Anterolateral approach
1. Preliminary remarks
Scar tissue due to previous exposure might obscure typical landmarks.
The anterolateral approach (Watson-Jones) to the proximal femur, through the interval between glutei and tensor fasciae latae provides somewhat limited access to the hip joint along with the lateral proximal femur. With well-positioned retractors and adequate soft-tissue releases, it is possible to perform open reduction of proximal periprosthetic femoral fractures or revision arthroplasty.
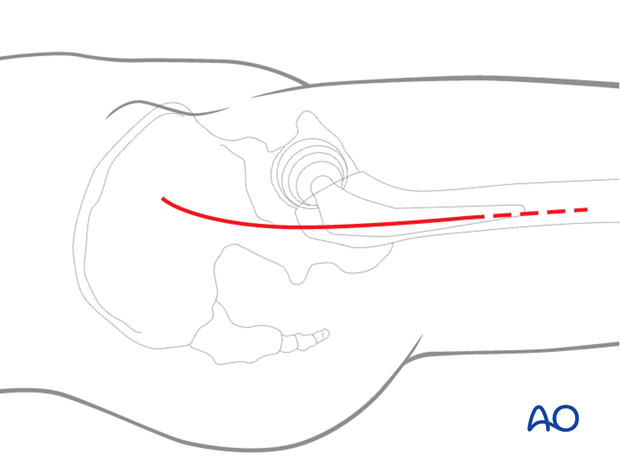
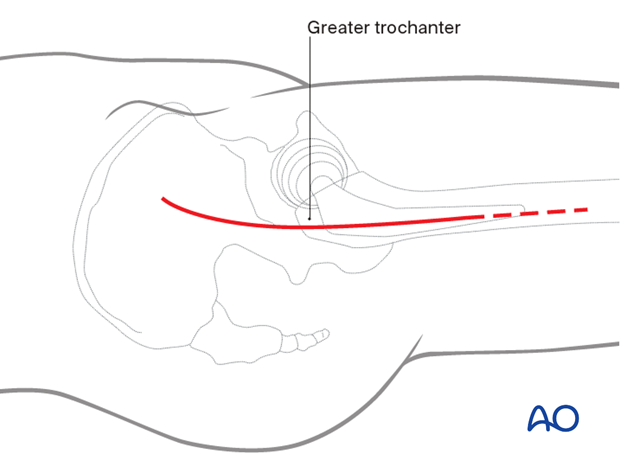
2. Skin incision
Start the slightly anteriorly curved skin incision about 7-10 cm proximal of the lateral part of the greater trochanter (directed towards the tubercle of the iliac crest – the posterior landmark of tensor fasciae latae origin). Distally, the incision extends along the femur about 10 cm below the greater trochanter. The approach can be extended distally, for adequate exposure of the fracture.
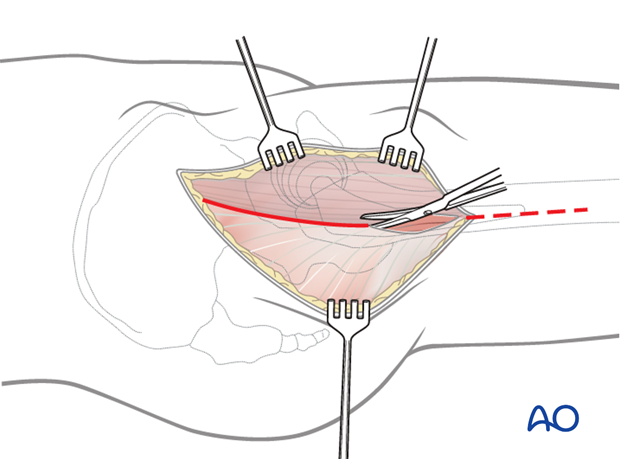
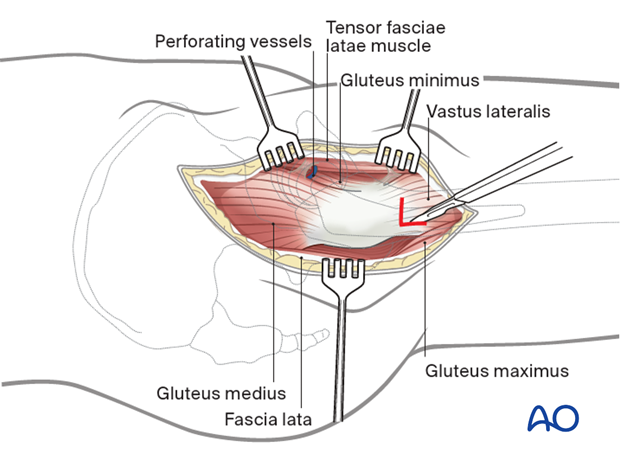
3. Incision of fascia lata
Expose the fascia lata sharply. Incise the fascia lata over the femur and extend this incision proximally along the posterior border of the tensor fascia lata.
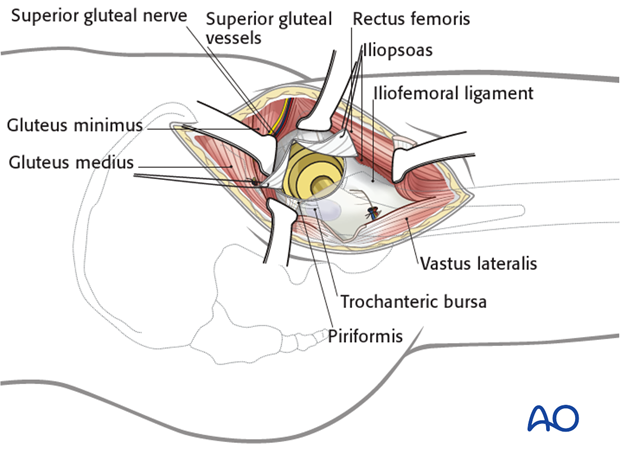
4. Deep surgical dissection
With the greater trochanter and the gluteus medius muscle exposed, retract the tensor fascia lata anteriorly and the gluteus medius muscle posteriorly. Expose the interval between the gluteus medius and the tensor fascia lata and extend it proximally over the hip joint. This can be best done by blunt dissection.
Be aware of vessels running across this interval. They require ligation or cautery.
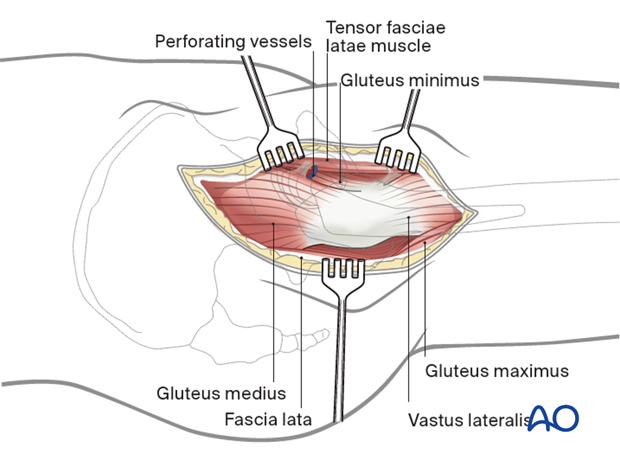
For further exposure of the femur and placement of hardware, the vastus lateralis can be released and repaired later.
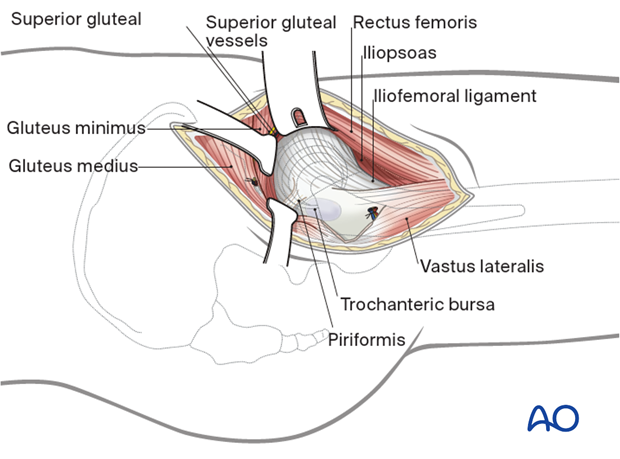
Anterior release of vastus lateralis
The origin of the vastus lateralis muscle should be released from the anterior inferior trochanteric region to expose the underlying hip capsule. Retract the muscle inferiorly.
Adjust the retractors as necessary and debride periarticular fat to expose the hip capsule.
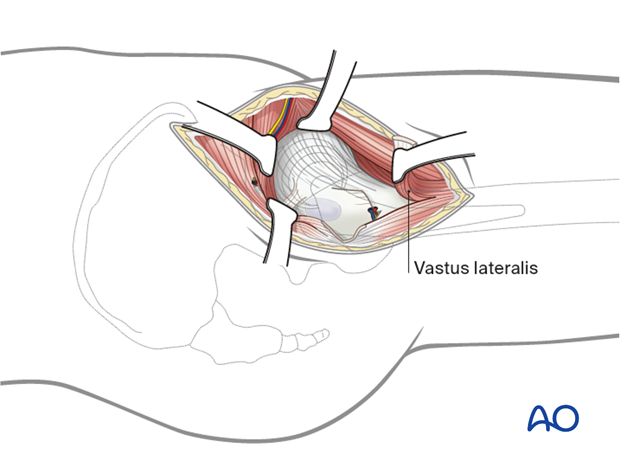
Exposure of hip capsule
Place a Hohmann retractor into the bone proximal to the hip capsule. Additional retractors anteriorly and posteriorly will open the dissected interval.
External rotation of the leg improves access to the hip capsule.
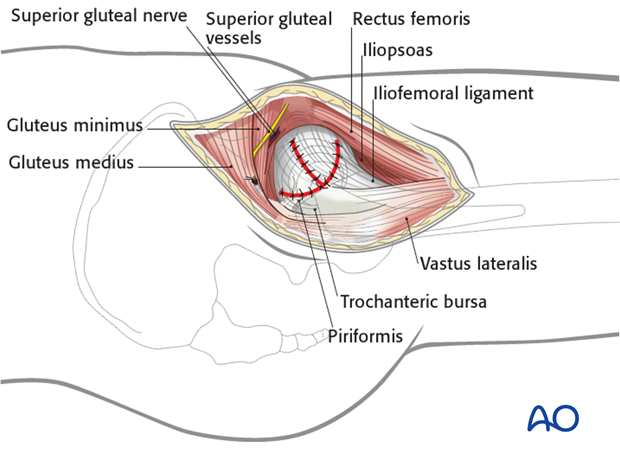
5. Opening of the joint capsule
Make a T-shaped incision in the capsule, if necessary, for exposure…
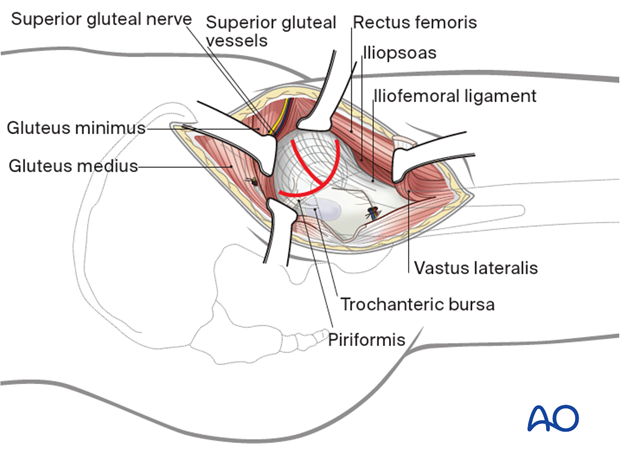
…and place two retraction sutures, anteriorly and posteriorly. This capsulotomy shows the prosthesis. Lateral traction and repositioning of the leg can improve visualization. The prosthesis can be dislocated anteriorly.
The incision can be prolonged distally over the proximal vastus lateralis to allow for insertion of plate fixation.
6. Wound closure
Perform a meticulous debridement of all soft tissues before starting wound closure.
Remove necrotic tissue and irrigate the entire wound to decrease the risk of periarticular ossification. Insert suction drains if desired.
After capsular closure, repair the vastus lateralis to its origin.
Close the fascia lata incision with interrupted sutures. Close the subcutaneous tissue and skin as desired.
Considerations for periprosthetic fracture patients
A layered closure is preferred for periprosthetic fractures. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied, and negative pressure incisional wound care can be considered.














