Hook plate and screw fixation
1. Principles
A proximal third diaphyseal fracture can present a particularly difficult problem for decision making. If there is clear evidence of the stability of the prosthesis, then removal can be more injurious to the patient than stabilization. However, standard periprosthetic plates may not adequately support a proximal femoral segment. In this setting, a proximal femoral locking hook plate may be selected for stabilization.
2. Approach
Direct lateral approach extension
Direct lateral approach to the femoral diaphysis is typically utilized. This will require an extension to the proximal femur.
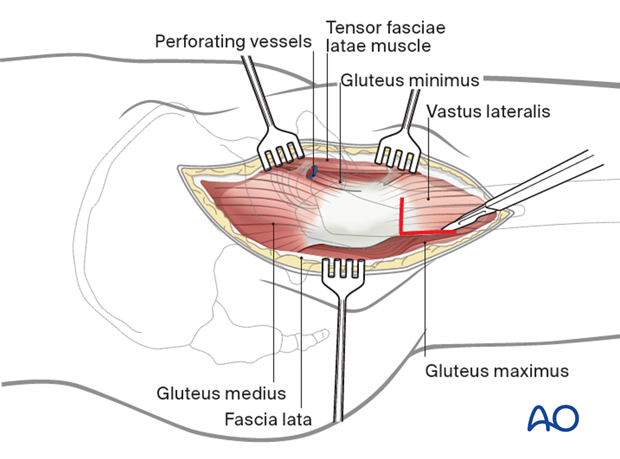
Option: Vastus lateralis origin release or split
To apply a plate to the lateral aspect of the femur, the vastus lateralis origin can be released and this can be repaired after stabilization is obtained.
Alternatively, if the patient has a very large proximal femoral anatomy, the vastus lateralis origin may be split in its mid portion and the plate slipped below the muscle belly. This avoids the morbidity of a more complex tenotomy.
Other approaches
Other approaches that can be used to perform this procedure are:
- Anterolateral approach
- Direct anterior approach
- Iliofemoral (Smith-Petersen) approach
- Posterolateral approach
- Trochanteric osteotomy
- Extended trochanteric osteotomy
These approaches can be performed with the patient in a lateral or supine position.
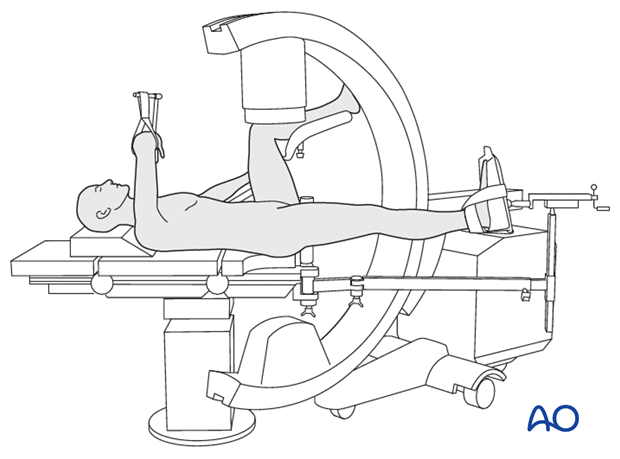
Option: use of a radiolucent or fracture specific table
A radiolucent table or a fracture specific table may be used.
The choice depends on surgeon experience and preference. The control of the fracture may often be more difficult on a traction table.
3. Reduction
Reduction technique when utilizing a hook plate depend on fracture morphology. In the setting of transverse, spiral and oblique fracture patterns without comminution, direct reduction techniques should be carried out.
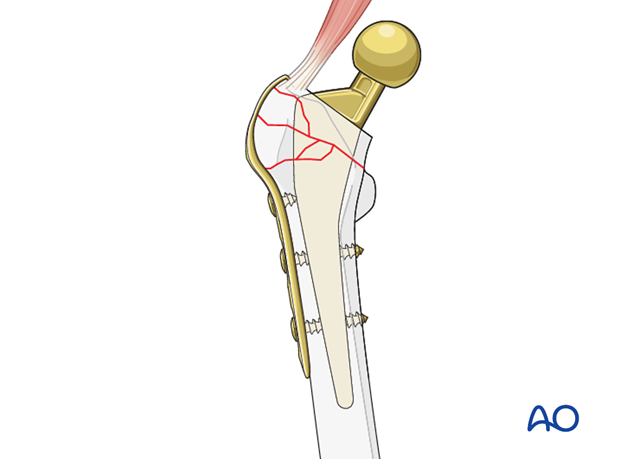
In the instance of comminuted fractures, indirect reduction technique should be carried out.
These techniques are described in the compression and bridging sections of this module.
4. Implant considerations
In a setting of a proximal third fracture, fixation can be difficult.
Once the reduction is achieved, cerclage should be used, when possible, to create compression.
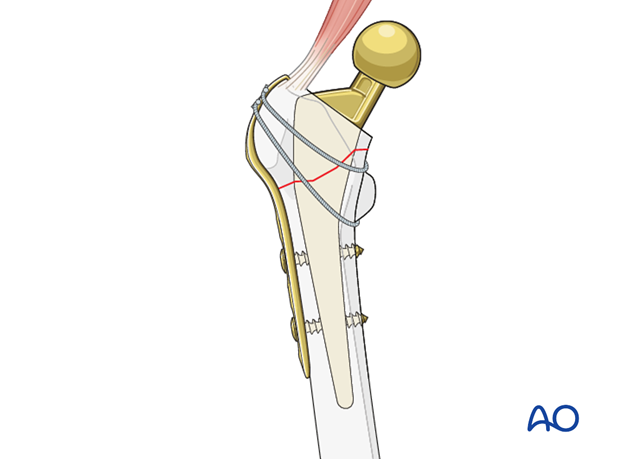
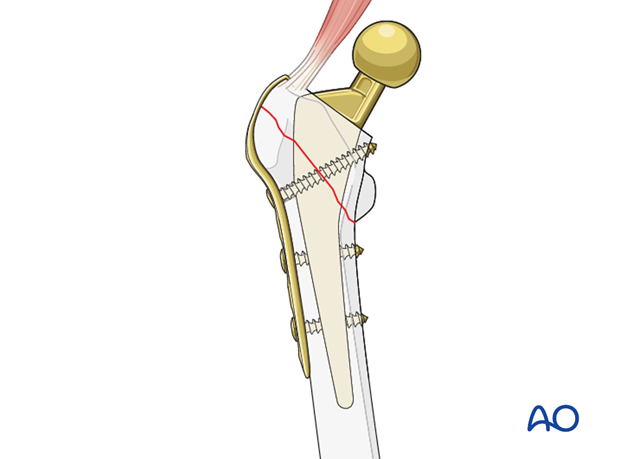
If the fracture is not amendable to cerclage, sometimes small screw lag fixation utilizing fully threaded screws around the femoral stem.
If neither of these is possible, or if the fracture is comminuted, stability can be obtained through use of a hook plate only.
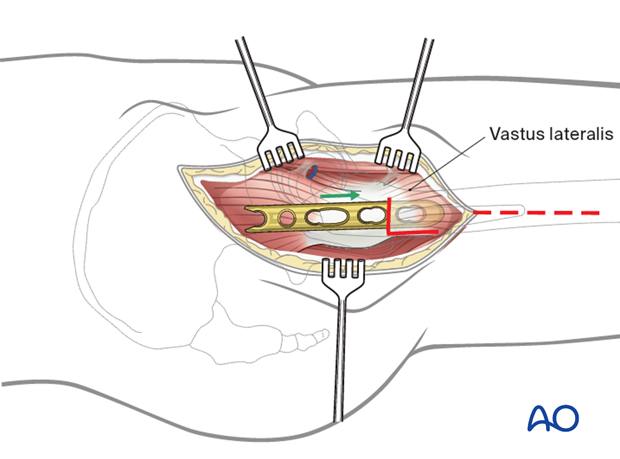
5. Plate application
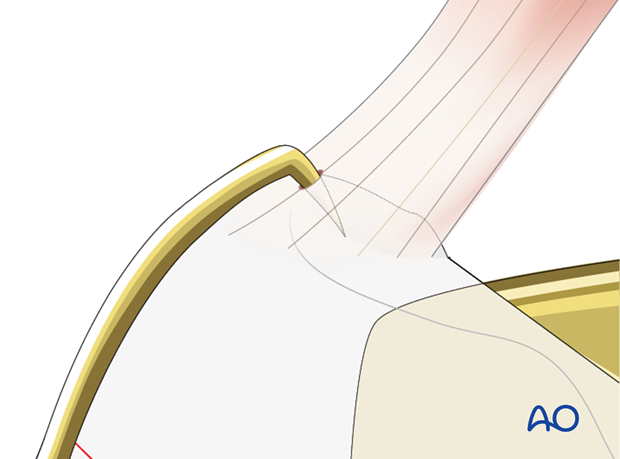
The plate can be applied on the lateral side of the femur to the proximal segment through the abductor tendon.
Placement of these plates can be challenging, as the sagittal bow rarely matches the bow of the patient's proximal femur. Care must be taken to achieve plate position and avoid fracture displacement.
Distal stabilization is carried out either in neutralization or compression mode, depending on the morphology of the fracture.
If there is no room for bicortical screw fixation, different options may be used around the femoral stem:
- Unicortical locking screw fixation
- Cerclage cables integrated into the plate
- Locking attachment plate
For additional details on these implants please refer to adjunct plate options.
Additional details about plate stabilization, depending on fracture configuration, can be found in the proximal femoral shaft section of the AO Surgery Reference.
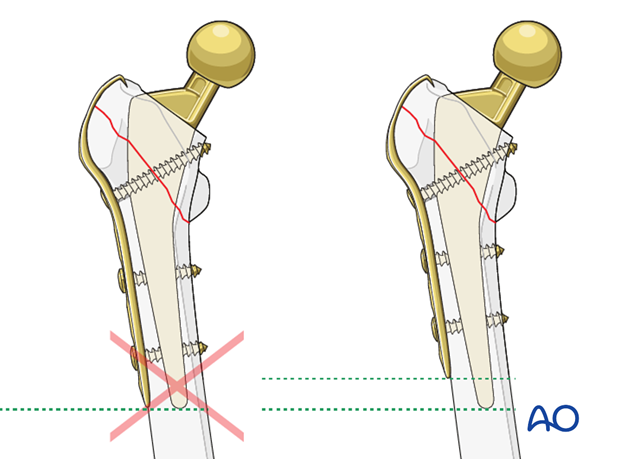
It is not advised to end the plate at the same level as the tip of the femoral stem.
6. Closure
A layered closure is preferred for periprosthetic fractures. If the vastus lateralis has been released, it should be primarily repaired with a nonabsorbable braided stitch. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied and negative pressure incisional wound care can be considered.

7. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
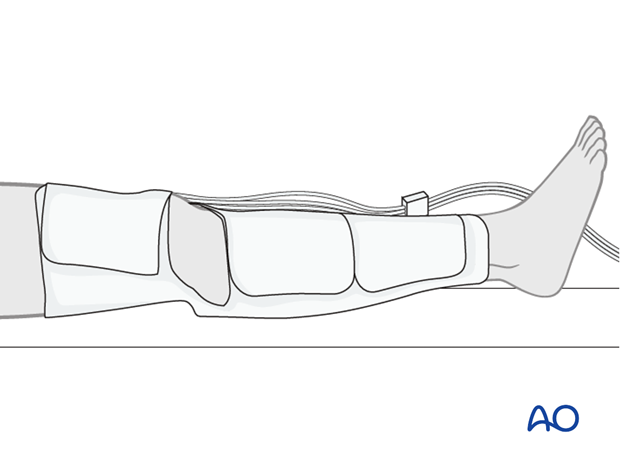
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.