ORIF - Plates without angular stability
1. Principle
Anatomical reduction
Split depression fractures are intraarticular, therefore they need anatomical reduction.
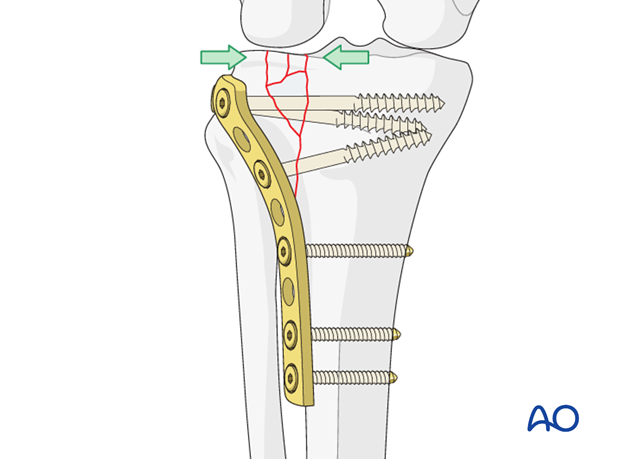
Buttress plate
The plate in this procedure acts as a buttress to neutralize the axial forces on the tibial plateau.
Lateral versus medial condylar fractures
The operative procedures for lateral condylar fractures and medial condylar fractures are comparable, but the medial fractures tend to be more difficult.
In medial condylar fractures, the position of the plate is determined by the principle fracture line. Therefore, the plate may be anteromedial, posteromedial or posterior.
The split depression fracture involving the tibial spines and one of the tibial plateaus is a special subtype. It is usually sustained as a result of a high velocity axial compression which is directed posteromedially. The result is a posteromedial fracture dislocation of the knee. The difficulties in dealing with this fracture arise in restoring the medial tibial condyle which is frequently split in the coronal plane as well, with the impaction and fragmentation of the medial portion of the lateral plateau and the intercondylar eminence, and fragments of bone caught in the major fracture line.
A lateral condylar fracture treatment is shown here.
2. Patient preparation
Depending on the approach, the patient may be placed in the following positions:
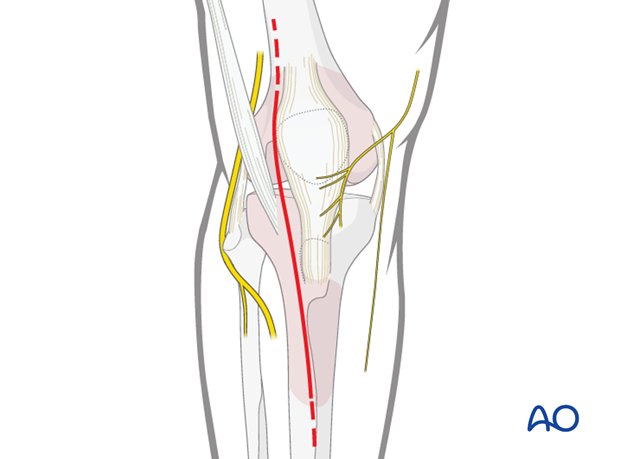
3. Approach
For the fracture illustrated an anterolateral approach is used.
Different fracture configurations may demand a medial/posteromedial or posterior approach.
4. Reduction
Window in the metaphyseal area
Approach from below through the fracture. The reduction of the articular surface is checked directly through a standard submeniscal articular exposure. Reduction of the articular surface is accomplished by elevating the fragments from below.

K-wire insertion
Temporary fixation with K-wires may be helpful.
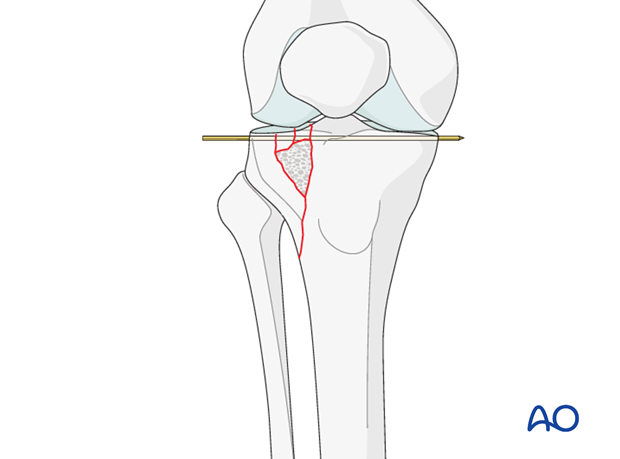
Filling of defect
The metaphyseal defect, which results when the articular fragments are reduced, may be filled with cancellous autograft or a corticocancellous block to support the elevated fragments. Alternatively, bone substitutes may be used.
5. Fixation
Preliminary fixation
Once reduction of the articular fragments is achieved and the metaphyseal defect has been bone grafted the lateral condylar fragment is reduced. Now, temporary K-wire fixation helps to maintain reduction. Large clamps may help to keep large metaphyseal fragments reduced prior to definitive plate fixation either from the lateral or medial side.
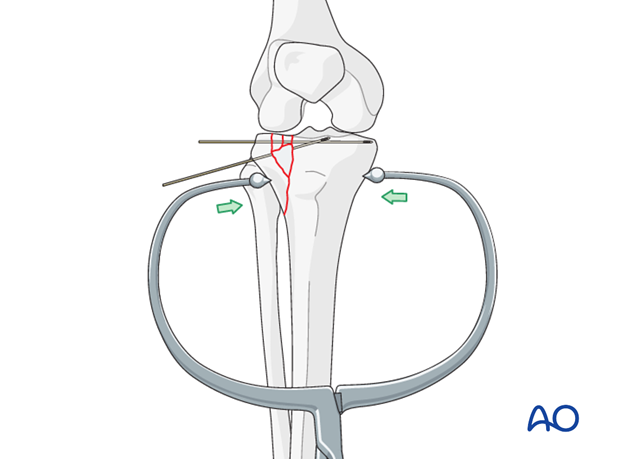
Plate osteosynthesis
Plate osteosynthesis represents the standard treatment for these fractures. The position of the plate is determined by the location of the fracture. The plate acts as a buttress, and compression of the articular fragments and large metaphyseal fragments is achieved by means of lag screws. Angular stable plates may be used, but are rarely necessary in monocondylar fractures except in osteoporotic bone.
Plate insertion
After preliminary fixation with K-wires prior to plate fixation, a clamp, if used for preliminary fixation, may have to be removed, but one must be very careful not to lose the reduction.
If the articular surface is very comminuted one must be careful not to overtighten the lag screws so as not to narrow and deform the articulation. Click here for a detailed description of the lag screw technique.
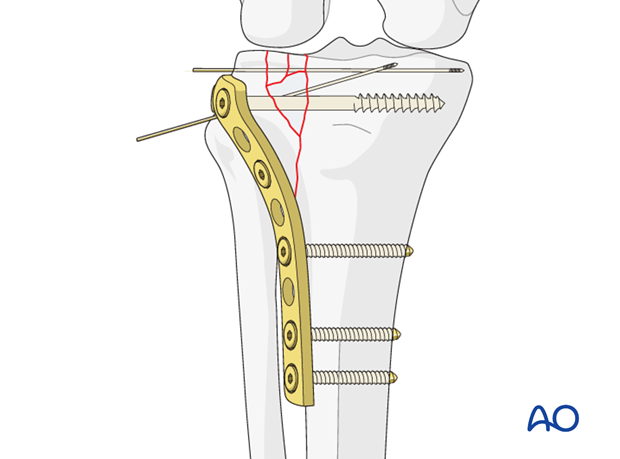
Plate fixation
Usually three screws are necessary to achieve adequate fixation of the buttress plate to the distal fragment. The number of screws in the proximal fragment will depend on the fracture pattern and the degree of comminution. Lag screw fixation of the articular surface is usually achieved by passing the lag screw outside the plate but may also be through the most proximal hole of the plate. This will depend on the fracture configuration because lag screws should be inserted at a right angle to the principle fracture plane. If one is using a plate with angular stability then fewer number of screws may suffice distally unless the bone is osteoporotic.
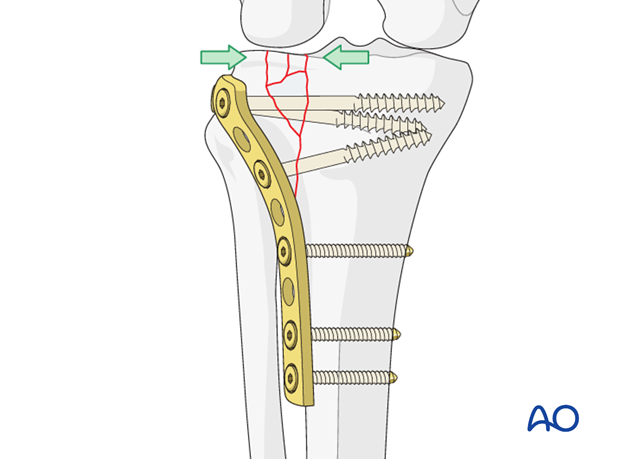
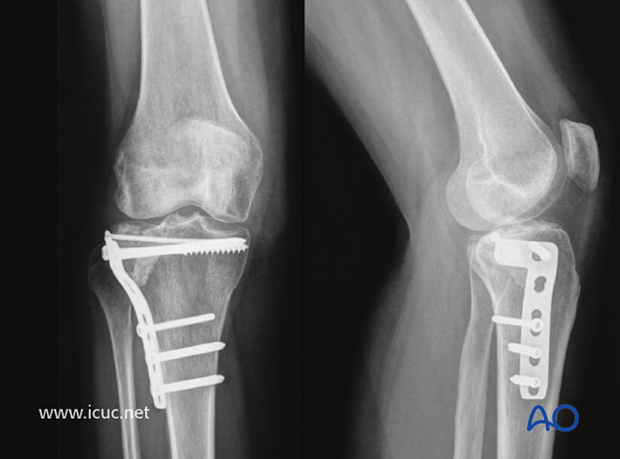
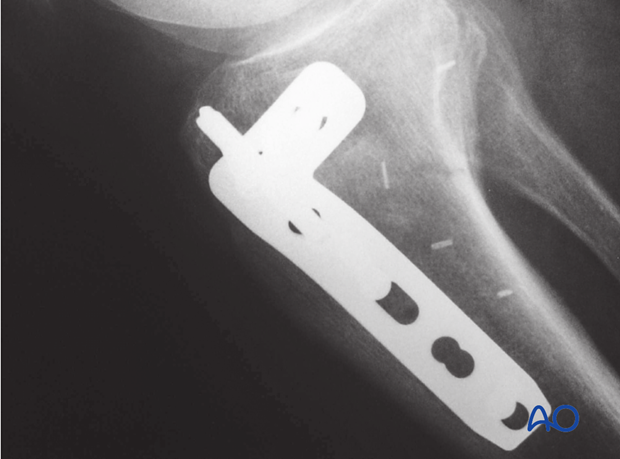
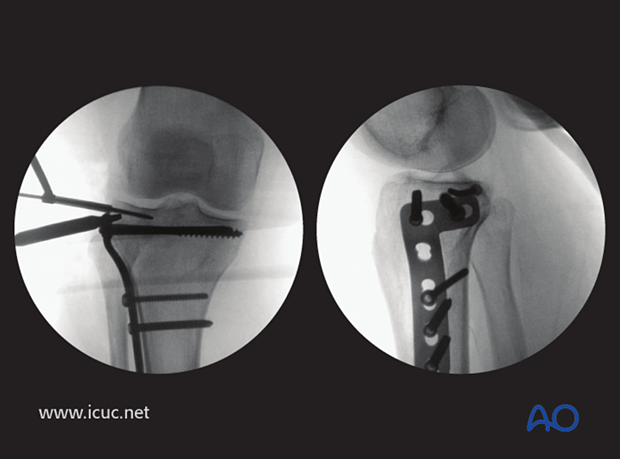
This image shows the final result with the use of a locking proximal tibia plate. Remember that a screw which locks in the plate will not act as a lag screw. Therefore, the first proximal screws should not be locking screws, and if partially threaded will exert compression. One then removes these screws one at a time and replaces them with fully threaded locking screws. The advantage of this is that interfragmentary compression is maintained while also achieving angular stability and stronger purchase in the proximal fragment.
6. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the tibial compartments should be carried out especially during the first 48 hours after surgery to rule out compartment syndrome.
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Unless there are other injuries or complications, mobilization may be performed on post OP day 1. Continuous passive motion (CPM) splints are very helpful in the early phase of rehabilitation. Static quadriceps exercises with passive range of motion of the knee should be encouraged. Afterwards special emphasis should be given to active knee and ankle movement.
Following any injury, and also after surgery, the neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently. The goal of early active and passive range of motion is to achieve as full range of motion as possible within the first 4 - 6 weeks. Optimal stability should be achieved at the time of surgery, in order to allow early range of motion exercises.
Weight bearing
No weight bearing in the treatment of articular fractures for a minimum of 10 – 12 weeks.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 6 and 12 week follow-up is usually performed. If a delayed union is recognized, further surgical care will be necessary and should be carried out as soon as possible.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.
7. Case
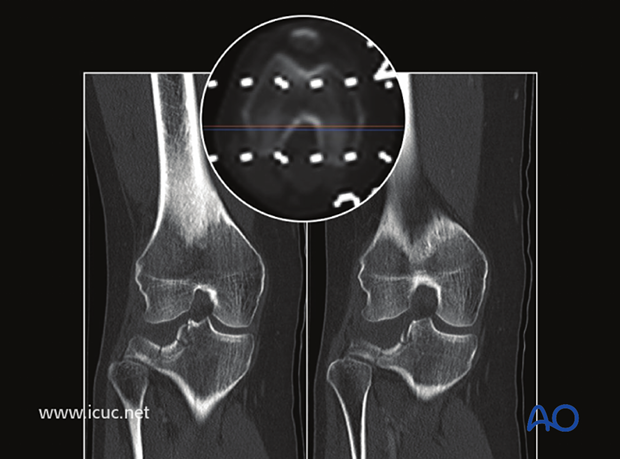
Lateral depressed tibial plateau fracture in a polytrauma patient. An external fixator has been applied during the early resuscitative phase. This allows for CT scanning with the knee in normal alignment. Although the femoral condyle is no longer applying pressure to the lateral tibial plateau, the fracture is still depressed.

Two images from CT showing the severe lateral tibial depression.
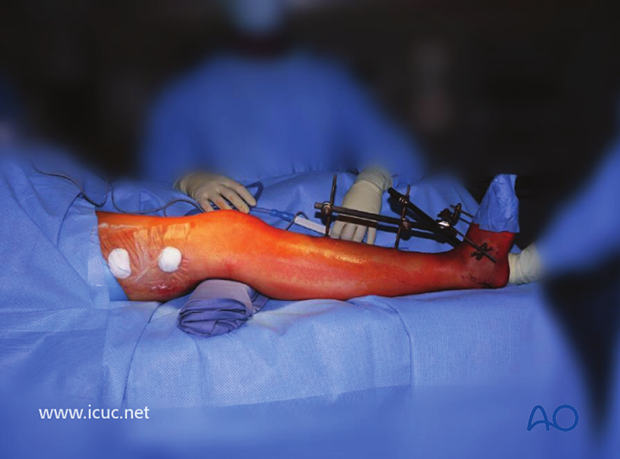
Sterile interoperative positioning for lateral plateau surgery. This patient also has a spanning frame for a severe distal tibial fracture.
Lateral approach to the proximal tibia with the fibular head outlined below and the tibial tuberosity outlined above, and an S-shaped incision between.
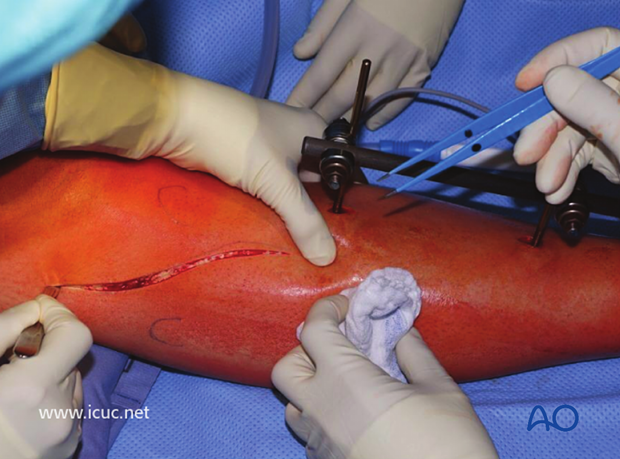
The anterior compartment has been opened and the surgeon is performing a subperiosteal dissection of the anterolateral tibial plateau.
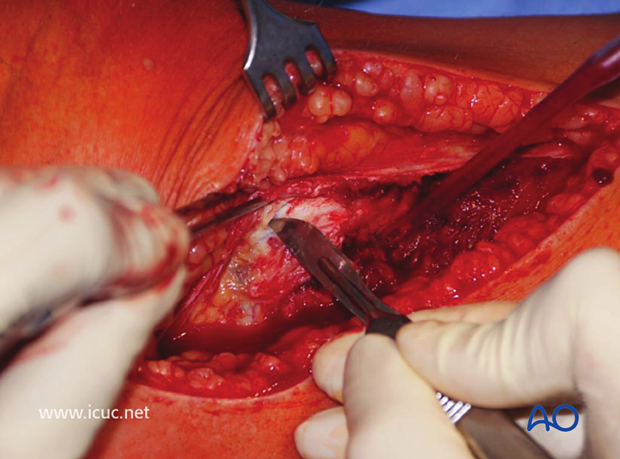
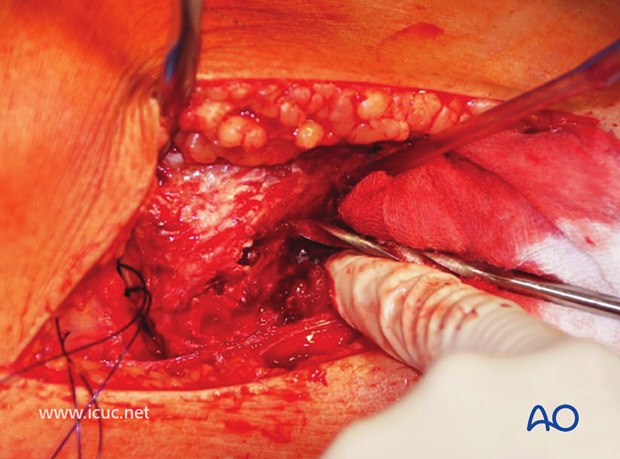
The joint is opened with a transverse incision below the meniscus.
With further dissection the distal femoral condyle can be seen behind the meniscus, and the lateral tibial plateau fracture is demonstrated.
Sutures are inserted into the meniscus to help with retraction and visualization. The split in the lateral tibial plateau is identified to facilitate reduction of the joint surface from below.
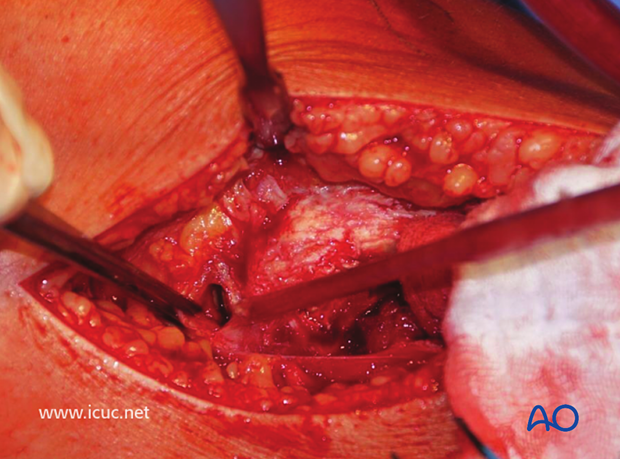
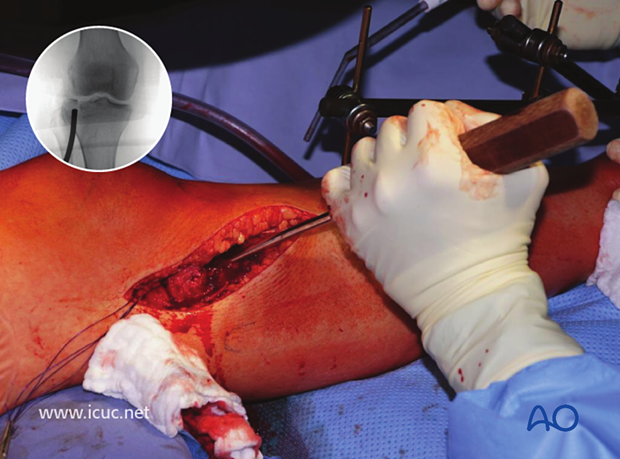
A drill is used to create a window for the insertion of the disimpaction tool.
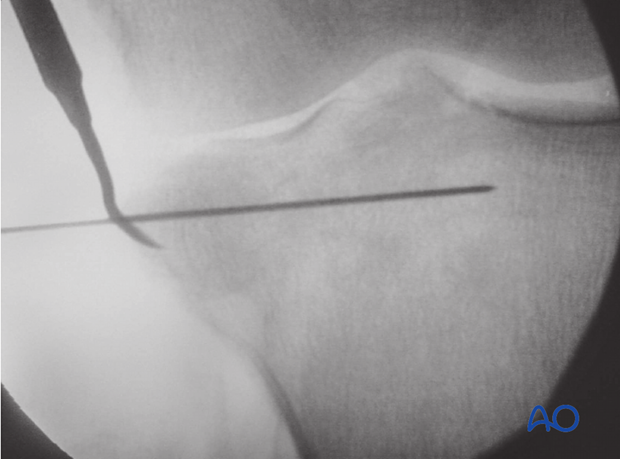
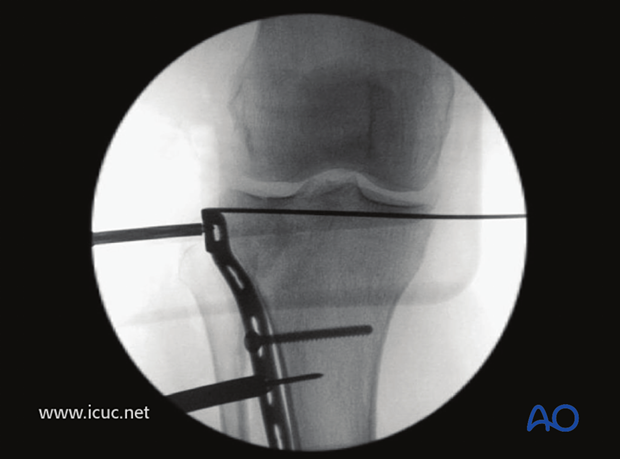
The disimpaction tool is inserted under fluoroscopic guidance and a large area is created underneath the fracture to ensure the whole impacted joint surface is lifted as one large piece.
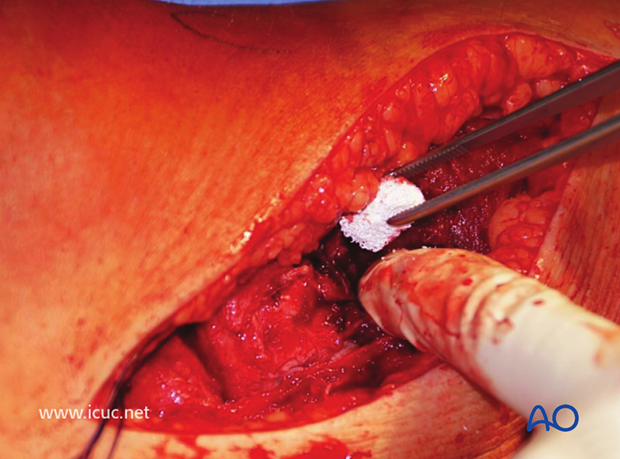
Once disimpaction is complete, then the use of calcium sulphate or calcium phosphate bone substitutes helps to fill the cavity and provide good structural support.
This image shows the joint surface reduced and the disimpactor maintaining reduction with a lateral K-wire is inserted beneath the joint surface.
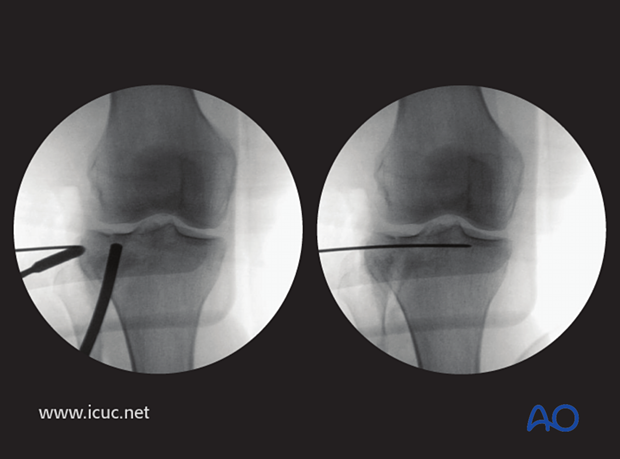
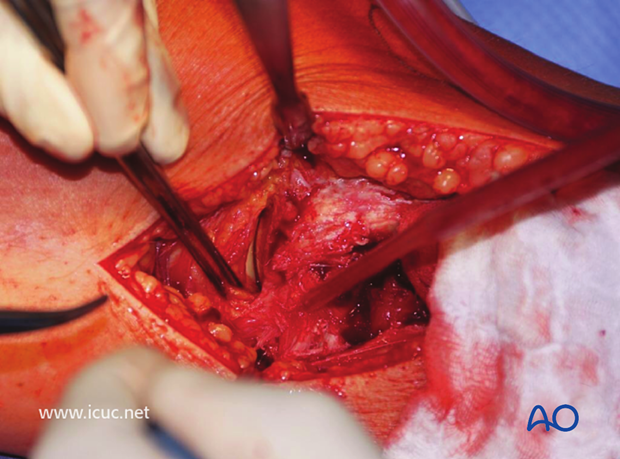
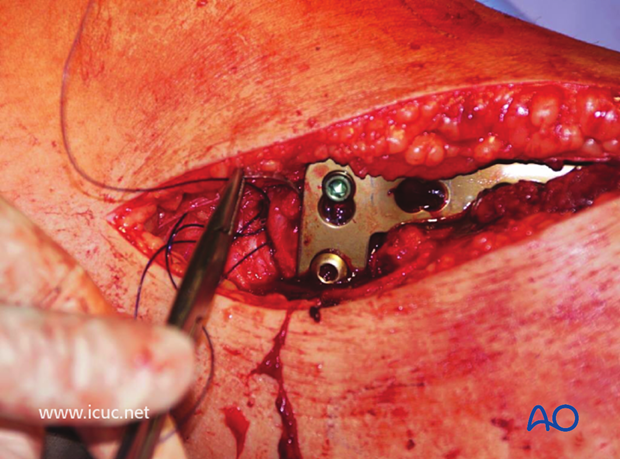
A lateral tibial plateau buttress plate is carefully inserted at the correct height.
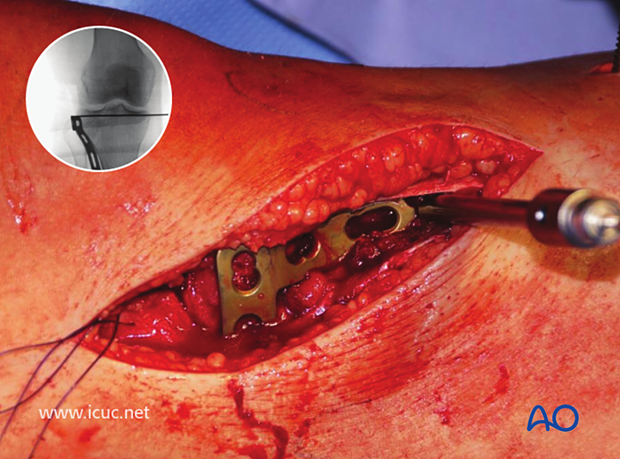
The oblique screw hole is filled first with a bicortical screw to allow for fine adjustments in the height of the plate. Note the K-wire has been driven out through the medial side of the knee so that it is still supporting the tibial plateau, but it is not interfering with plate positioning. It is not infrequent to use multiple small raft screws beneath the joint surface to support the reduction of the depressed area.
These image shows a cancellous screw inserted through the plate.
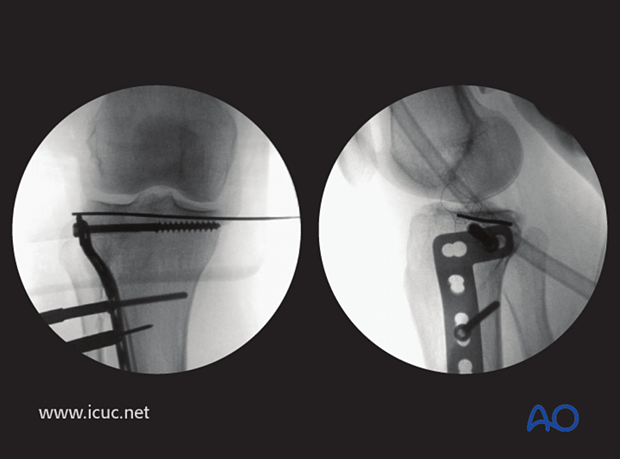
This image shows an extra subchondral raft screw being inserted to support the joint surface.
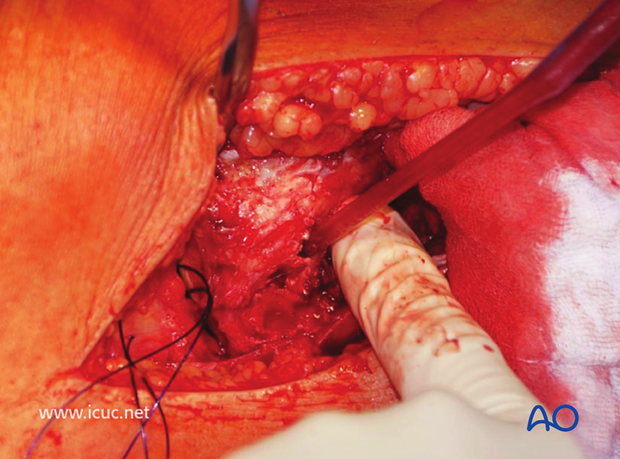
The sutures in the lateral meniscus are used to help position the meniscus appropriately on the reconstructed tibial plateau.
The anterior compartment may be closed if compartment syndrome is not a threat. If in doubt, this compartment should be left open.
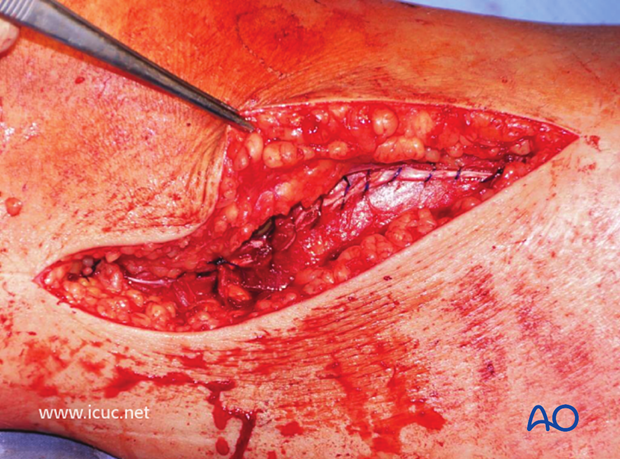
A subcuticular suture was used for skin closure.

12-week image showing a very good reduction but some loss of joint height despite raft screws.
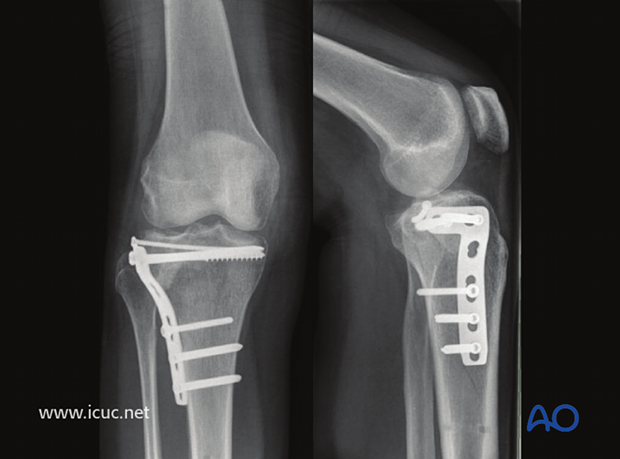
Nearly one year later, bone substitute can still be seen and small loss of joint height is evident. The lateral tibial plateau is quite forgiving as far as late consequences of a fracture because of the large meniscus that covers the joint surface.