Primary fusion of unreconstructable calcaneocuboid joint
1. Introduction
Goal of surgery
The goal of the treatment is bone healing with appropriate intra- and extra-articular reduction to maintain lateral column length. Early weight-bearing may be tolerated depending on the fracture pattern.
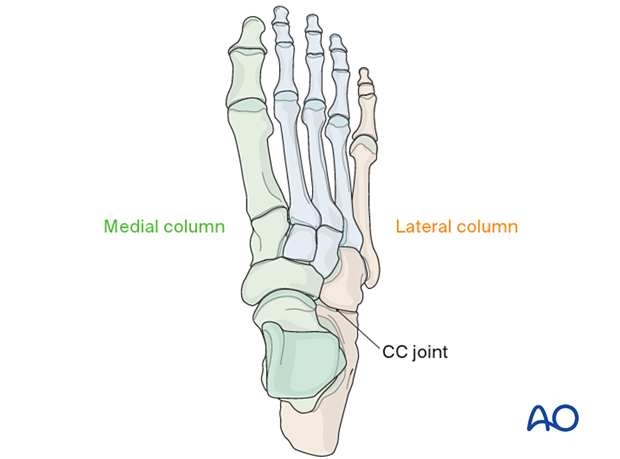
CC joint
Unlike the TN joint, which is responsible for complex hindfoot circumduction, the CC joint is less important for normal function. If fused at normal length, no loss of motion in the rest of the hindfoot occurs.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

Anatomic function
The calcaneocuboid joint and the talonavicular joints are responsible for complex hindfoot circumduction.
Lateral column length is critical to maintaining the shape and function of the foot. Therefore, the cuboid length must be maintained.
2. Patient preparation and surgical approach
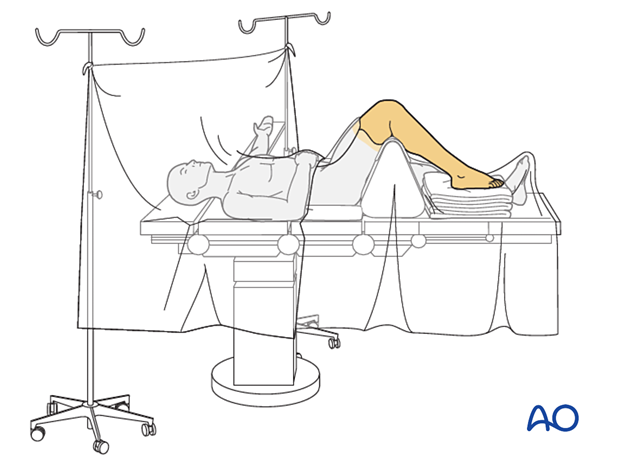
The procedure is performed with the patient placed supine with the knee flexed 90°.
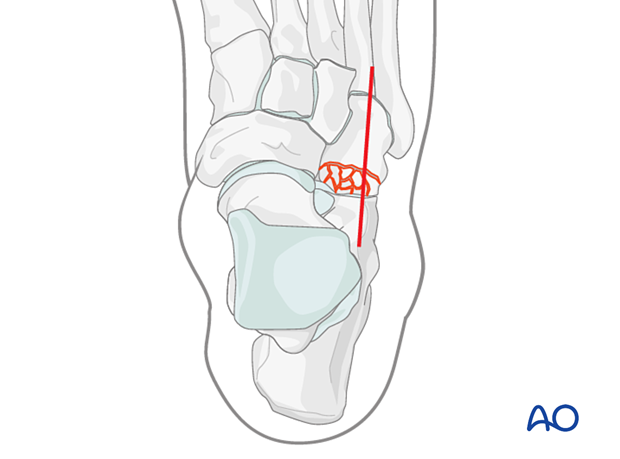
Fractures of the cuboid are best approached through the dorsolateral approach to the cuboid.
The soft tissues, including capsule and periosteum, are often disrupted. Care should be taken to minimize soft-tissue stripping during the approach, which will help maintain the blood supply to the fragments.
3. Visualization
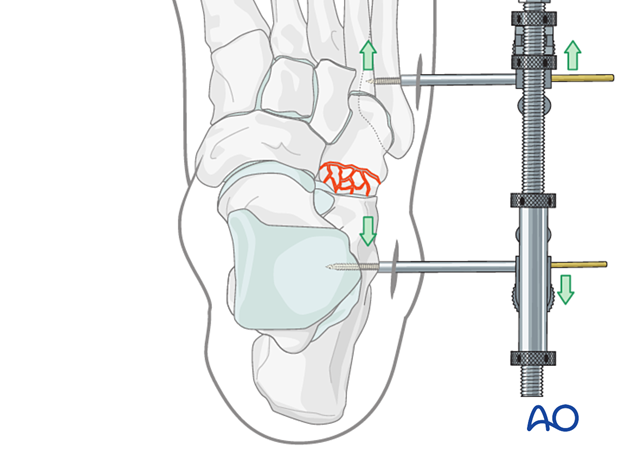
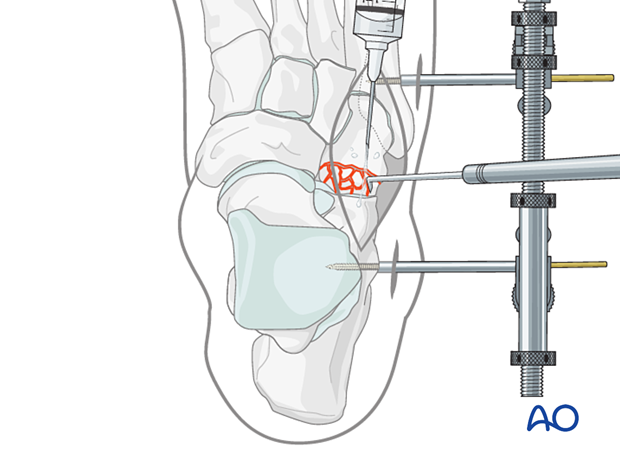
Distraction
Use a lateral-column distractor to achieve the articular surface visualization needed for accurate reduction and fixation.
Distraction is essential when dealing with comminution or a delay between the injury and the definitive reduction.
Insert the external fixator pins in the calcaneum through stab incisions, proximally in the calcaneum, and distally in the fifth metatarsal.
The distraction vector should be parallel to the plantar aspect of the lateral foot.
The fracture is distracted to allow complete visualization of either joint surface as needed.
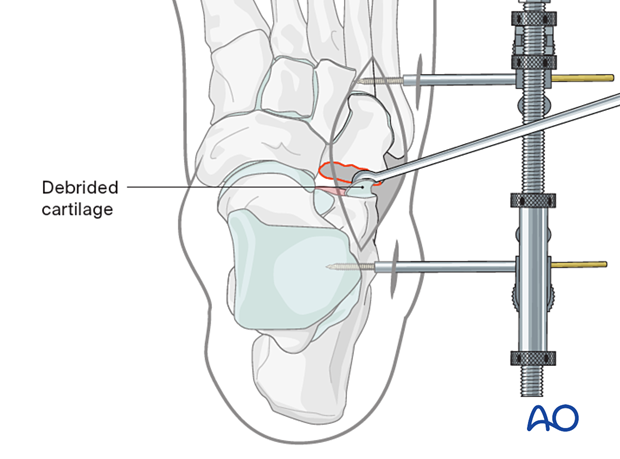
Debridement
Irrigate the fracture site using, eg, a syringe.
Fracture fragments are debrided and mobilized with a dental pick or Freer elevator.
4. Fusion
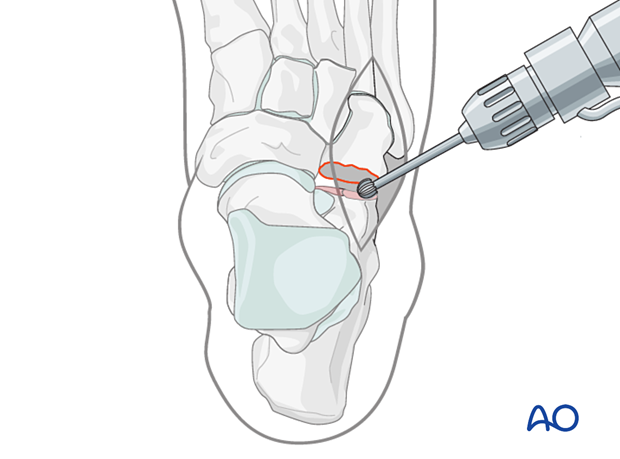
Preparation of the calcaneal articular surface
Remove the cartilage from the anterior facet of the calcaneum using a curette.
Penetrate the subchondral bone using a high-speed burr or drill to promote bone growth.
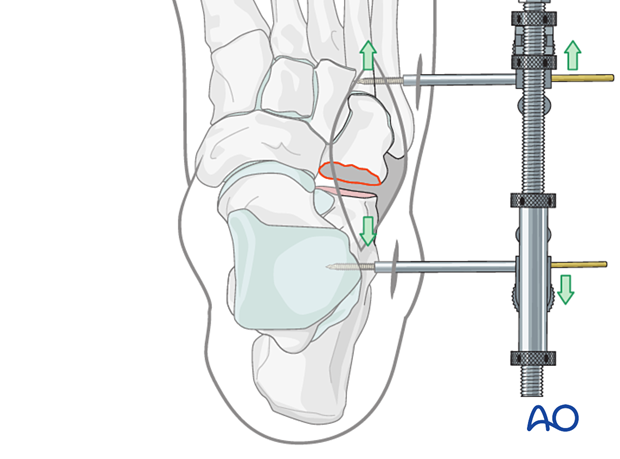
Establishment of correct cuboid length
Once the fusion site is prepared, the distraction can be adjusted to achieve the correct length of the lateral column.
It is helpful to have comparative x-rays from the uninjured side, allowing proper length and morphology to be judged.
Grafting
The defect can be grafted using a corticocancellous bone graft for structural support. The graft is harvested from either the distal or proximal tibia.
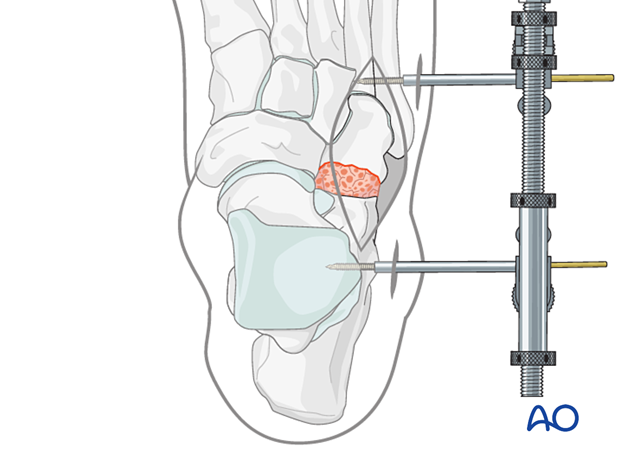
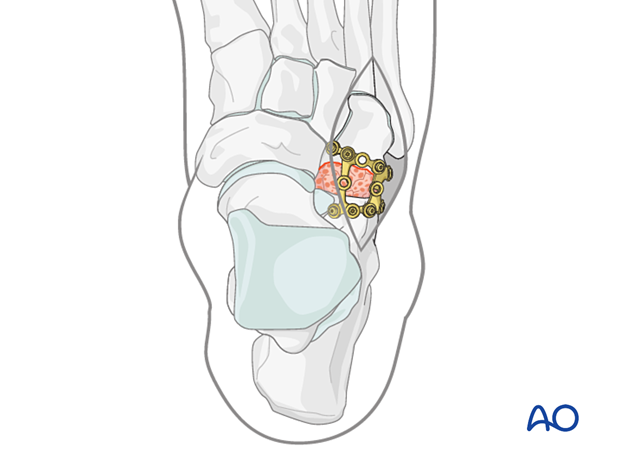
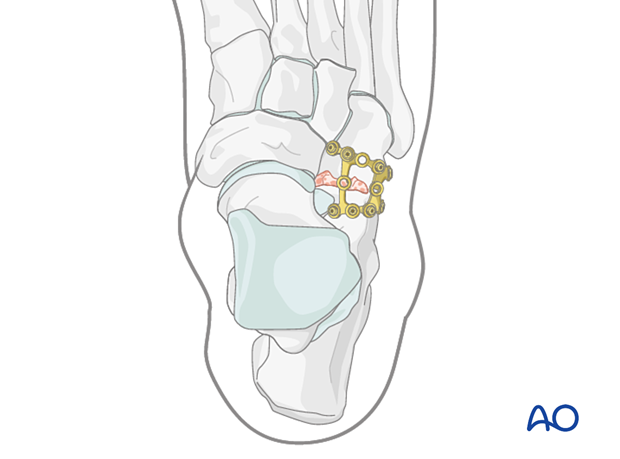
Plate fixation
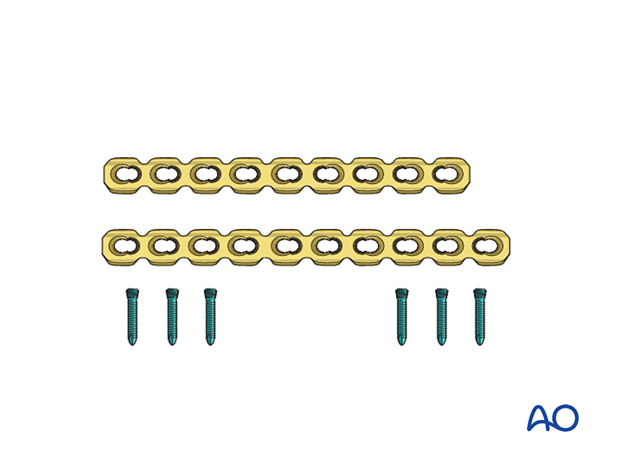
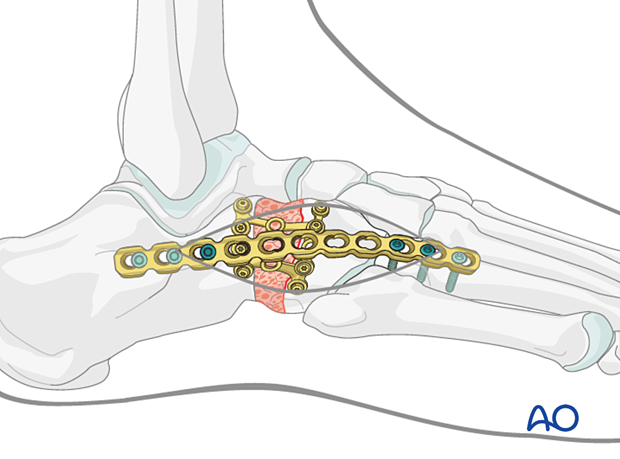
An appropriate locking plate is selected to bridge the defect.
A mesh plate can be used for larger defects and a cuboid plate for smaller defects.
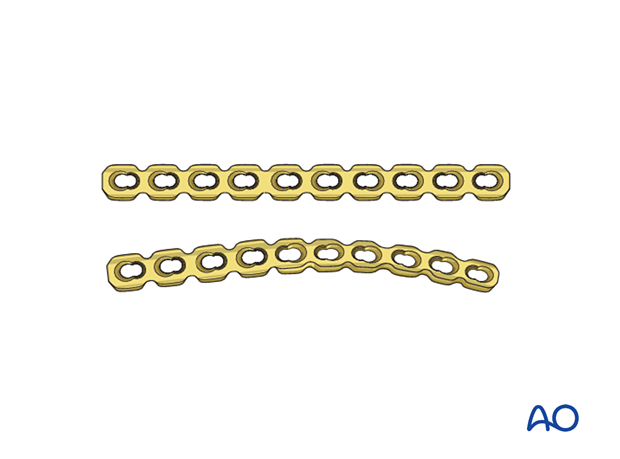
Contour the plate to fit the cuboid anatomy.
When contouring locking plates, care must be taken not to deform the screw holes.
The plate is fixed with locking head screws.
Quality control
Using intraoperative imaging, verify:
- Restoration of the appropriate length of the lateral column
- Appropriate screw placement and length
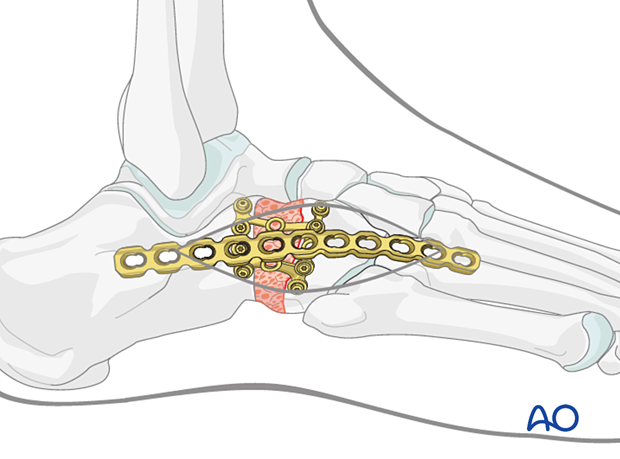
5. Temporary bridging of the reconstruction
A bridge plate or an external fixator may be used to supplement the cuboid reconstruction.
Bridging may be achieved using either an external fixator or a reconstruction plate until the cuboid has healed.
Such a plate or distractor must be removed subsequently to permit restoration of some joint motion.
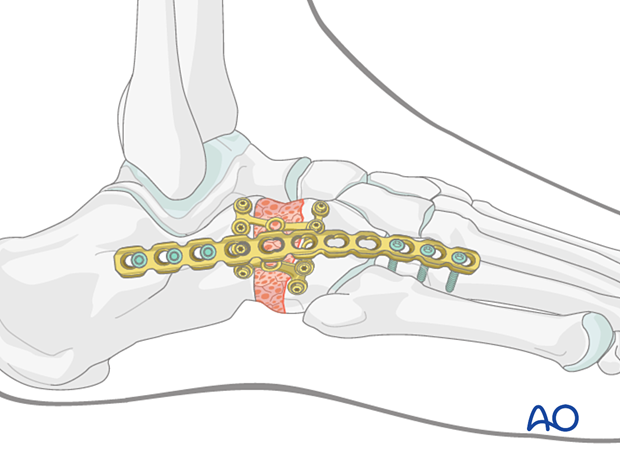
Temporary bridging using a reconstruction plate
Plating can be performed through the dorsolateral incision aligned with the fourth metatarsal. Soft-tissue stripping should be avoided if possible.
The plate length should allow for fixation using a minimum of three screws both proximally and distally.
The plate needs to be contoured to achieve a good fit and prevent tenting of the skin.
- In-plane bending to adapt to the arch of the lateral foot
- Out of plane bending to adapt to the lateral contour of the lateral column
- Torquing to fit both the vertical wall of the calcaneus proximally and the dorsal aspect of the fourth metatarsal distally
The step-by-step bending procedure is analog to the bending of reconstruction plates.
The plate may be pre-contoured using a saw-bone foot model and fine-tuned in situ as an alternative to using a template.
Fix the bridge plate, using a minimum of three screws both proximally (calcaneum) and distally (fourth metatarsal).
Temporary bridging using an external fixator
Instead of bridge plating, the lateral column distractor can be replaced with an external fixation construct, which can be left in place while the bone heals.
Two bicortical pins are inserted in both the calcaneum and the 5th metatarsal.
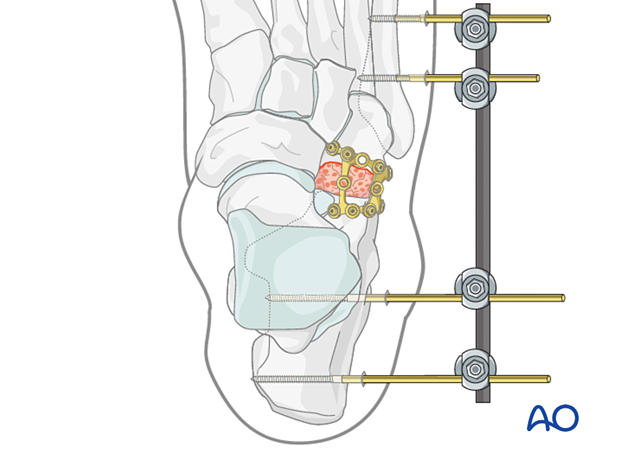
Supplemental fixation (screw or K-wire) can be placed from the fifth metatarsal (which can be rendered unstable by this injury) through the fourth metatarsal into the third metatarsal, or lateral cuneiform; which will further prevent lateral column shortening.
6. Aftercare
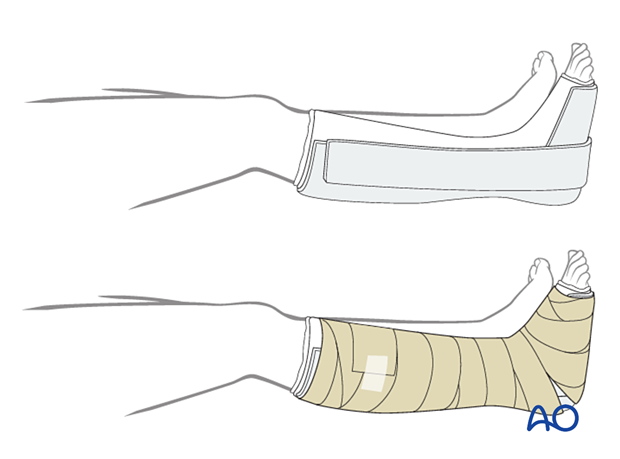
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
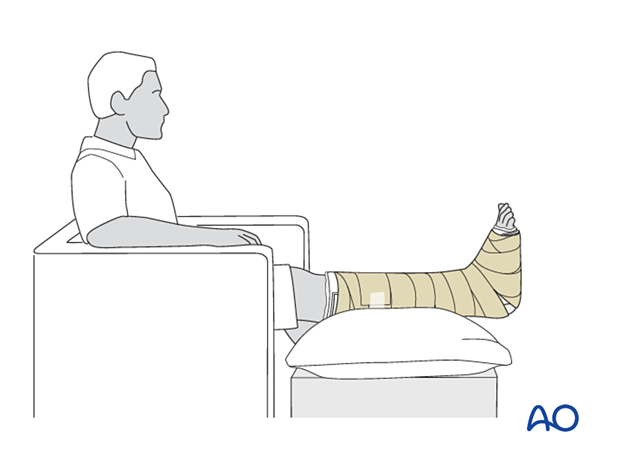
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













