Trochanteric osteotomy
1. Preliminary remarks
Scar tissue due to previous exposure might obscure typical landmarks.
The trochanteric osteotomy is performed through a posterolateral approach which can be used for revision hip arthroplasty or ORIF of periprosthetic acetabulum and femur fractures. This can be extended into a formal Kocher-Langenbeck for treatment of periprosthetic acetabular fractures.
The femoral attachment of the short external rotators and hip capsule should be repaired to reduce the risk of postoperative dislocation (early descriptions of hip arthroplasty through a posterolateral approach suggested excision of the posterior hip capsule).
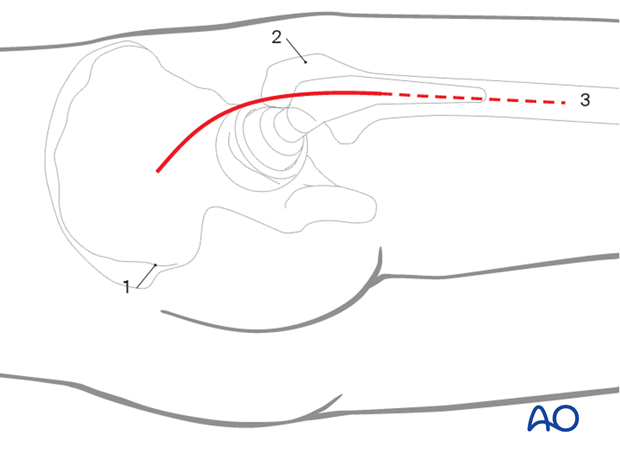
2. Skin incision
Outline all bony landmarks with a sterile marking pen:
- Posterior superior iliac spine (PSIS)
- Greater trochanter
- Shaft of femur
Start the skin incision posterior to the lateral side of the greater trochanter and carry it distally about 6 cm along the femoral axis. Proximally, the incision runs slightly curved towards the PSIS to a point approximately 6 cm proximal to the greater trochanter. This should be extended distally to incorporate the entire trochanteric osteotomy.
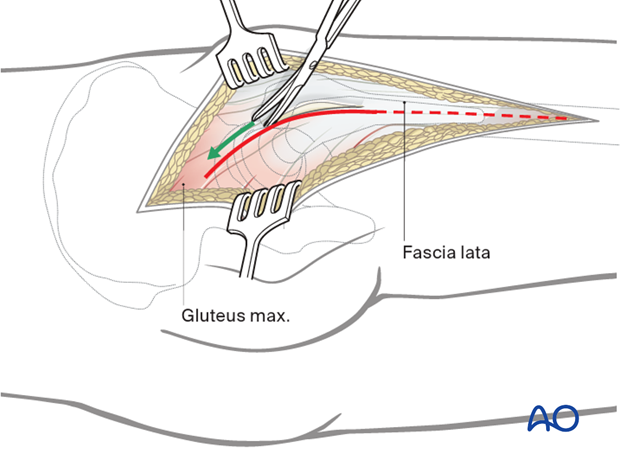
3. Dissection of fascia lata
Straight sharp dissection of the fascia lata and gluteal muscle across the greater trochanter. Incise the fascia lata in line with the skin incision. This can be extended as distally as necessary to incorporate the entire trochanteric osteotomy exposing the vastus lateralis.
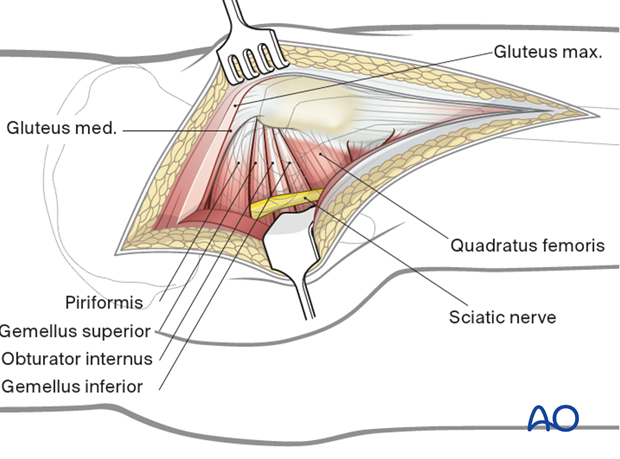
4. Protection of sciatic nerve
Retraction of the gluteal muscle flap posteriorly shows short external rotators inserting on femur (at least partially obscured by fat). The sciatic nerve can be palpated posteriorly in the depths of the wound. Its exposure is not necessary for uncomplicated hip arthroplasty, but the surgeon should be aware of the nerve’s location and avoid injuring it with retractors. The surgeon should consider exposing the sciatic nerve for more extensive surgical dissection.
5. Exposure of short rotator tendons
Bluntly dissect the tendinous insertions of the short external rotators.
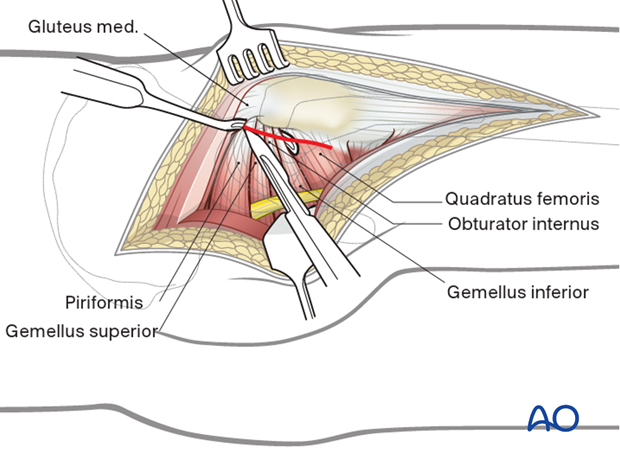
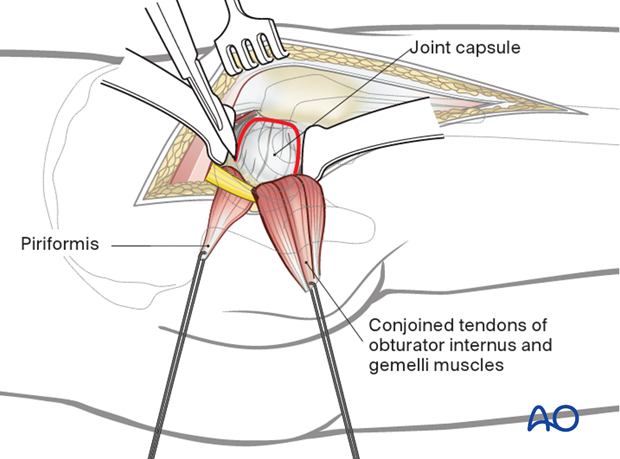
6. Exposure
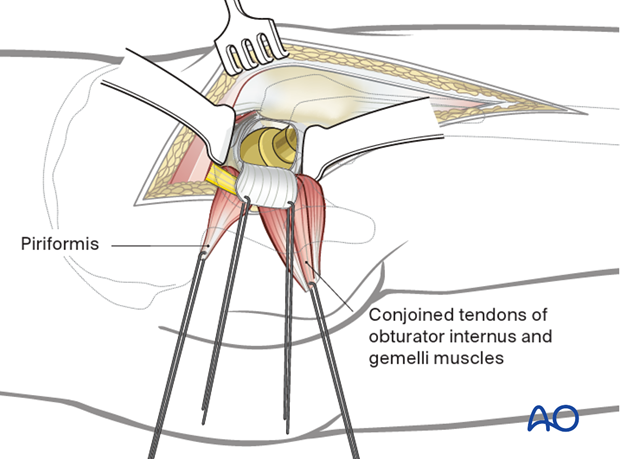
Before dividing the tendons, place heavy, nonabsorbable stay sutures for retraction and subsequent repair. One suture can be placed in the piriformis tendon, and the other in the conjoined tendons of obturator internus and gemelli. Reflection of the short rotator muscles exposes the hip capsule. Next, enter the joint with a broad-based, 3-sided capsulotomy as shown.
Expose the hip joint by creating and reflecting a full thickness, broad-based flap through the posterior hip capsule. Heavy (e.g. #2) non-absorbable sutures can be used to tag the capsule to aid in retraction and subsequent repair. Once this dissection is complete, attention can be turned to perform the trochanteric osteotomy.
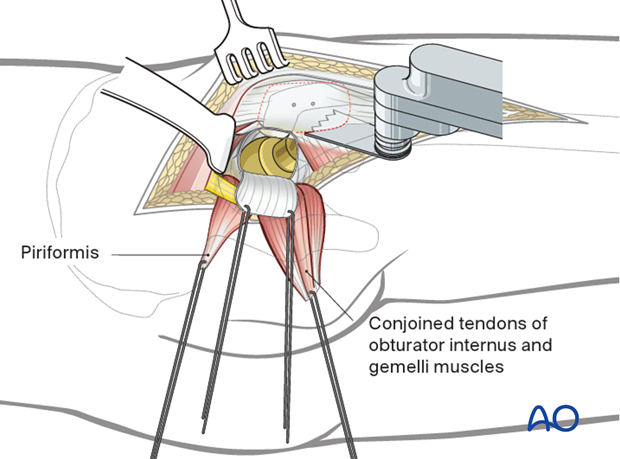
7. Trochanter osteotomy
The plane of the trochanter osteotomy is then prepared by cauterizing the trochanteric anastomotic vessels.
The osteotomy is then carried out from the tip of the trochanter to the base of the vastus tubercle using a saline-cooled oscillating saw or osteotome. A small portion of the medius tendon is left temporarily attached to the intact femur until the trochanter can be mobilized.
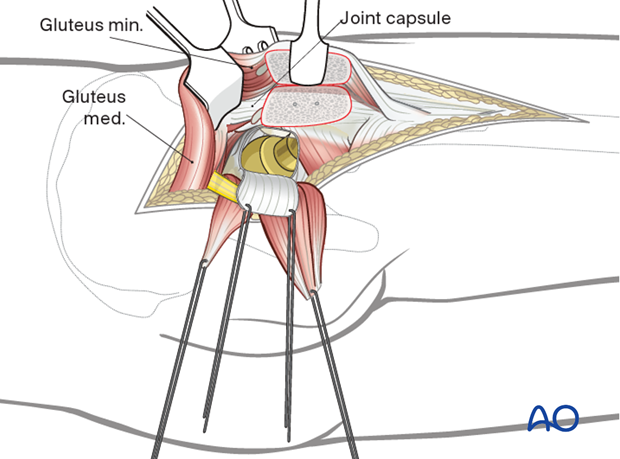
8. Anterior exposure and mobilization of gluteus minimus
The vastus lateralis fascia is incised from the vastus tubercle distally a distance of 5-8 cm to allow extra periosteal mobilization of the proximal lateralis muscle belly with the trochanteric segment.
The trochanter is progressively everted utilizing a Hohmann retractor placed over the anterior aspect of the greater trochanter. Now, the small remaining gluteus medius attachment to the intact trochanteric ridge is released. Scar tissue should be released to allow mobilization of the trochanteric osteotomy. At times, the piriformis insertion may be partially attached to the mobile trochanteric fragment. This should be released as the trochanter is everted.
Flex and externally rotate the hip to improve anterior exposure.
This allows complete mobilization of the gluteus minimus from the retroacetabular surface along the superior capsule to its femoral insertion along the anterior aspect of the trochanter.
The minimus insertion may also straddle the trochanter osteotomy. If so, it must be released from the intact femur to allow full trochanteric mobilization.
9. Wound closure
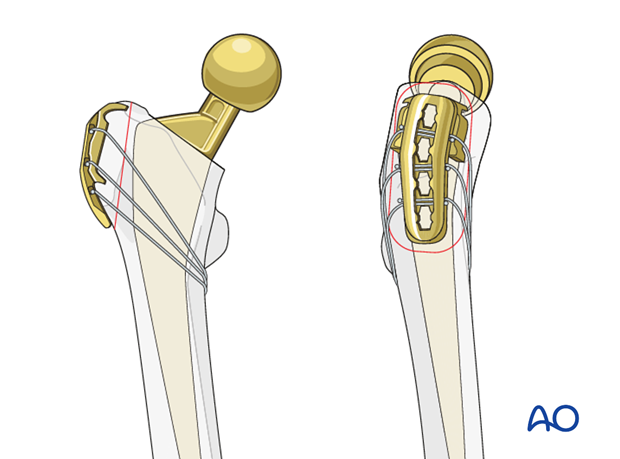
When the reconstruction is completed, the great trochanter is reattached using cerclage wires through drill holes or plate and screw fixation (trochanteric claw or hook plate).
Standard closure of the posterior approach should be performed.
Considerations for periprosthetic fracture patients
A layered closure is preferred for periprosthetic fractures. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied, and negative pressure incisional wound care can be considered.














