ORIF (plate and screw) of anterior fractures with or without cup revision
1. Principles
Successful treatment of acetabular fractures noted intraoperatively is critical to achieve component ingrowth, pain control and long-term survivorship of the arthroplasty.
For further information about standard techniques for ORIF in native acetabular fractures, please refer to the acetabulum section of the AOSR.
2. Approach and extensions for fracture visualization
The primary surgical approach may predict the fracture location:
- Direct anterior and anterolateral approaches are more commonly associated with anteriorly based fractures.
- Direct lateral and posterior approaches to the hip are more commonly associated with posterior type fractures.
- Medial wall fractures can be associated with any approach
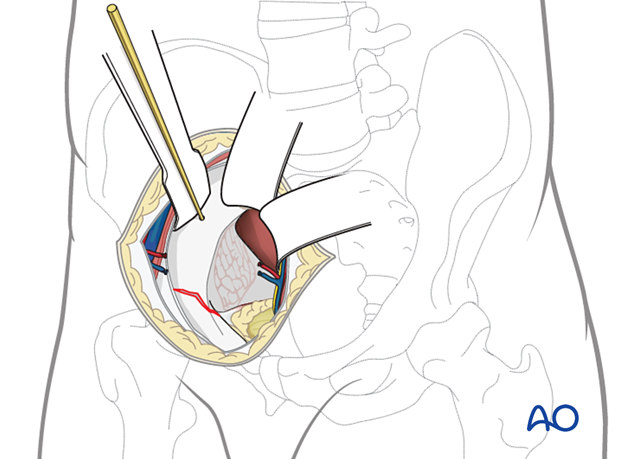
In the setting of an anterior acetabular fracture, and the cup is unstable, the standard surgical approach should be enlarged to evaluate the anterior column and the anterior wall.
The patient can be in a lateral or supine position.
If extending the surgical approach does not allow adequate fracture evaluation, removal of the cup and direct visualization of the acetabulum is beneficial.
Anterior wall fractures
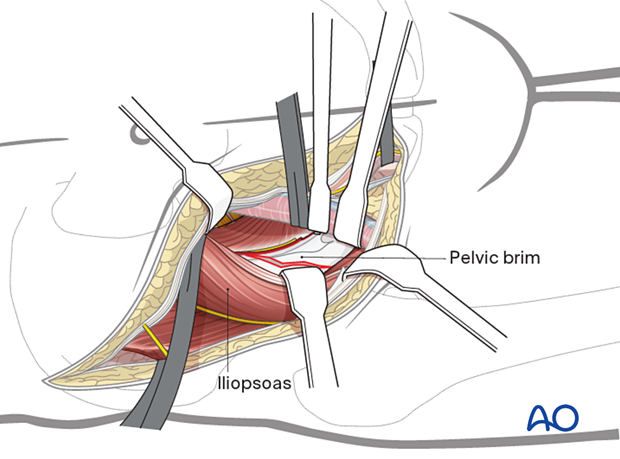
A fracture of the anterior wall must be evaluated for extension to the pelvic rim. When this extension exists, often a separate surgical approach may be required. An anterior intrapelvic approach, iliofemoral or ilioinguinal approach can be used.
Anterior column fractures
High anterior column fractures may be best treated utilizing the lateral window of the ilioinguinal approach.
3. Cup removal
In the setting of infection, loosening, or osteolysis, cup removal may lead to acute bone loss and/or the creation of periprosthetic fractures. If this destabilizes the acetabular support of the arthroplasty, fracture specific reduction and fixation techniques are necessary. Depending on the fracture pattern, ORIF with plate and screw and/or column fixation may be indicated.
It is critical to remove the cup without causing additional fractures or bone defects.
Liner removal
The cup liner is removed prior to cup removal.
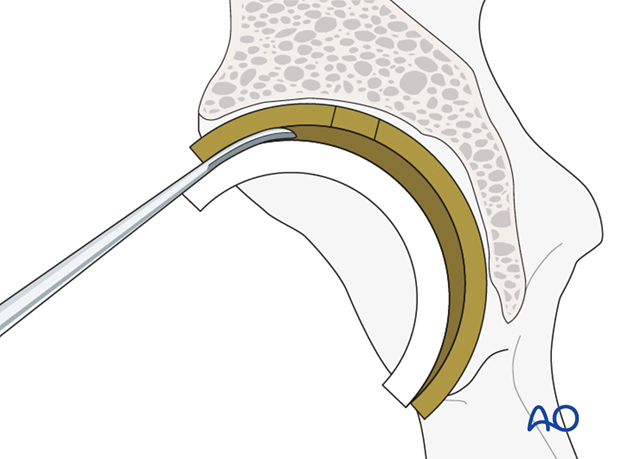
Cup screw removal
Ensure that all the cup screws are removed prior to attempting to remove the cup itself.

Acetabular component removal
The acetabular component is removed. Details on how to remove an acetabular cup are described in the basic technique for acetabular cup removal.
4. Reduction and stabilization of anterior moiety fractures
Fracture reduction
In these fractures, anatomic reduction of the articular surface is not relevant. Columnar stability and wall containment are needed.
In the setting of an unstable cup, the anterior aspects of the joint should be reduced and buttressed.
Anterior wall fracture stabilization
Fracture of the anterior aspect of the acetabulum are typically less contributory to cup instability than posterior fractures.
Although small plates may be utilized to buttress very marginal fractures, the stabilization of such small fractures may not be beneficial given the relative thickness of the anterior wall.
Anterior wall fractures can be buttressed utilizing a brim plate that spans the displaced portions of the anterior wall and links them to the posterior column.
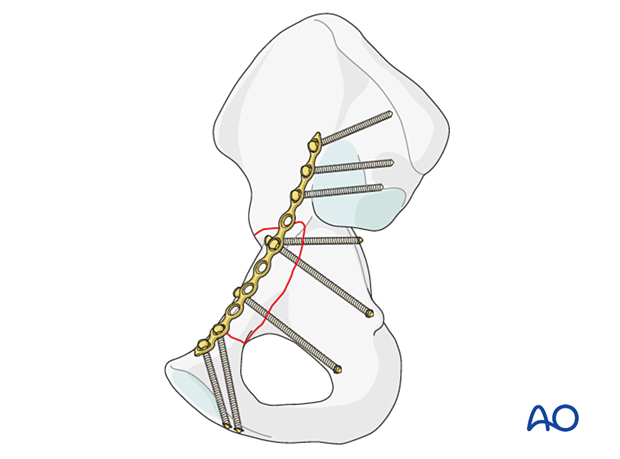
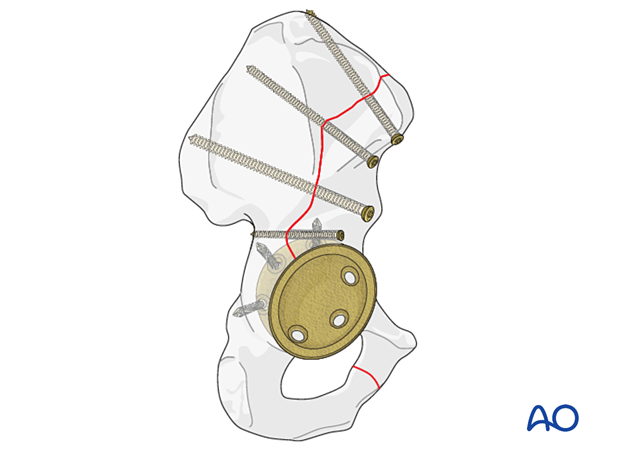
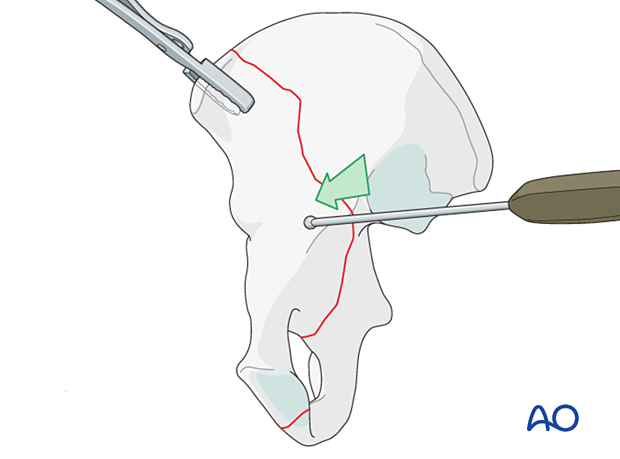
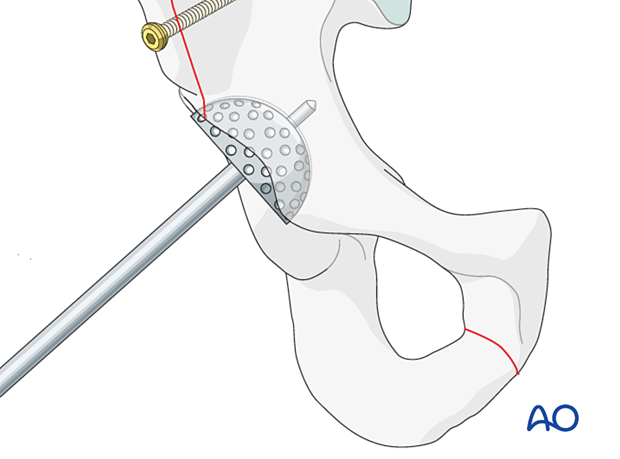
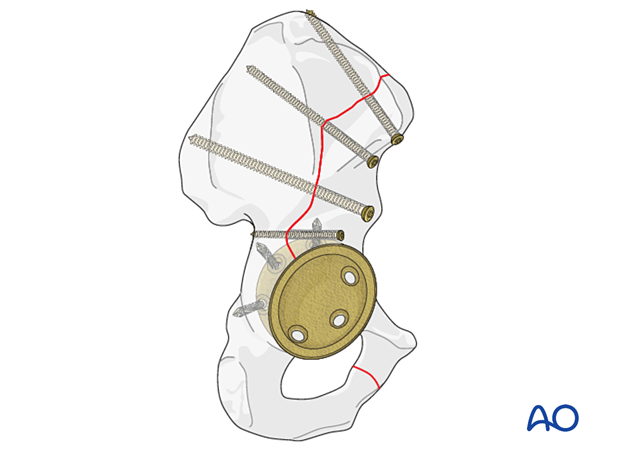
Anterior column fracture stabilization
Anterior column fractures typically have displacement from the acetabulum out through the interspinous notch, between the ASIS and the medius tubercle, or posterior to the tubercle.
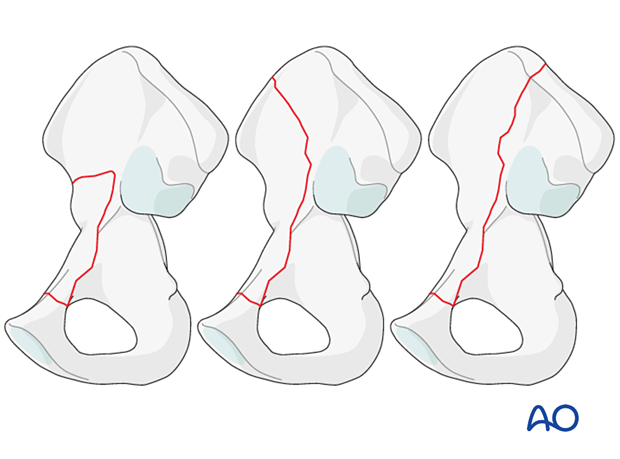
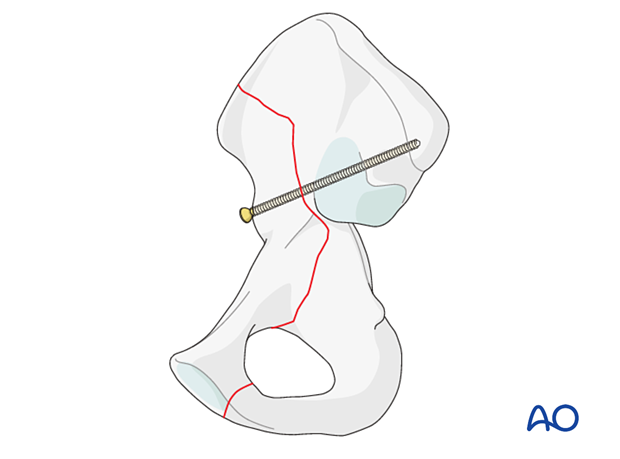
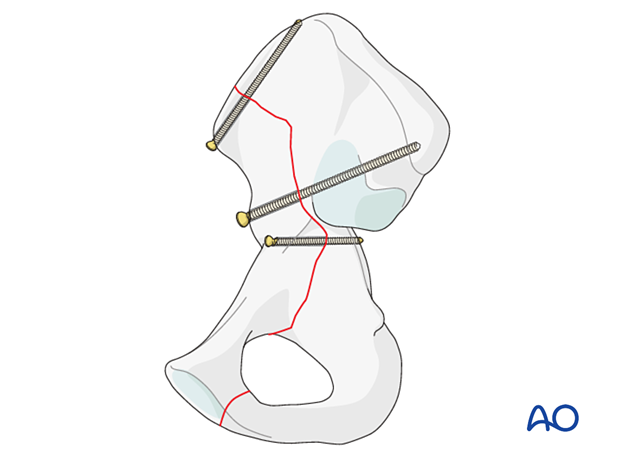
After reduction typically an intramedullary screw is inserted from the AIIS down the sciatic buttress towards the PSIS.
Additional screws stabilization can be achieved with screws inserted at the iliac crest and posterior column.
If deemed necessary, further stabilization can be performed per surgeons preference.
Radiographic confirmation
Reduction and stabilization of the fracture should be confirmed using fluoroscopy.
5. New acetabular cup insertion
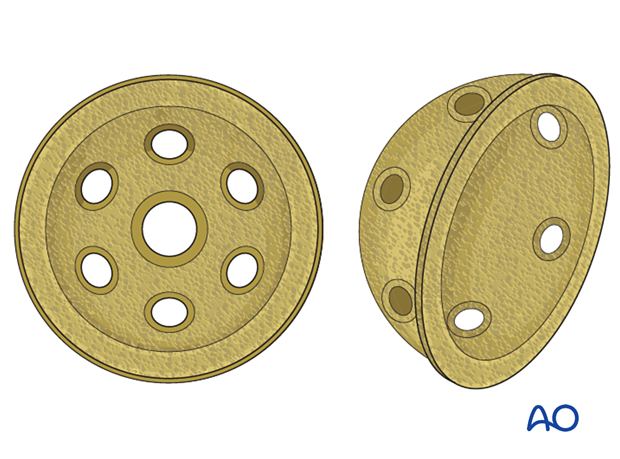
With the anatomy of the acetabulum restored, a standard multi-hole cup can be utilized.
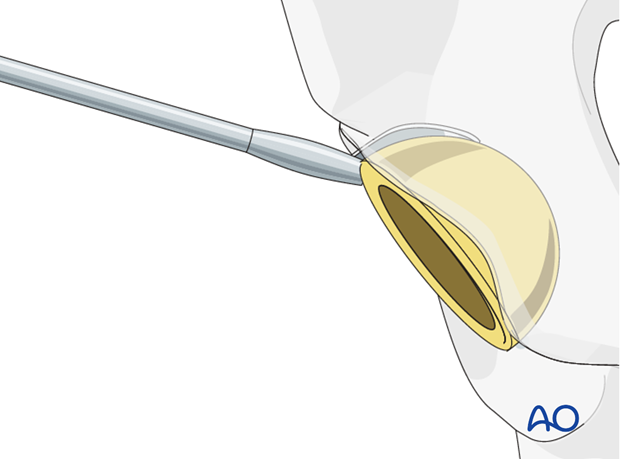
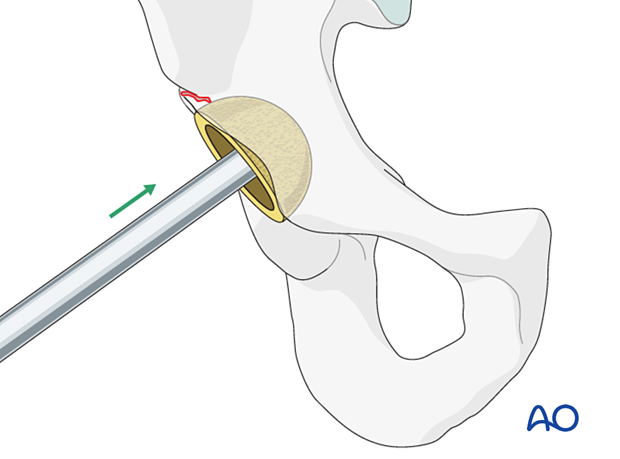
Acetabular reaming
The acetabulum should be reamed gently as not to compromise the reduction. The new cup can be implanted.
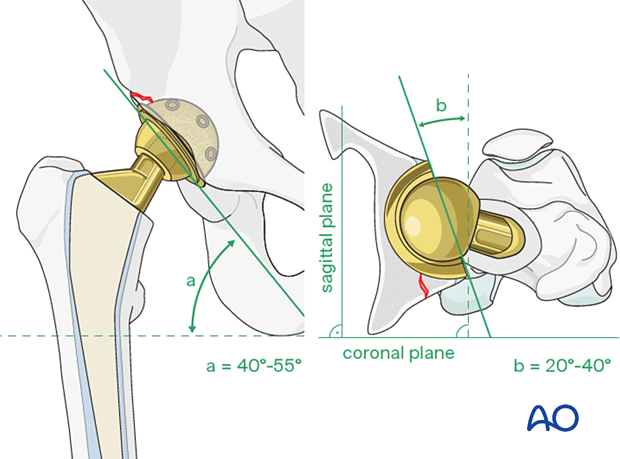
New cup positioning
The surgeon should insert the new cup following the recommended position (inclination) and orientation (anteversion) guidelines.
The accepted "safe zone" is:
- cup inclination 40° to 55° (a)
- cup anteversion 20° to 40° (b)
New cup impaction
The appropriate cup is inserted using implant system specific instruments.
Cup screw fixation
The cup should achieve rim fit. Insert multiple screws in different planes to achieve stabilization to allow bony ingrowth.
Residual bony defects should undergo bone grafting with autograft or allograft, per surgeon's preference.
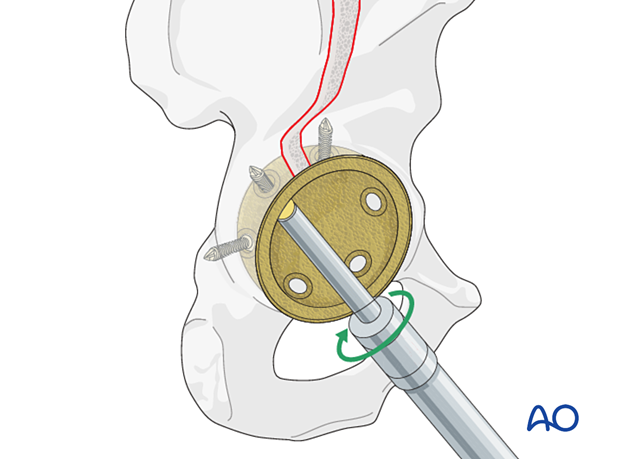
For further details about the multihole pressfit cup implantation please refer to the treatment: Revision of cup to multihole pressfit cup.
6. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
Patient mobilization
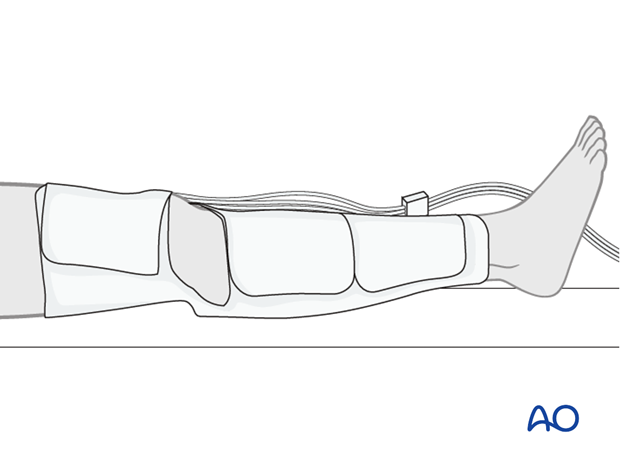
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
Precautions against hip dislocation
Hip precautions can be extremely important in patients who have suffered intraoperative acetabular fracture. Much work has been done to minimize the surgical exposure during hip arthroplasty to decrease the risk of dislocation. These advantages are typically removed when acetabular stabilization need to be performed. A dislocation in the postoperative course of such a patient can be disastrous.
Patients are instructed to follow standard hip precautions against dislocation based upon the surgical approaches for hip arthroplasty.
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.