Posterolateral approach
1. Preliminary remarks
Scar tissue due to previous exposure might obscure typical landmarks.
The posterolateral approach can be used for revision hip arthroplasty or ORIF of periprosthetic femur fractures. This can be extended into a formal Kocher-Langenbeck for treatment of periprosthetic acetabular fractures.
The approach is essentially the same as the Kocher-Langenbeck, but exposure is limited to the hip joint, respecting but not displaying the sciatic nerve. The femoral attachment of the short external rotators and hip capsule should be repaired to reduce the risk of postoperative dislocation (early descriptions of hip arthroplasty through a posterolateral approach suggested excision of the posterior hip capsule).
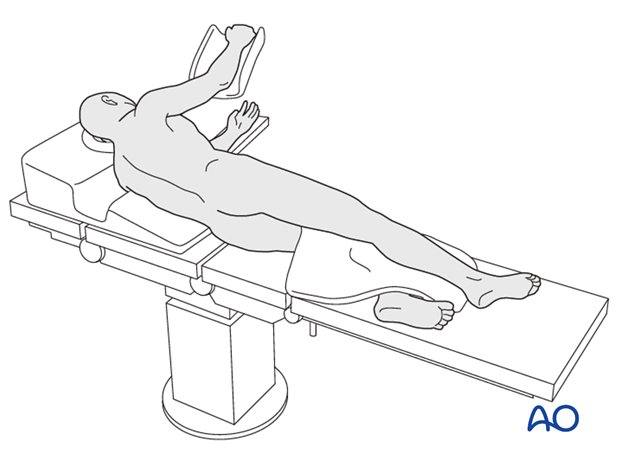
2. Positioning
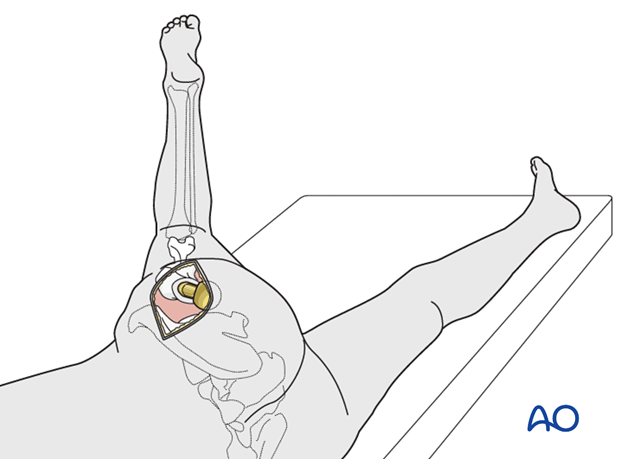
The posterolateral approach to the hip may be done with the patient in lateral decubitus or prone positions. For arthroplasty, a lateral decubitus position is usually chosen.
The patient is placed in the lateral decubitus position, with supports to prevent rotation away from true lateral, and appropriate padding to limit focal pressure.
After sterile preparation of the hip region, the involved leg is draped free, to permit full mobility.
The patient can also be positioned prone, if necessary (the lateral position is preferred for periprosthetic fracture and revision arthroplasty).
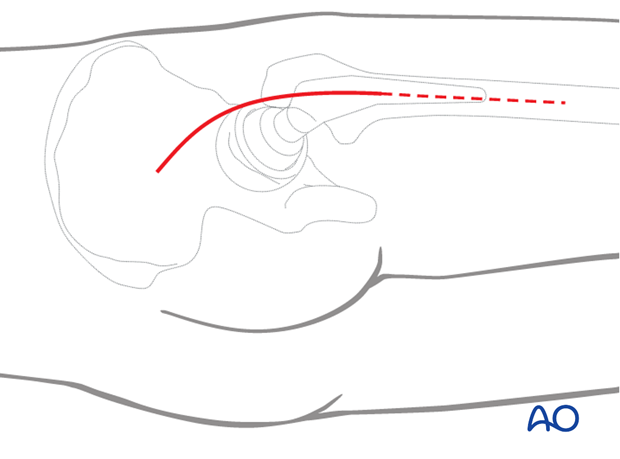
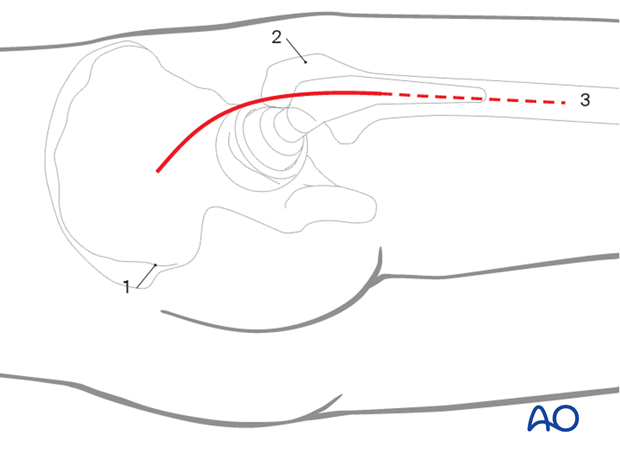
3. Skin incision
Outline all bony landmarks with a sterile marking pen:
- Posterior superior iliac spine (PSIS)
- Greater trochanter
- Shaft of femur
Start the skin incision posterior to the lateral side of the greater trochanter and carry it distally about 6 cm along the femoral axis. Proximally, the incision runs slightly curved towards the PSIS to a point approximately 6 cm proximal to the greater trochanter. This can be extended as distally as necessary.
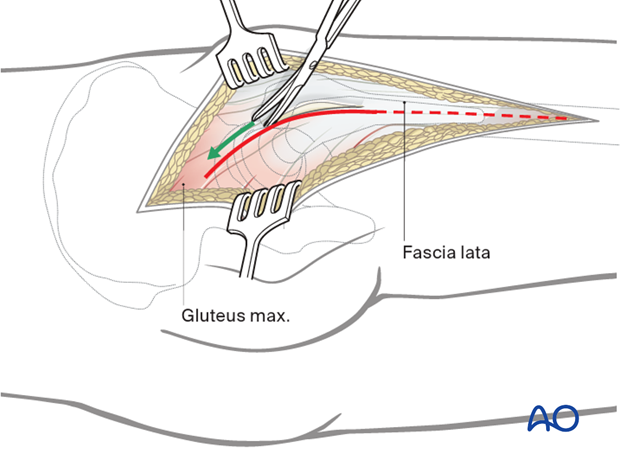
4. Dissection of fascia lata
Straight sharp dissection of the fascia lata and gluteal muscle across the greater trochanter. Incise the fascia lata in line with the skin incision. This can be extended as distally as necessary exposing the vastus lateralis for a subvastus approach.
5. Protection of sciatic nerve
Retraction of the gluteal muscle flap posteriorly shows short external rotators inserting on femur (at least partially obscured by fat). The sciatic nerve can be palpated posteriorly in the depths of the wound. Its exposure is not necessary for uncomplicated hip arthroplasty, but the surgeon should be aware of the nerve’s location and avoid injuring it with retractors. The surgeon should consider exposing the sciatic nerve for more extensive surgical dissection.
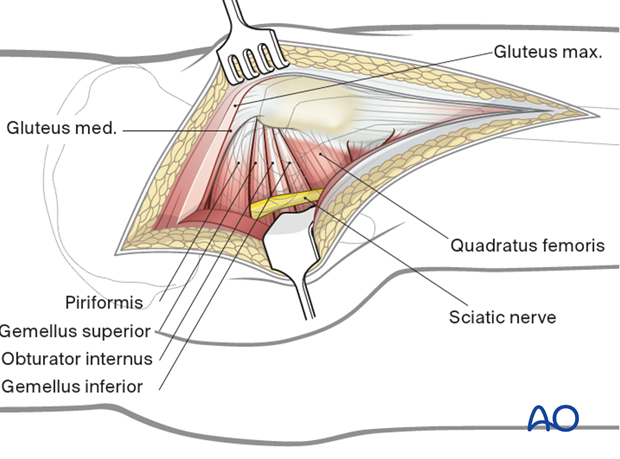
6. Exposure of short rotator tendons
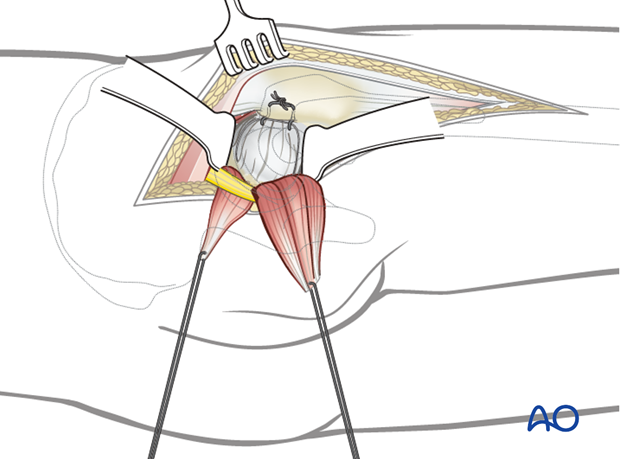
Bluntly dissect the tendinous insertions of the short external rotators.
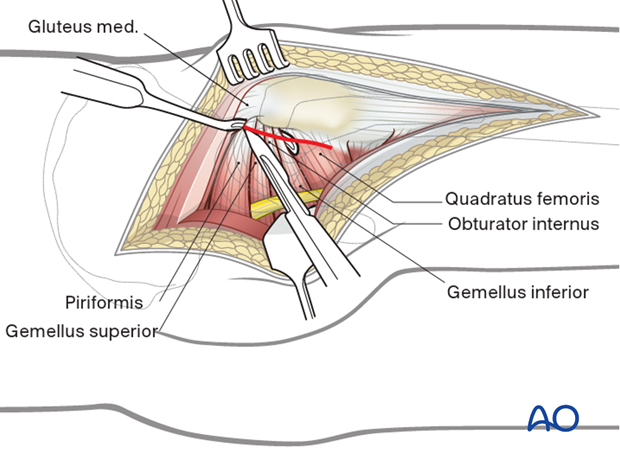
7. Exposure
Before dividing the tendons, place heavy, nonabsorbable stay sutures for retraction and subsequent repair. One suture can be placed in the piriformis tendon, and the other in the conjoined tendons of obturator internus and gemelli. Reflection of the short rotator muscles exposes the hip capsule. Next, enter the joint with a broad-based, 3-sided capsulotomy as shown.
Alternatively, the short external rotators and the capsule can be taken down together.
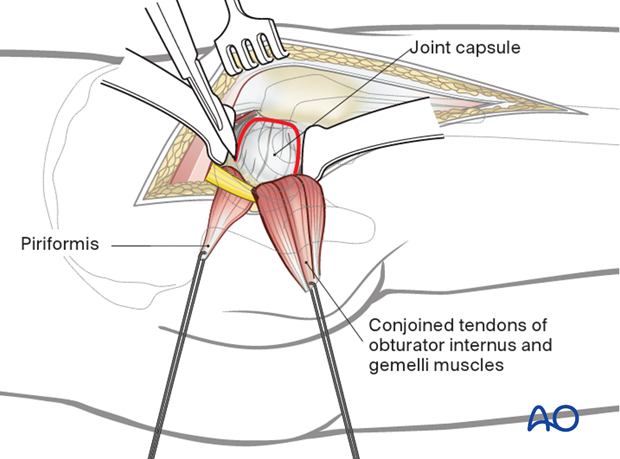
Expose the hip joint by creating and reflecting a full thickness, broad-based flap through the posterior hip capsule. Heavy (e.g. #2) non-absorbable sutures can be used to tag the capsule to aid in retraction and subsequent repair.
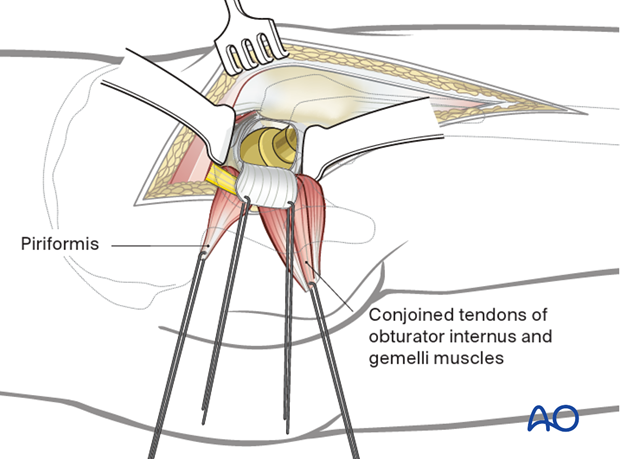
If needed, the hip is dislocated with internal rotation.
8. Closure
At the completion of the procedure, the posterior capsular flap sutures, and then the tendon sutures, are tied to each other after being passed through drill holes in the posterior greater trochanter. Quadratus femoris, if divided, is repaired separately. A secure repair of the tendons and capsule decreases the risk of hip prosthesis dislocation after a posterior approach.
(See also:Pellicci PM et al.(2009) MRI shows biologic restoration of posterior soft tissue repairs after THA Clin Orthop Relat Res.April; 467(4): 940–945.)
Considerations for periprosthetic fracture patients
A layered closure is preferred for periprosthetic fractures. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied, and negative pressure incisional wound care can be considered.














