ORIF - Conventional plates
1. Principles
General considerations
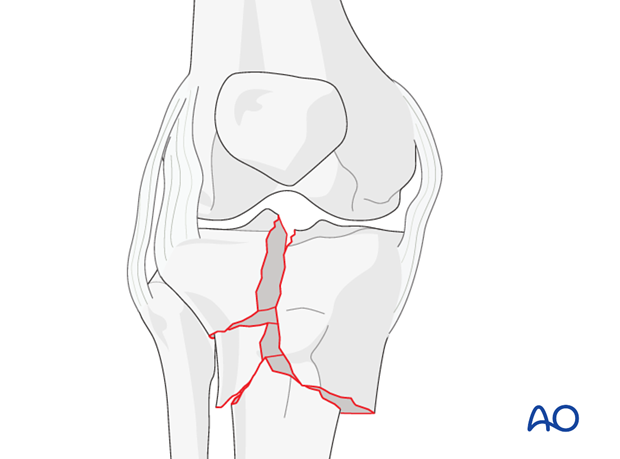
Anatomical reduction of the articular surface is mandatory. Reduction of the metaphyseal fracture depends on the degree of comminution. If possible, reduce anatomically but remember that it is more important to retain vascularization of the bony fragments than to achieve their anatomical reduction.
Main steps in treatment include:
- Temporary reduction and immobilization until definitive surgery (eg, external fixator).
- Adequate preoperative planning (is a bone graft necessary, what type of approach, the number and type of implants, and any additional equipment).
- Make an arthrotomy between the meniscus and the tibia. This will allow for adequate visualization of the articular fracture. Inspect the meniscus for any tears. These will have to be repaired at the end.
- Anatomical reduction of the articular surface and absolutely stable fixation if possible.
- Reduction of the metaphysis and provisional fixation with K-wires.
- Definitive stable fixation of the metaphysis using screws and plate(s) with preservation of the blood supply of the metaphyseal fragments.
Timing of surgery
Surgery should be delayed until full recovery of soft tissues (swelling, blisters, abrasions, etc). This takes usually 3 to 10 days.
Until surgery, length of the leg should be maintained (eg, external fixator, traction, etc).
Plate location
Plate location depends on the fracture morphology. The plate is used to buttress the fragments. On the medial side, if the fracture morphology allows, the plate may be placed on the anteromedial surface. Most commonly, the wedge fragment is split off in such a way that to buttress it adequately the plate must be positioned posteromedially.
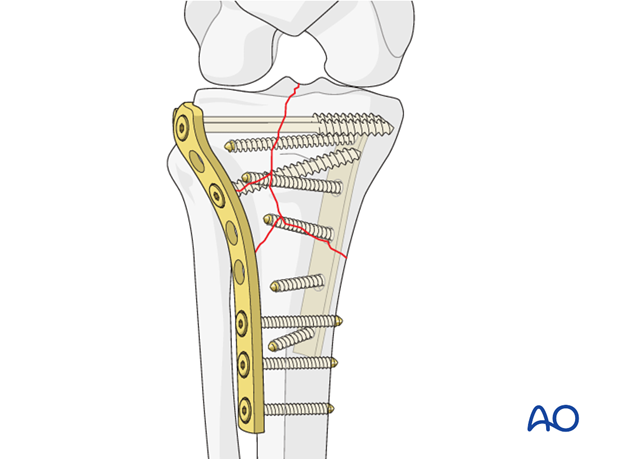
Double plating
In order to prevent collapse these fractures require buttressing on the medial as well as lateral side. The position of the medial plate will depend on the fracture pattern. Most often it is positioned on the posteromedial crest of the tibia.
Medial or lateral side first?
Most often the medial fragment is less comminuted and should be addressed first to restore the anatomical relationship of the medial joint surface, original length and rotation. Therefore, in the majority of cases the medial approach is carried out first and the medial fracture is reduced and fixed provisionally with a buttress plate with the minimum number of screws necessary. Because occasionally the reduction and fixation of the medial side has to be readjusted as the lateral side dealt with.
The lateral fracture is addressed next. Once a satisfactory reduction and fixation is reached on the lateral side, the fixation on the medial side is completed and the wounds are closed in a routine fashion.
Potential complications
- Articular damage
- Vascular and nerve injury (peroneal nerve)
- Compartment syndrome
Check for these during surgery. Do not close the fascia to prevent compartment syndrome.
2. Preparation
Patient positioning
Depending on the approach, the patient may be placed in the following positions:
Use of a tourniquet
A tourniquet should be applied in every case. Whether the tourniquet is used depends on the amount of bleeding. Exsanguinate the limb by elevating it.
Use of a radiolucent table
To allow for intraoperative radiographic control of reduction and fixation, the use of a radiolucent table is mandatory.
Preparation for bone graft
If autologous bone grafting is planned the anterior iliac crest should be prepared and draped as well as the limb.
3. Approaches
Not all complete articular fractures can be perfectly reduced through a medial/posteromedial and/or an anterolateral approach. Sometimes fractures with a flexion injury mechanism need to be addressed through a posterior approach as well.
4. Preliminary reduction
General consideration
Rotation, length and axial alignment should be restored first by axial traction (distractor, external fixator or manual traction).
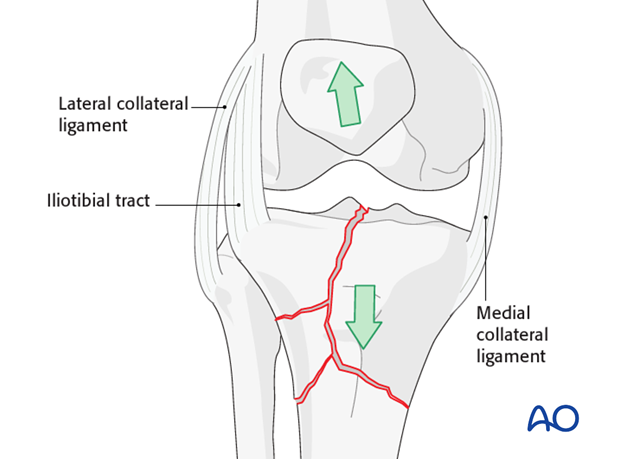
Ligamentotaxis
Ligamentotaxis helps to achieve preliminary reduction of the main fracture fragments and helps to maintain length during the operation. It is also used preoperatively to maintain provisional reduction.
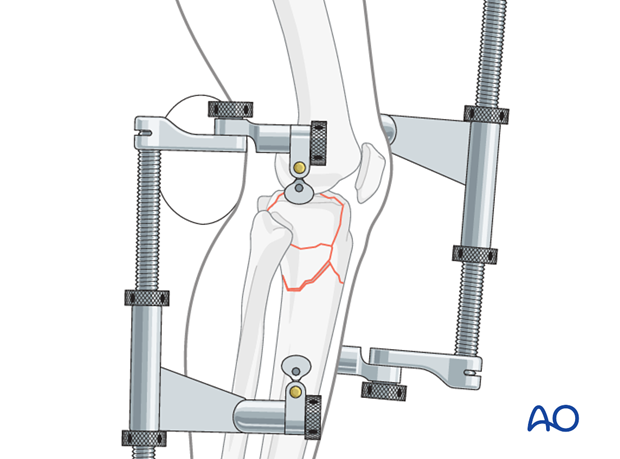
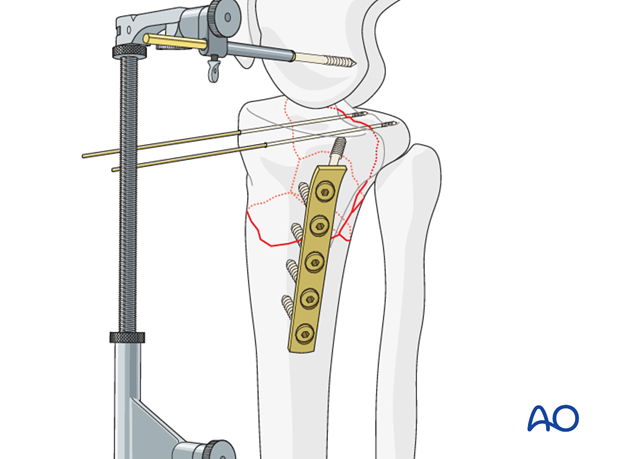
Use of distractors and/or external fixators
In order to reduce these complex fractures one may need to use two femoral distractors one on the medial and one on the lateral side. To do this place the knee in slight flexion.
One can also achieve the same with the use of two external fixators or one distractor and one external fixator. The use of the external fixators makes intraoperative adjustments almost impossible because they do not allow for rotational or angular correction.
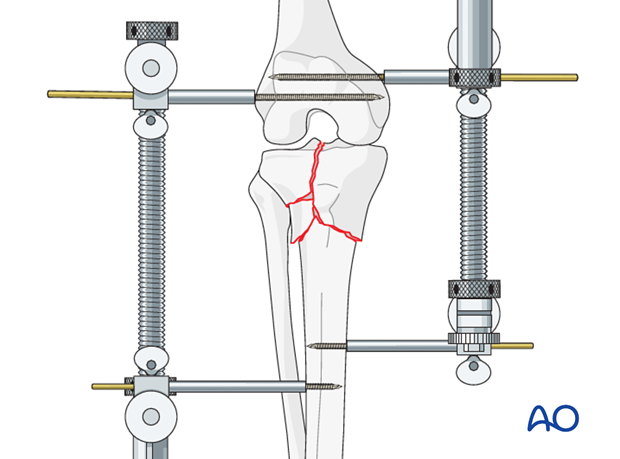
Distractors, because they apply the force directly to the bone, are very powerful and make distraction easy. Use the distractor on the side with more comminution. Usually, the medial side can be managed with an external fixator because it is usually less comminuted. If only external fixators are available, place one on the medial and one on the lateral side or span the knee joint anteriorly with a unilateral frame.
5. Reduction of the articular surface
Reduction of the articular surface with clamps
In rare situations where the articular fragments are large, their reduction may be achieved by percutaneous manipulation with clamps and joy sticks. Most often, the joint has to be exposed in order to achieve an anatomical reduction. If only percutaneous manipulation is used, reduction must be checked with either a C-arm or an arthroscope.
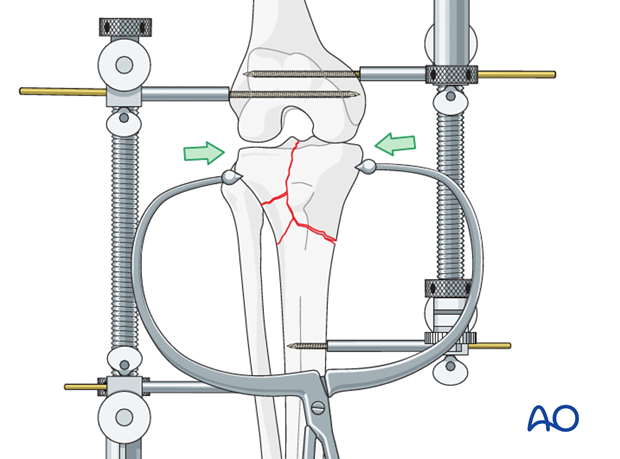
Pearl: clamp over plate
If you intend to keep the clamp on throughout the whole procedure, it is best to slip the plate under the clamp prior to its tightening to maintain reduction. From your preoperative plan and/or intraoperative trail you will know which screw hole is best for placement of the clamp.
Secure reduction
Once reduced, secure the provisional fixation with K-wires.
Verify the reduction with the help of image intensification.
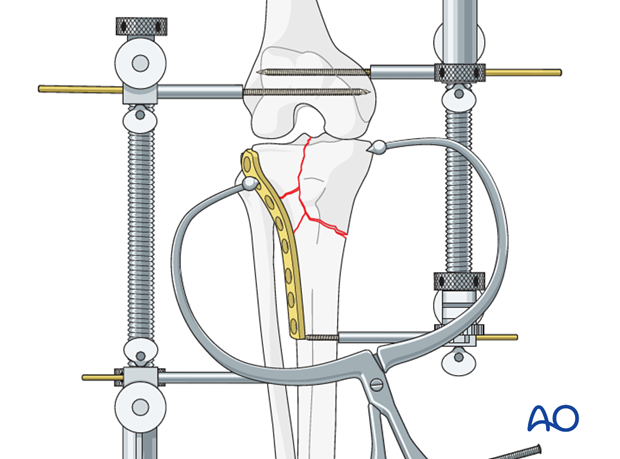
6. Medial column fixation
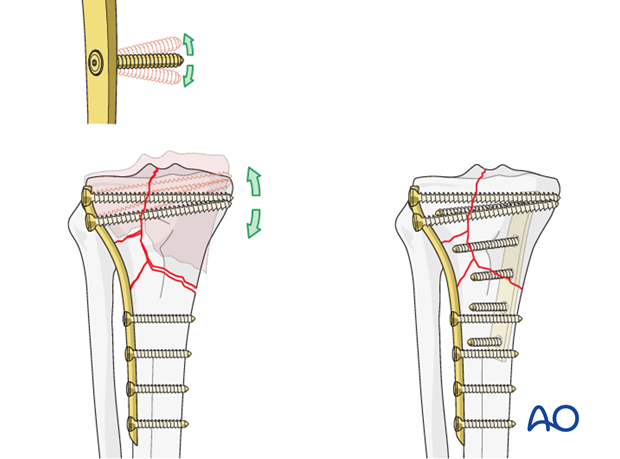
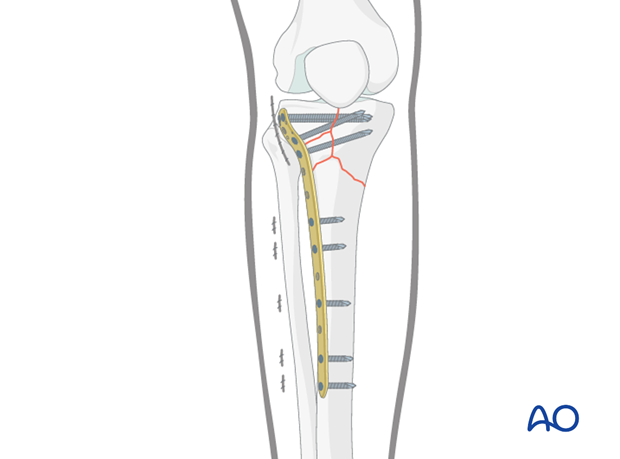
Plate application on medial side
A medial plate is applied and secured with screws. Some of these may be only unicortical if fixation is meant to be provisional.
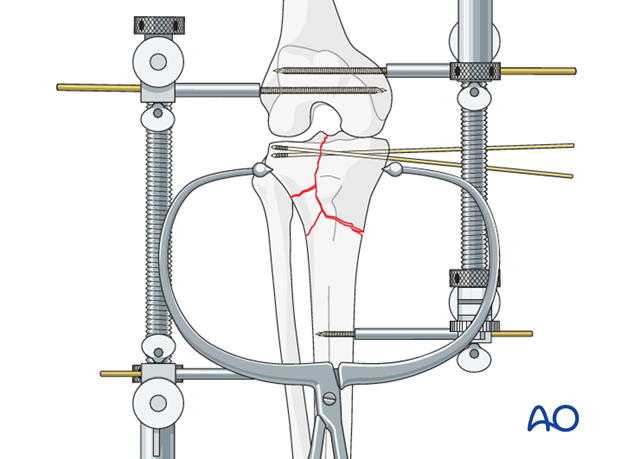
7. Lateral column fixation
Placement of lag screw
The placement of the lag screw or screws used to achieve absolute stability of the articular surface is determined by the fracture pattern. Ideally, these screws should be inserted at right angle to the fracture plane.
The buttress plate, once properly contoured, is inserted on top of the periosteum deep to the muscle envelope. The most proximal screw if it fits with the fracture morphology may be a lag screw.
Click here for a detailed description of the lag screw technique.
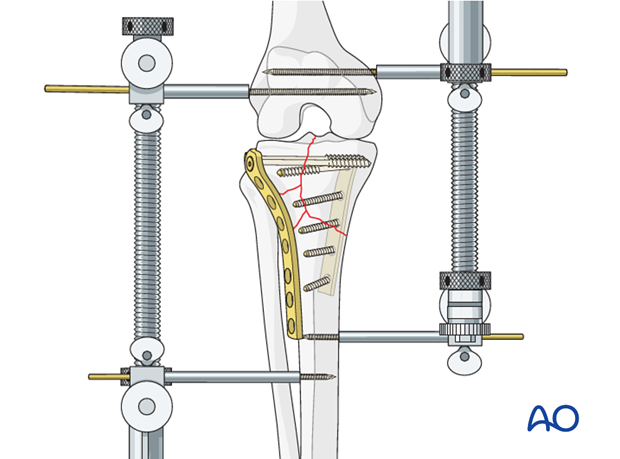
Additional screw placement
K-wires may be removed once fixation is achieved. The number of screws on each side of the fracture depends to some degree on the fracture configuration. Distal to the fracture, one should aim for at least two to three cortex screws for plate fixation to the distal fragment.
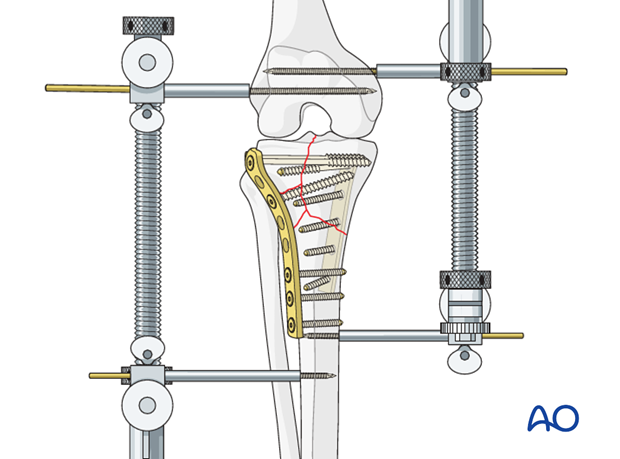
Final osteosynthesis
At the end, once stable fixation has been achieved and checked with the image intensifier, remove the distractor(s).
8. Alternative: angular stable plate
If one is using a plate with the possibility of angular stability like the lateral tibial plate with locking screws or the LISS for the tibia and the fracture configuration is such on the medial side that once reduced there is inherent stability, one can consider to leave out the medial plate.
9. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the tibial compartments should be carried out especially during the first 48 hours after surgery to rule out compartment syndrome.
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Unless there are other injuries or complications, mobilization may be performed on post OP day 1. Continuous passive motion (CPM) splints are very helpful in the early phase of rehabilitation. Static quadriceps exercises with passive range of motion of the knee should be encouraged. Afterwards special emphasis should be given to active knee and ankle movement.
Following any injury, and also after surgery, the neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently. The goal of early active and passive range of motion is to achieve as full range of motion as possible within the first 4 - 6 weeks. Optimal stability should be achieved at the time of surgery, in order to allow early range of motion exercises.
Weight bearing
No weight bearing in the treatment of articular fractures for a minimum of 10 – 12 weeks.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 6 and 12 week follow-up is usually performed. If a delayed union is recognized, further surgical care will be necessary and should be carried out as soon as possible.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.













