Diaphyseal fixation using long tapered stem
1. Principles
The most critical criterium is to achieve rigid stem fixation in the distal fragment.
Proper reduction of the two major fracture fragments for rotation and length is equally important.
These principles should be followed when using modular and non-modular tapered stem designs.
2. Approach
The surgeon should use the surgical approach that is the most familiar to him/her for any total hip arthroplasty, such as:
- Anterolateral approach
- Direct anterior approach
- Iliofemoral (Smith-Petersen) approach
- Posterolateral approach
- Trochanteric osteotomy
- Extended trochanteric osteotomy
An extensile approach is necessary to access the fracture site for reduction and placement of additional fixation devices, such as cerclage wires, cables, strut graft, and/or plates.
These approaches can be performed with the patient in a lateral or supine position.
3. Implant removal
Acetabular cup assessment
Following adequate exposure into the hip joint, the surgeon should assess the position and the fixation stability of the acetabular cup.
The accepted "safe zone" is:
- cup inclination 40° to 55° (a)
- cup anteversion 20° to 40° (b)
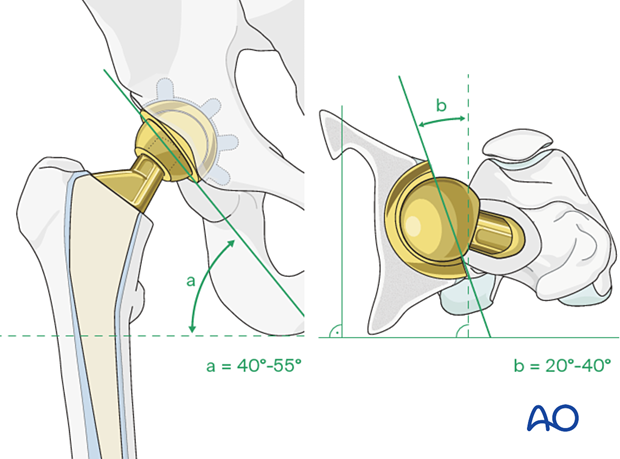
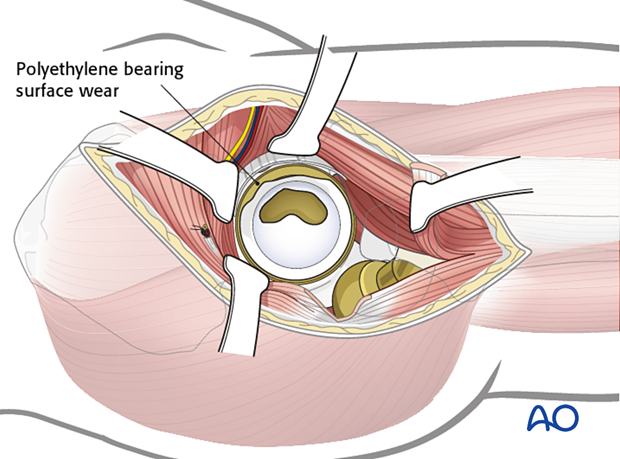
The surgeon should also assess for liner wear. If there is significant wear, liner revision should be done.
Femoral stem removal
The surgeon must perform adequate soft tissue releases around the proximal femur in order to reduce further fracture displacement or comminution.
It is critical to maintain the integrity of the hip abductor mechanism, in order to avoid abductor insufficiency.
The femoral component is removed. Details on how to remove a femoral stem are described in the basic technique for femoral stem removal.
The surgeon must minimize any additional damage to the host bone during the stem removal process.
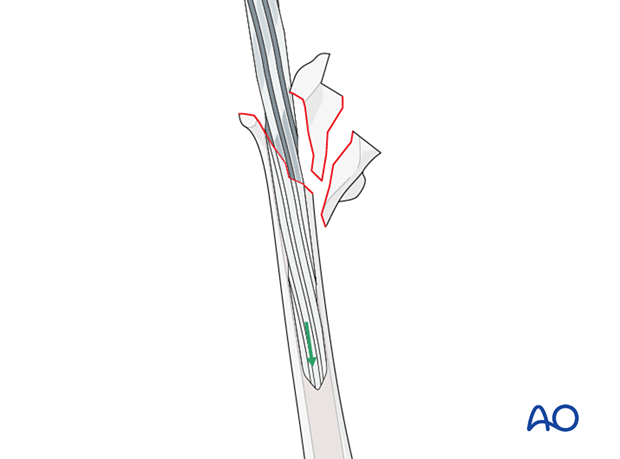
4. Provisional fracture reduction and fixation
General considerations
If the proximal femur fragment is comminuted, the surgeon can initially prepare the distal fragment. The proximal comminuted fracture fragments can later be reduced to the new femoral stem.
5. Femoral preparation
Implant selection
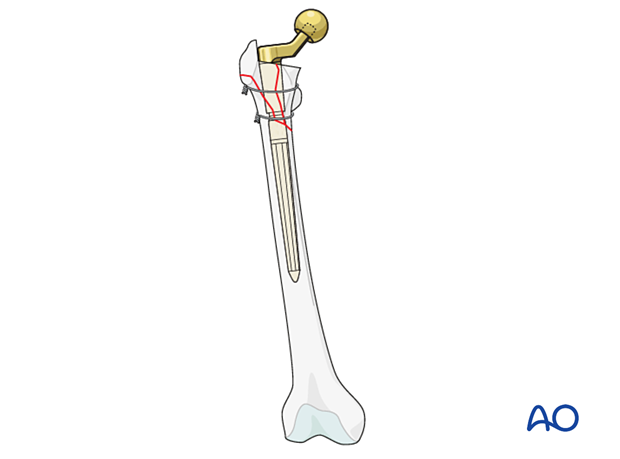
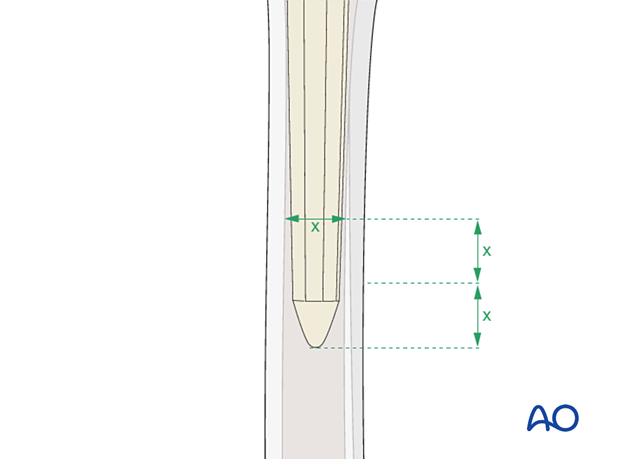
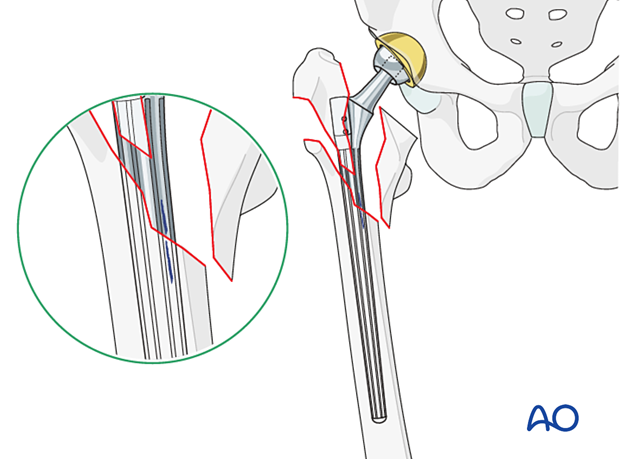
The new femoral stem must be of sufficient length to achieve rigid axial and rotational fixation into the distal diaphyseal femur fragment.
In general, the recommendation is a minimum length of two times the diameter of the femur below the fracture site. This length should be at least 4 to 6 cm of stem-to-cortex engagement in the distal fragment.
The diameter of the new stem is determined by the fit and rigidity of the reamer during the femoral preparation.
These are the general guidelines for femoral stem revision. Each implant manufacturer has specific recommendations and surgical technique for the specific device.
Femoral canal reaming
Femoral canal reaming is done using the reamer system from the specific device manufacturer.
The surgeon should ream in sequence, from the smallest diameter reamer to the largest diameter reamer that would achieve ideal stable fixation of the new stem. This is performed based upon both preoperative templating and intraoperative fit of the reamer.
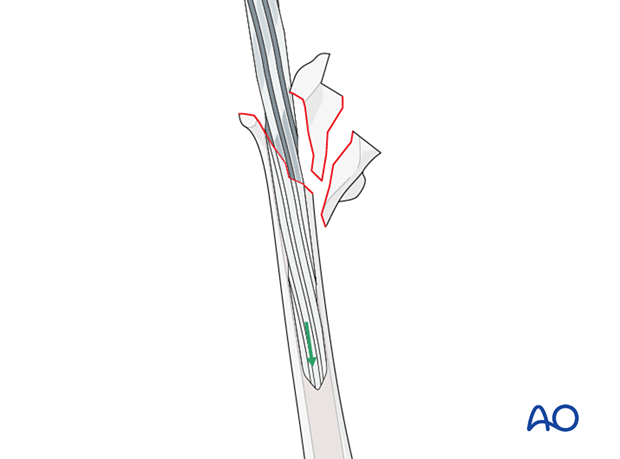
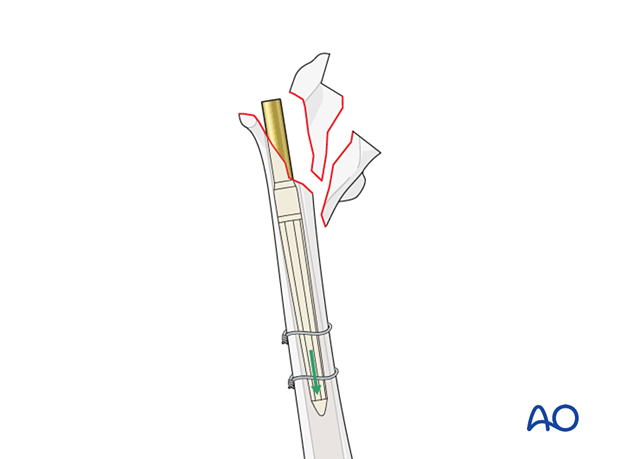
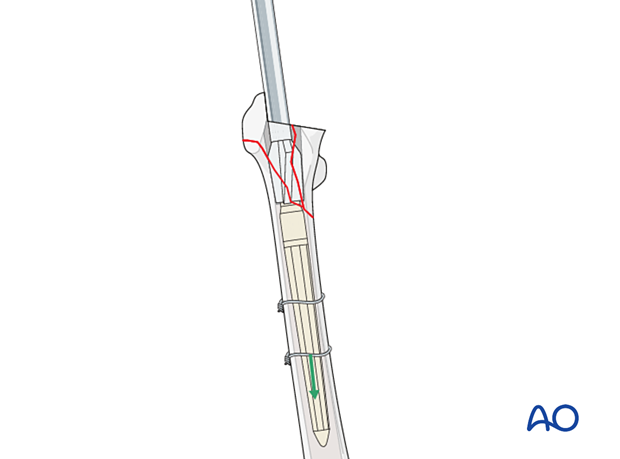
Distal fragment protection
The distal fragment should be protected with clamps or provisional wires/cables during the reaming process to avoid further fractures or comminution.
6. New implant insertion
The surgeon has the option of using a modular or nonmodular stem.
Select the proper stem size based upon the reaming.
Non modular stem insertion
If a nonmodular stem is selected, proper stem alignment must be achieved at this point.
A trial stem is inserted, and the hip is reduced to assess leg length, rotation, alignment of the limb, and hip joint stability. It is critical to mark the trial position prior to its removal.
The final stem is inserted guided by the previously made markings.
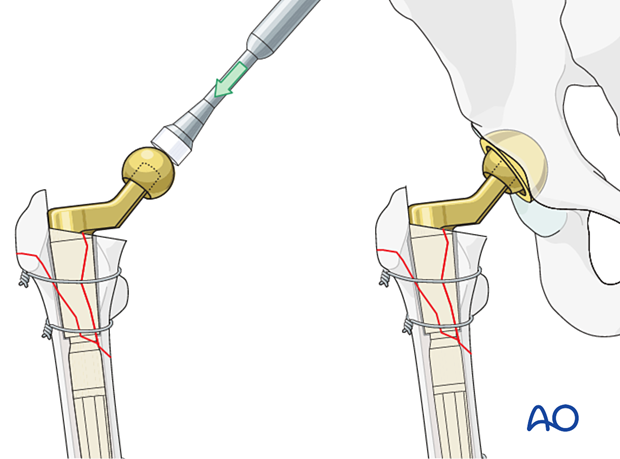
Modular stem insertion
The stem is inserted into the distal fragment to the appropriate level, using the dedicated stem inserter. Correct rotation is not determined at this time.
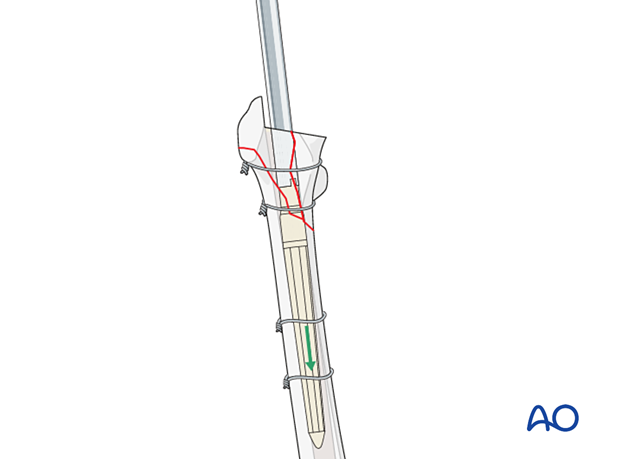
Following distal stem insertion, proximal femoral reaming is performed using the cannulated instruments. This can be performed with or without the proximal bone fragments reduced.
The diameter and the height of the proximal body is determined by preoperative templating, intraoperative reamer fit and rigidity.
A trial proximal body is inserted, and the hip is reduced to assess leg length, rotation, alignment of the limb, and hip joint stability. It is critical to mark the trial position prior to its removal.
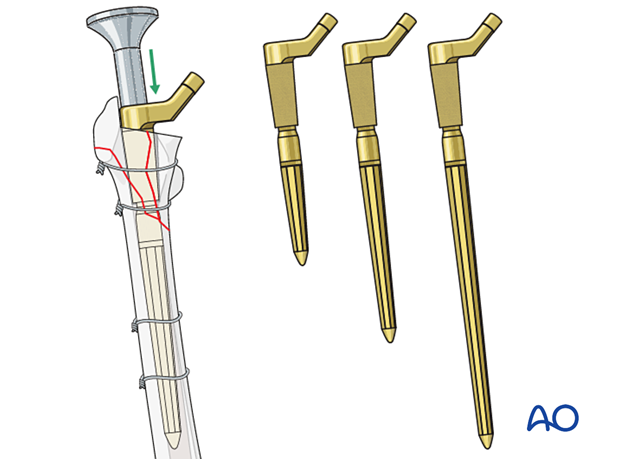
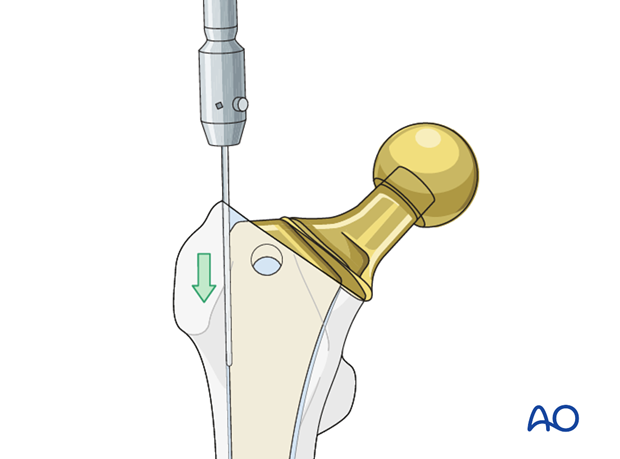
Proximal body insertion
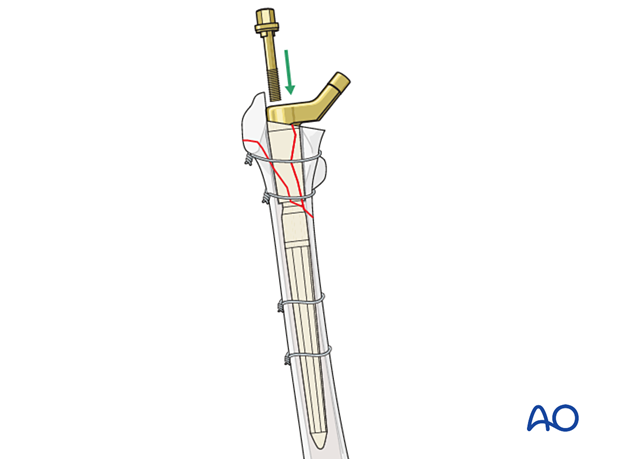
The final proximal body is inserted guided by the previously made markings to engage the distal stem.
The surgeon must be certain that proper and secure engagement between the two device components has been achieved.
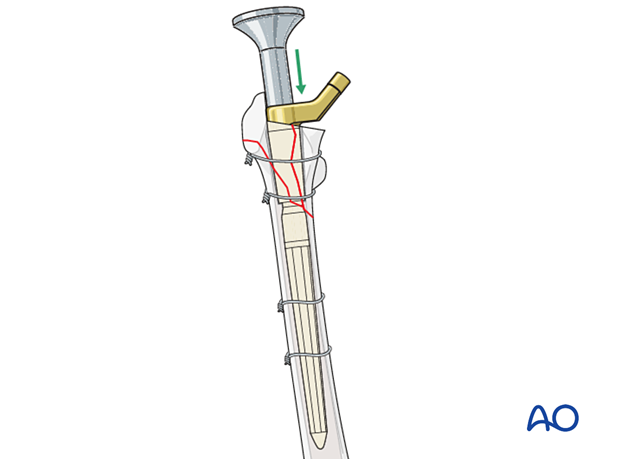
The supplemental screw/bolt for secure engagement at the taper junction between the proximal body and the distal stem is inserted and secured according to the manufacturer's specifications.
Hip reduction
The surgeon should do a trial reduction.
With the hip reduced, confirm the range of motion, leg length, and hip stability. Adjust the neck length if necessary.
Once satisfactory, attach the definitive femoral head to the stem, and reduce the hip. Confirm complete reduction, stability, and range of motion.
7. Final fracture reduction and fixation
Anatomic reduction verification
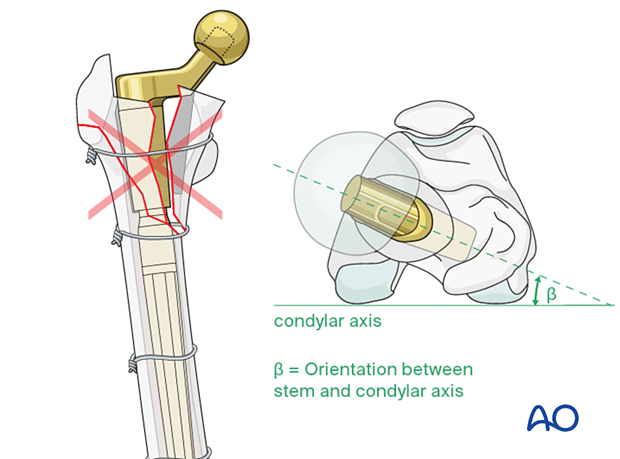
The surgeon must ensure anatomic limb alignment with regard to:
- adequate contact of the fracture fragments
- proper rotational alignment of the fracture fragments: the orientation of the distal femoral condylar axis should be aligned properly to the new femoral stem anteversion (recommended beta is equal to 5° to 15°)
- appropriate leg length
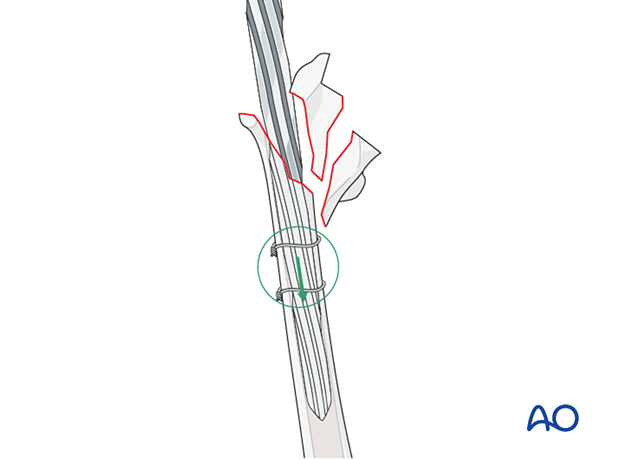
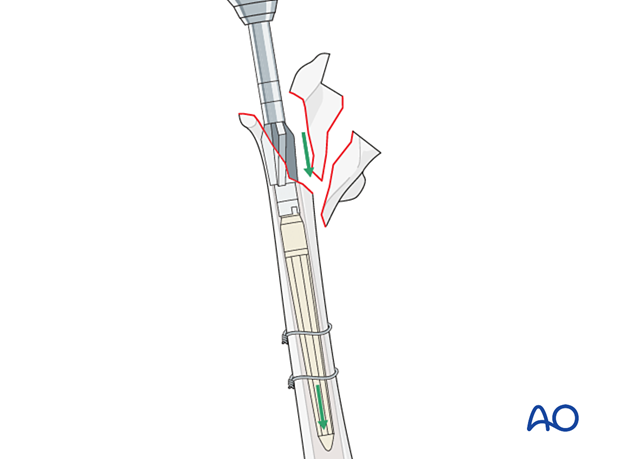
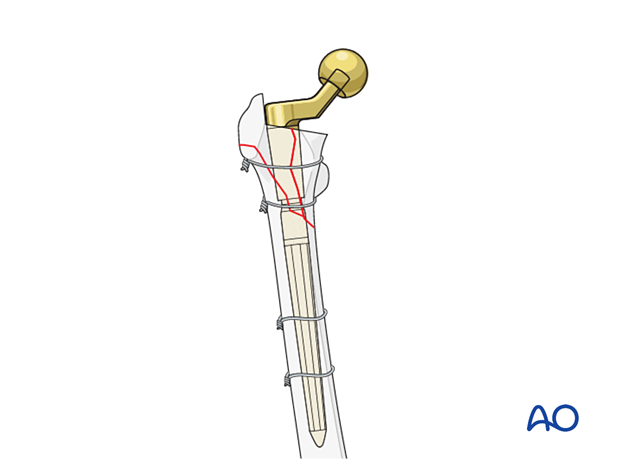
Additional extramedullary fixation
The surgeon must determine if additional extra-medullary adjunct fixation is required. If necessary, additional wires/cables can be used.
If the initial provisional fixation prior to femoral canal preparation was performed using a plate, additional screws/cables can be added.
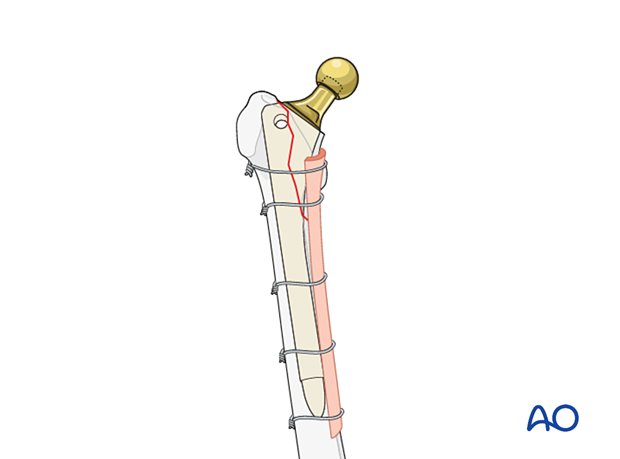
Adjunct strut graft
In selective cases of severe comminution, adjunct strut graft(s) may be considered to supplement the bone stock.
8. Aftercare following a femoral revision
Physiotherapy guidelines
Routine physiotherapy protocols for elective total hip arthroplasty is followed.
Early mobilization is recommended. Weight bearing status is individualized based upon fixation and implant stability.
Hip dislocation precautions are given to the patient.
Imaging
Postoperative radiographs can be made at 2 to 3 weeks to determine maintenance of satisfactory fracture reduction and fixation, no evidence of stem subsidence, or fracture displacement.
Follow-up radiographs can be made at 6 to 8 weeks after surgery to determine sufficient fracture fixation to increase the weight bearing status, and physical activities.
Future follow-up is similar to the routine and standard protocol for total hip arthroplasty.













