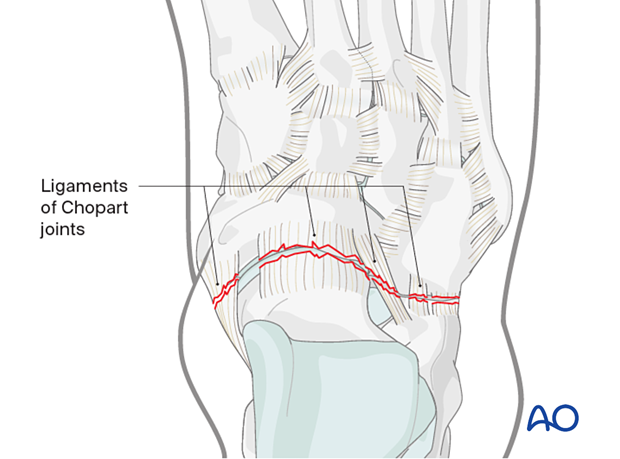
Treatment of Chopart injuries
1. General considerations
Goal of surgery
The goals of surgery for the treatment of Chopart injuries are:
- Reduction of dislocated Chopart joint
- Joint reconstruction
- Axial alignment with the restoration of the normal relationship of the lateral and medial column
- Stabilization of the Chopart joint
The general sequence of the treatment
This general sequence of treatment can be applied:
- Decompression of compartment syndrome, if necessary
- Reduction of Chopart dislocation and other associated fracture-dislocations
- The management of soft tissue injuries, which is achieved by applying a temporary external fixator
- Once the soft tissues allow for surgical intervention, address the intraarticular injuries with care to align the medial and lateral columns. If there are several bony injuries, one would typically address the simplest fractures first to ensure a more reliable reduction. Below we will list the available treatments for the various bony injuries
- Address any residual ligamentous instability of the Chopart joint
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Reduction of the dislocated Chopart joint
One should always attempt to perform a closed reduction of the dislocation. If this fails, an open reduction must be performed independently of the soft-tissue state.
Closed reduction
Under anesthesia, apply manual traction in the axial vector and reverse the mechanism of the injury.
Open reduction
If closed reduction maneuvers are unsuccessful in obtaining an anatomic reduction of the joint(s), the failure can be due to bone interference, soft tissue interposition, or both.
A direct open reduction will be necessary.
3. Patient preparation and surgical approach
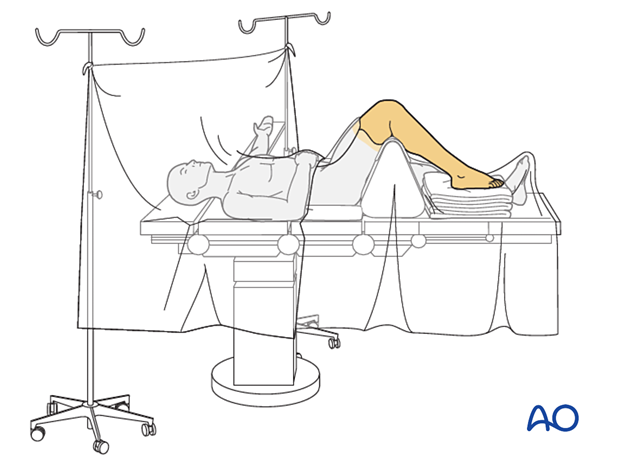
Patient positioning
The procedure is performed with the patient placed supine with the knee flexed 90°.
Medial approaches
The talus head can be approached through the medial utility or dorsomedial approach.
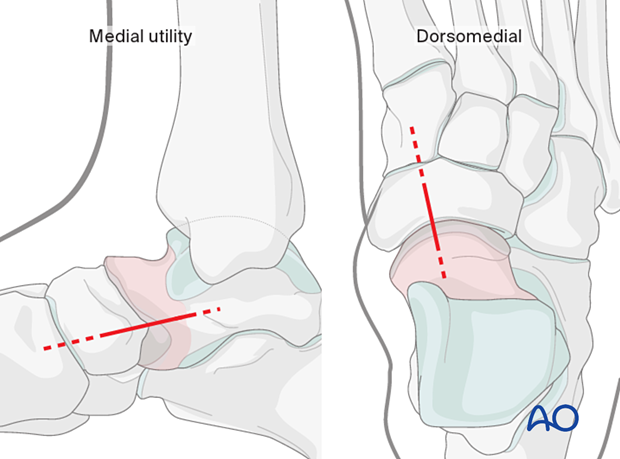
The navicular can be approached through the dorsomedial approach.
Lateral approaches
The anterior process of the calcaneus and the cuboid can be addressed through the dorsolateral approach.
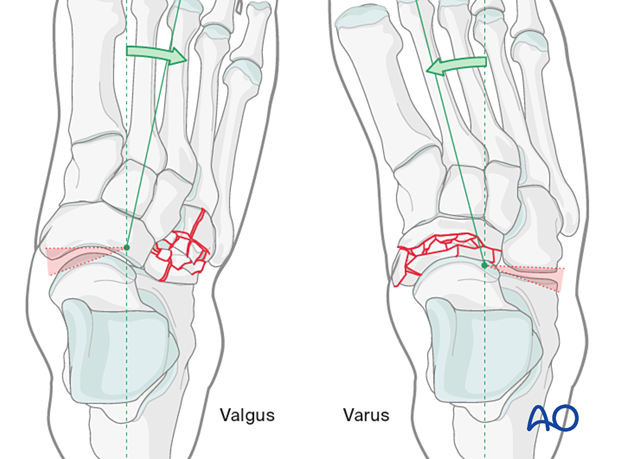
4. Varus injury
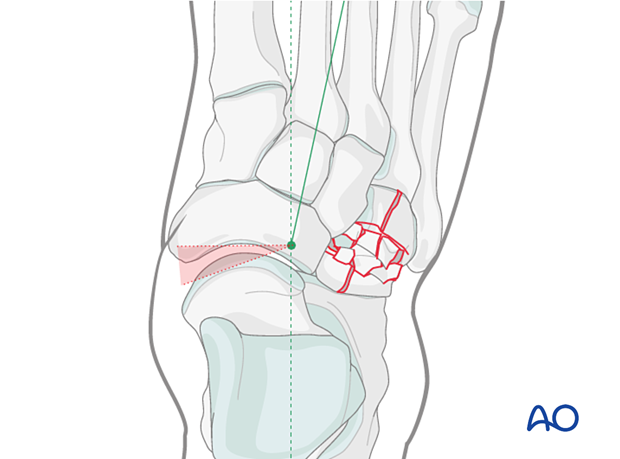
A varus injury is composed of compression of the medial column and a distraction of the lateral column.
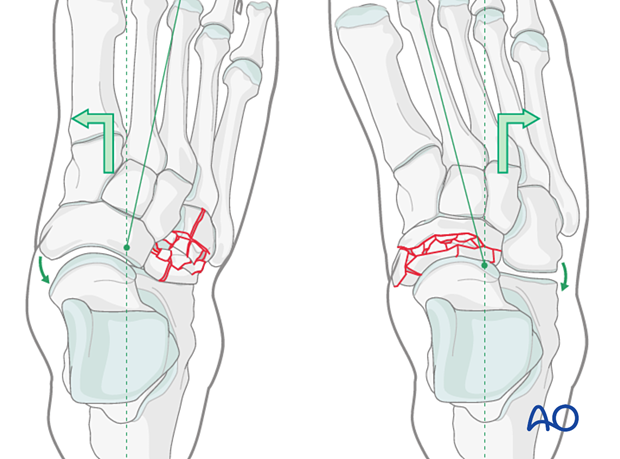
Reduction and fixation of the lateral column
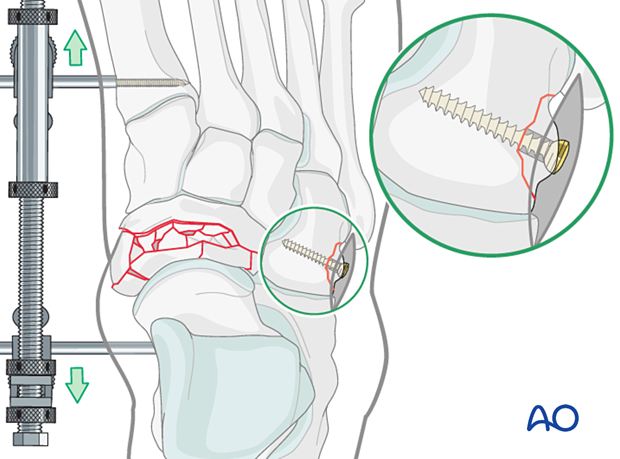
A medial distractor assists in obtaining a reduction.
If reduction of the medial column injury is obtainable, the lateral column injury may be addressed first.
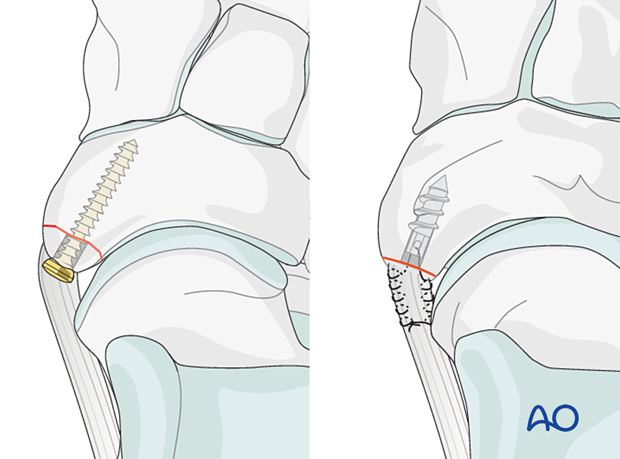
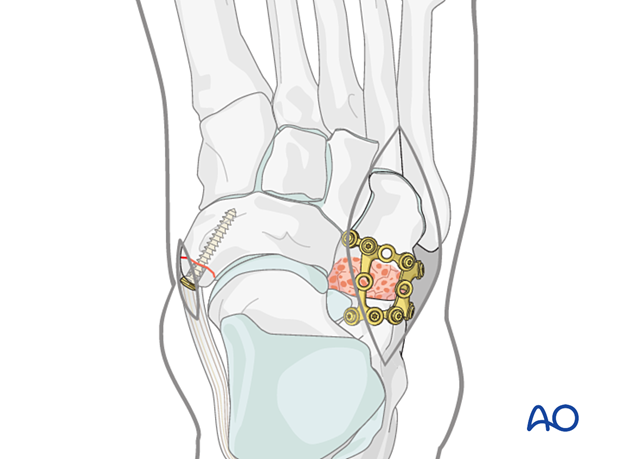
An avulsion fracture of the cuboid is treated with a lag screw. In contrast to lag screws inserted in the diaphysis, these lag screws will typically not penetrate the far cortex, as this would damage the opposite articular surface.
A lateral column ligamentous injury can be stabilized with transfixion K-wires or direct suture repair.
Reduction and fixation of the medial column
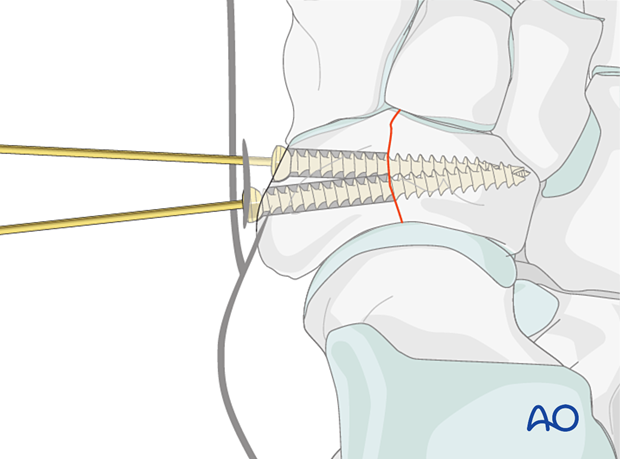
Simple complete articular fractures of the navicular can be treated with lag screw fixation.
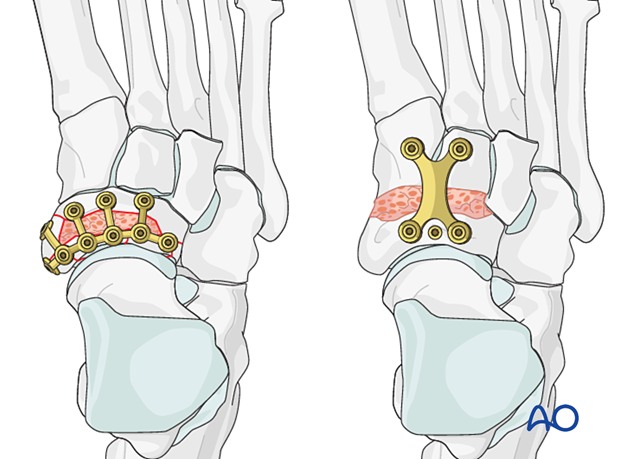
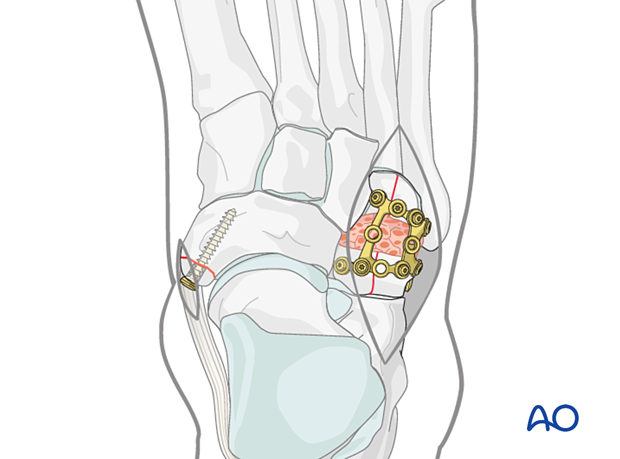
Multifragmentary complete articular fractures are addressed with ORIF, fusion, or bridging, depending on the injury.
- ORIF of navicular with reconstructable articular surfaces
- Fusion of unreconstructable naviculocuneiform joint
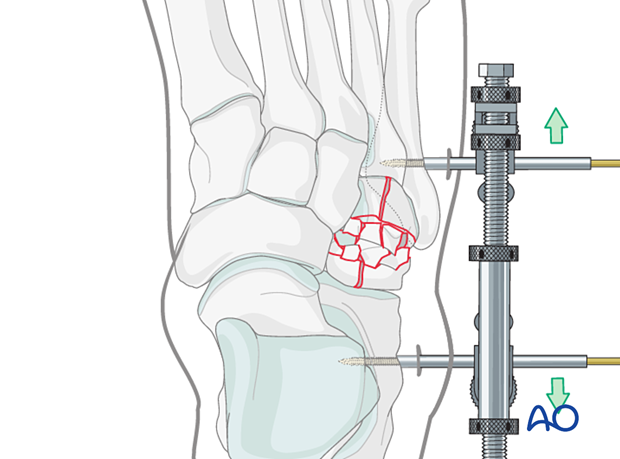
Temporary bridging or medial column external fixation may be needed to maintain the length of the medial column.
Due to the talonavicular joint’s importance for hindfoot circumduction, a fusion of an unreconstructable talonavicular joint should be avoided. Instead, consider bridging the unreconstructable joint until healing has occurred.
5. Valgus injury
A valgus injury consists of a compression injury of the lateral column and a distraction injury of the medial column.
Reduction and fixation of medial-column distraction injury
A lateral distractor assists in obtaining a reduction.
If reduction of the lateral column injury is obtainable, the medial column injury may be addressed first.
Any avulsion fracture of the navicular is fixed:
Due to the talonavicular joint’s importance for hindfoot motion, the fusion of an unreconstructable joint should be avoided.
Reduction and fixation of lateral compression injury (“nutcracker injury”)
Reconstructable articular surfacesComplete articular fractures with reconstructable articular surfaces are treated with open reduction and fixation.
- ORIF - Lag screw fixation of simple fracture
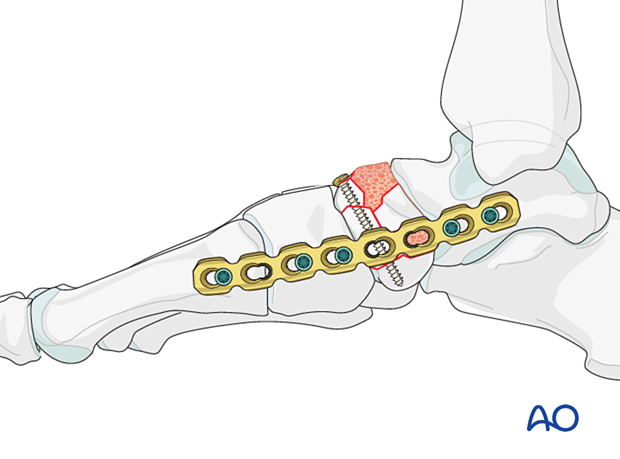
- ORIF - Bridge plate fixation of multifragmentary fractures
Temporary bridging or lateral column external fixation may be needed to maintain the length of the lateral column.
Loss of lateral column length will lead to a flatfoot deformity and peritalar subluxation.
An unreconstructable articular surface may be fused.
Temporary bridging or lateral column external fixation may be needed to maintain the length of the lateral column.
6. Stabilization of residual instability
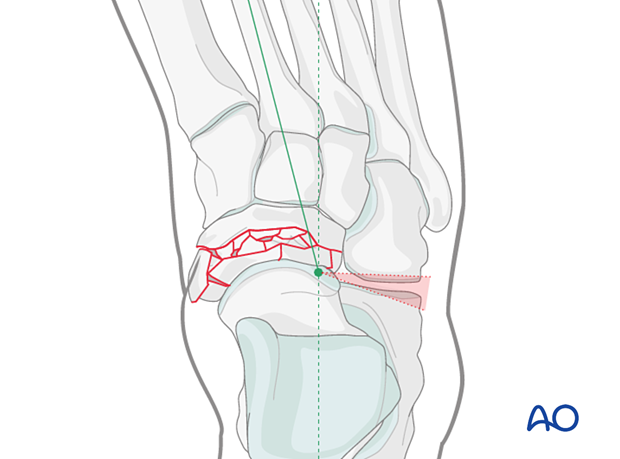
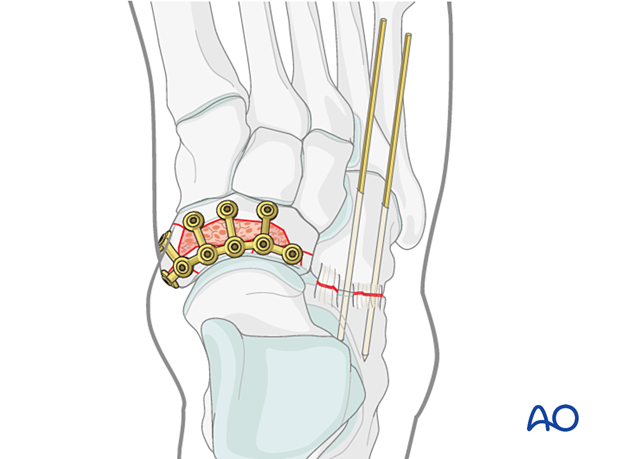
Any residual instability of the Chopart joint following ORIF of the bony injuries is treated with temporary transfixion K-wires.
Insert a minimum of two 1.8 mm K-wires perpendicular to the joint surface(s) in each unstable column.
Possible K-wire trajectories are illustrated below.
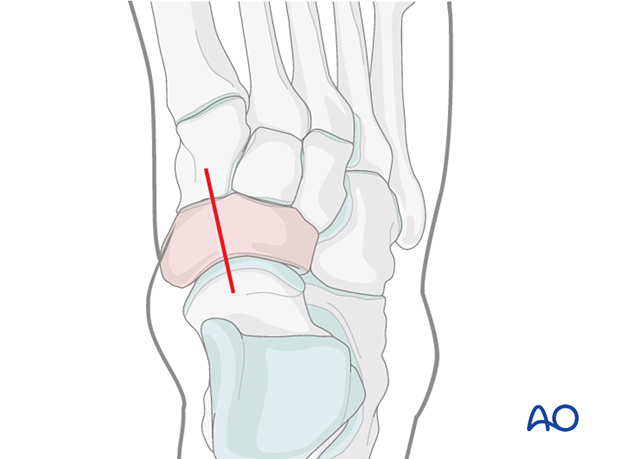
Medial transfixion
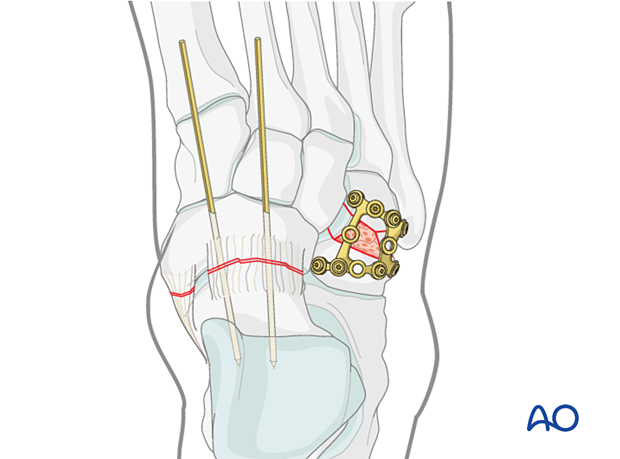
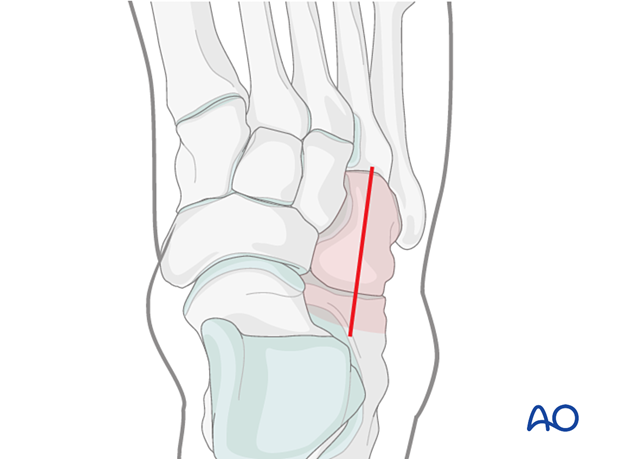
Lateral transfixion
7. Aftercare
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
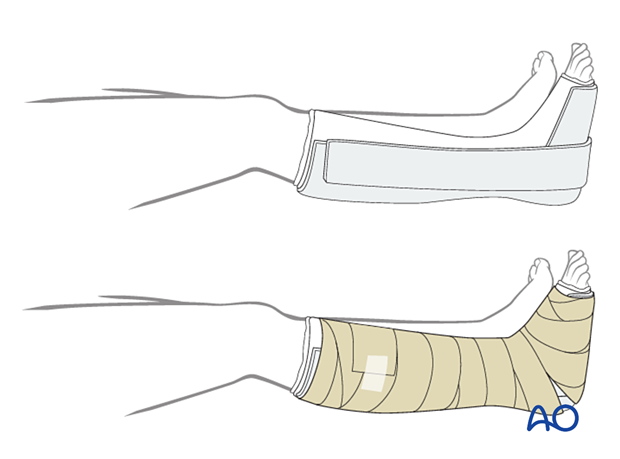
Follow-up
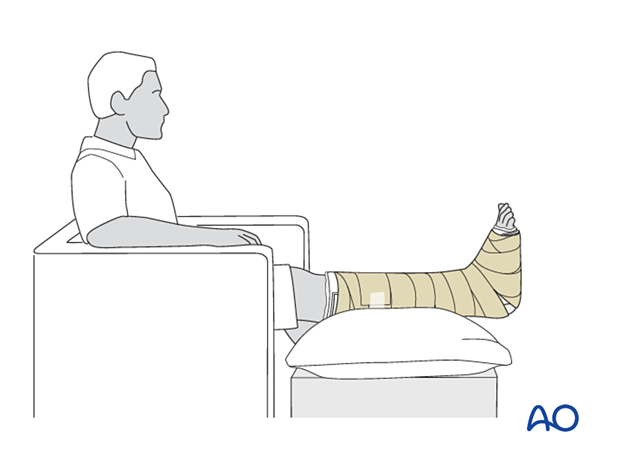
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













