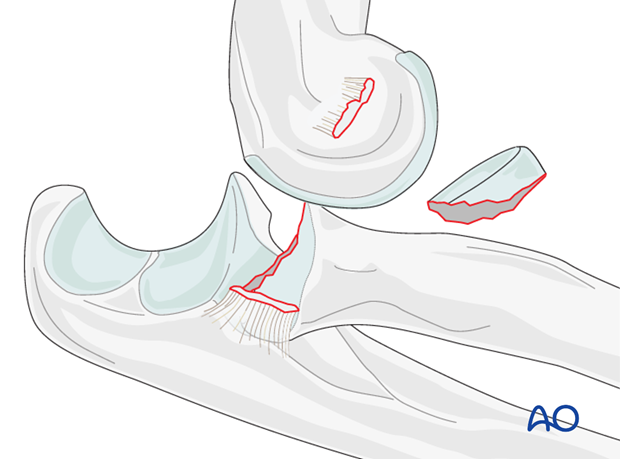
5. Terrible triad (Elbow dislocation with radial head/neck, coronoid fracture, and lateral collateral ligament disruption)
Sequence of fixation
The following sequence of fixation is used:
- Mobilization of the radial head fragments and fixation of coronoid fracture
- Fixation or replacement of radial head or neck fracture
- Reattachment of the LCL origin to the lateral epicondyle
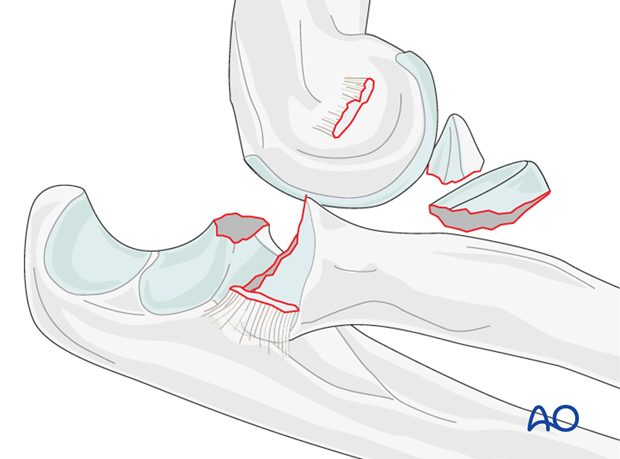
Coronoid fixation
There is some debate whether small coronoid fractures always need to be repaired, but there is no debate that repair is easiest as a first step before radial head management, when exposure is best.
If one decides to repair the coronoid fracture, move the radial head fragments aside (usually they have little or no soft tissue attachment and can be removed); repair the coronoid with screws for large fragments and sutures for small fragments.
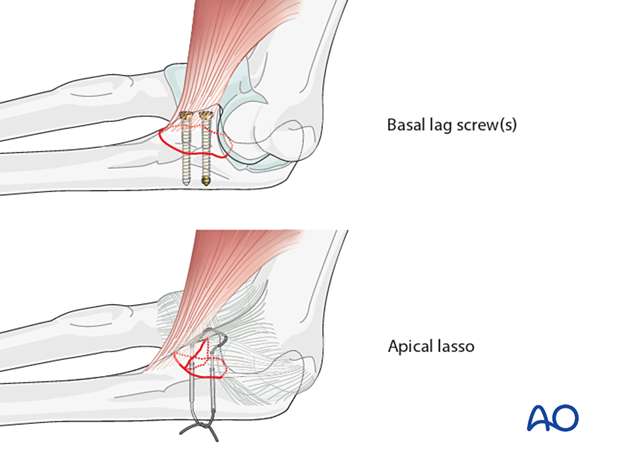
Radial neck fractures
If there is a fracture of the radial neck, repair with plate and screws. The treatment options are:
- Transverse fracture: Compression with T-plate and screws
- Multifragmentary fracture: Bridge plate
Partial radial head fractures
If there is partial articular fracture consisting of 1-2 fragments, screw fixation is used.
For greater fragmentation (> 3 fragments including the intact head) the radial head is excised and replaced by a prosthesis.
Complete radial head fractures
A complete articular fracture consisting of no more than 3 large fragments, plate fixation is performed.
If comminution exceeds 3 fragments, the head is not salvageable and should be replaced.
Ligament repair
Once the radial head/neck is either fixed or replaced, the collateral ligament injury is address by either suture anchors or sutures through drill holes:
For medial collateral ligament repair, a posterior midline incision with a medial flap can be used.
6. Intraoperative control of joint stability
After the repair is completed, make sure the elbow does not dislocate or subluxate in full gravity extension with the forearm in neutral. Check under image intensification using a lateral view in this position.
When the MCL has not been repaired, there is no point in testing valgus stability—we expect instability, but that does not mean that the elbow will dislocate or the MCL won’t heal.
If repair of the radial head, coronoid, and LCL does not prevent subluxation or redislocation in full gravity extension, the surgeon can consider repairing the MCL, applying an external fixator, cross pinning the elbow joint, or applying an internal joint stabilizer (internal hinge).
7. Postoperative treatment following ORIF
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
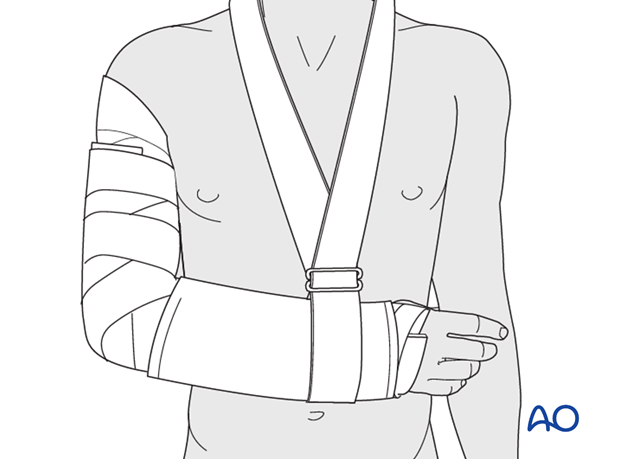
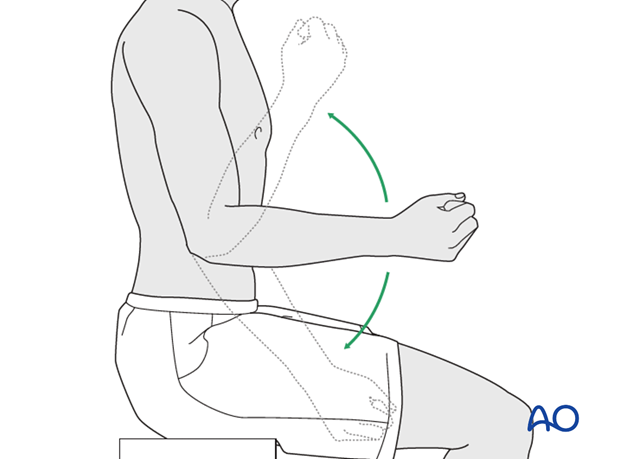
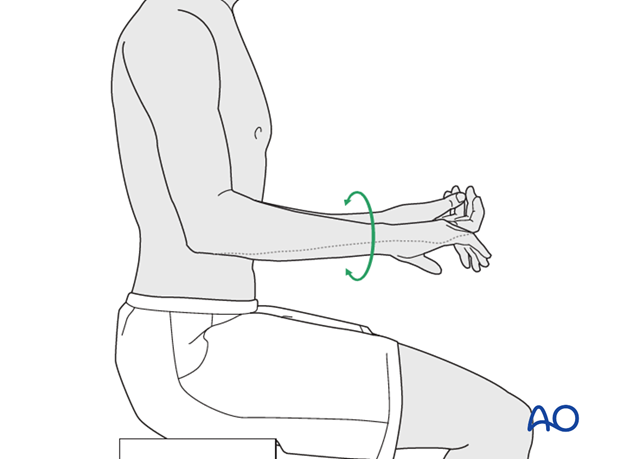
Mobilization
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













