ORIF - Plating
1. Principles
Order of fixation
Normally, the less challenging of the two bones (the segmental injury) will be approached first and preliminary fixation undertaken, unless the condition of the soft tissues determines otherwise.
Most often, fixation of these fractures proceeds as follows:
- Reduction and preliminary fixation usually starts with the segmental fracture
- Reduction and definitive bridge fixation of the multifragmentary fracture of the other bone
- Definitive fixation of the segmental fracture
Never commit yourself to the definitive fixation of one bone until you have assured yourself that you can reduce the other bone.
Throughout this module, the fixation of each bone will be described to completion, but the surgeon is reminded not to complete the first fixation until the second bone has been definitively fixed.
Note on approaches
When both bones need to be reduced and fixed, a separate approach to each bone should be performed to reduce the risk of heterotopic bone formation.
For proximal radial shaft fractures, the anterior approach (Henry) is most often used to minimize the risk of damage to the posterior interosseous nerve, which crosses the proximal radius within the supinator muscle.
In mid and distal radial shaft fractures, either the anterior approach (Henry) or posterolateral approach (Thompson) can be used, depending on surgeon’s preference.
The ulna is exposed by the standard subcutaneous approach between the flexor and extensor muscle compartments.
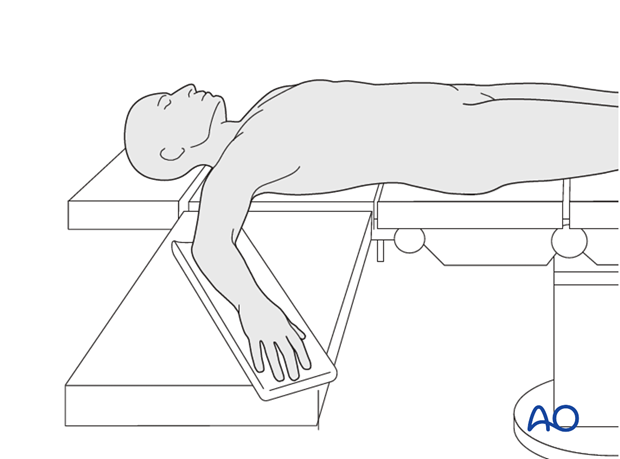
2. Patient preparation
This procedure is normally performed with the patient in a supine position.
3. Detailed procedures
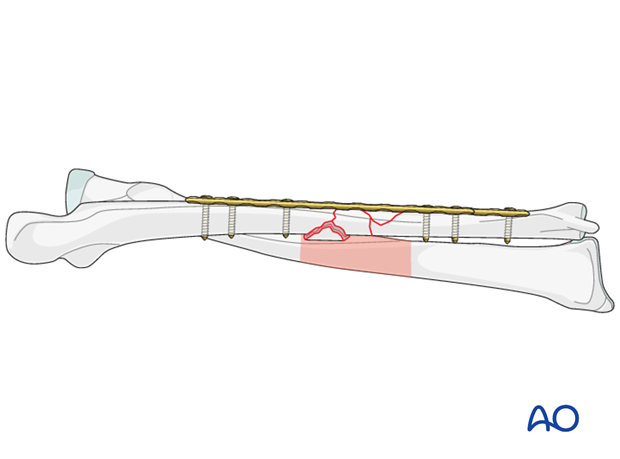
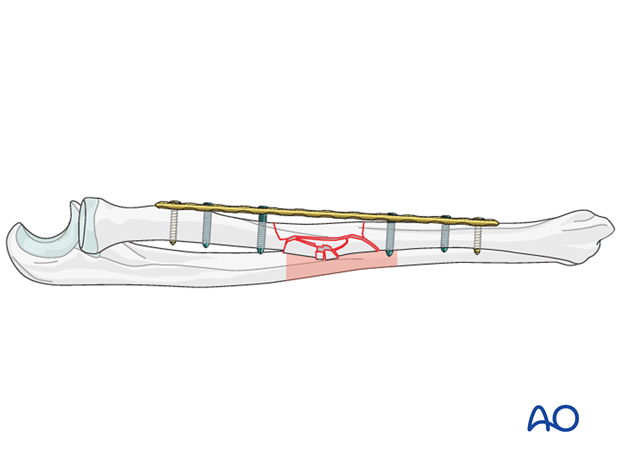
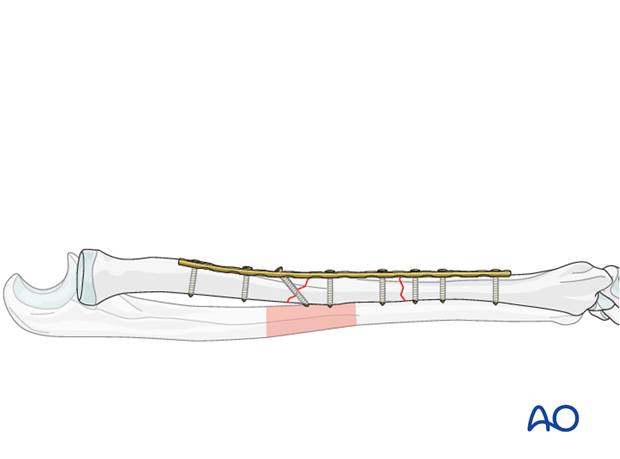
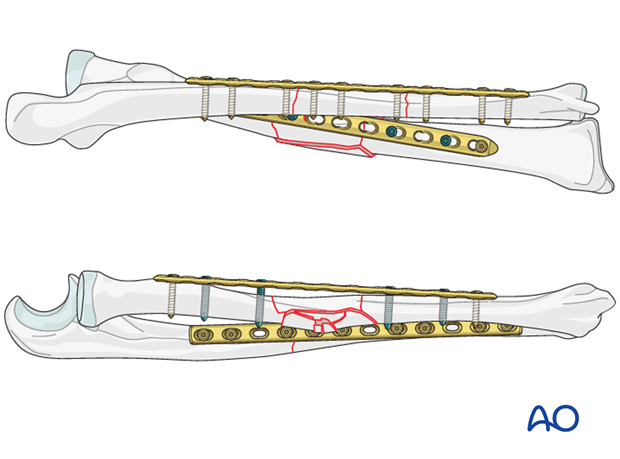
In fractures where either the radius or the ulna has an intact segmental fracture pattern, whereas the other bone has a complex multifragmentary fracture, at either of the two fracture sites of the segmental injury, the fracture morphology may be either oblique or transverse (short oblique). Possible techniques are:
Note: one long (as illustrated) or two short plates can be used (see detailed technique).

Note: one long (as illustrated) or two short plates can be used (see detailed technique).
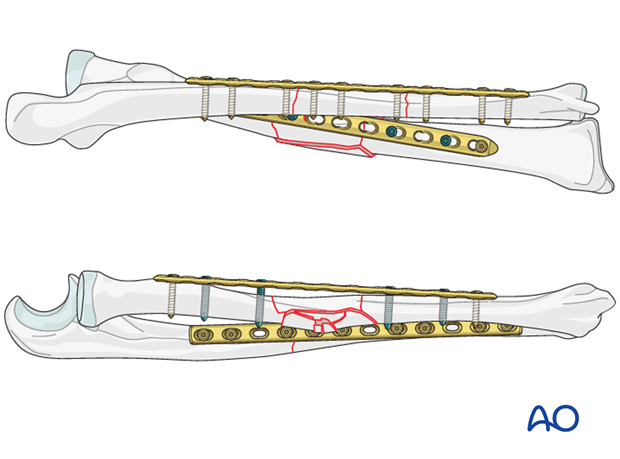
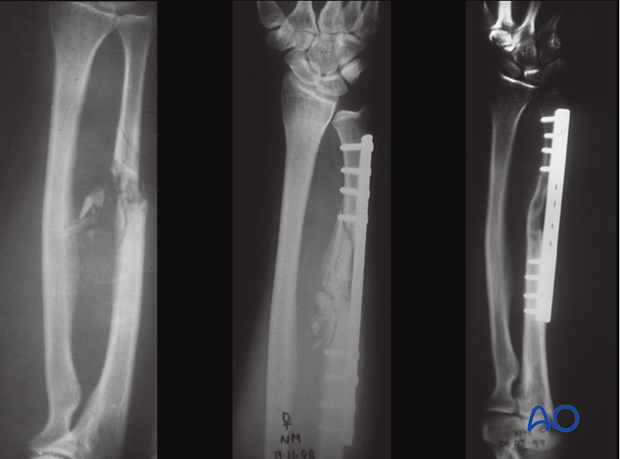
4. Completed osteosynthesis
This illustration shows an example of a completed osteosynthesis.
5. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
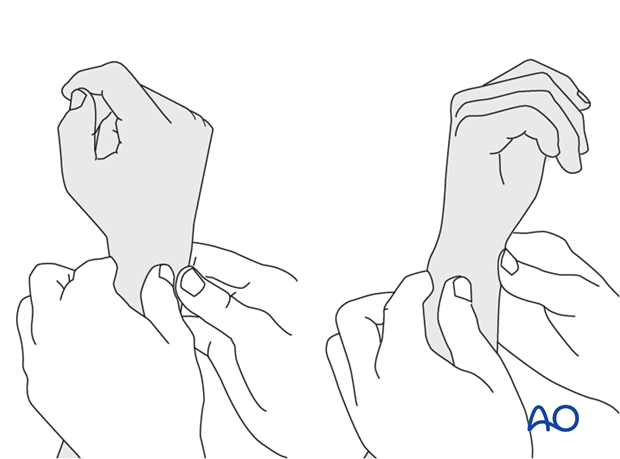
The elbow should be stabilized at the epicondyles and the forearm rotation should be checked between the radial and ulnar styloids.
6. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
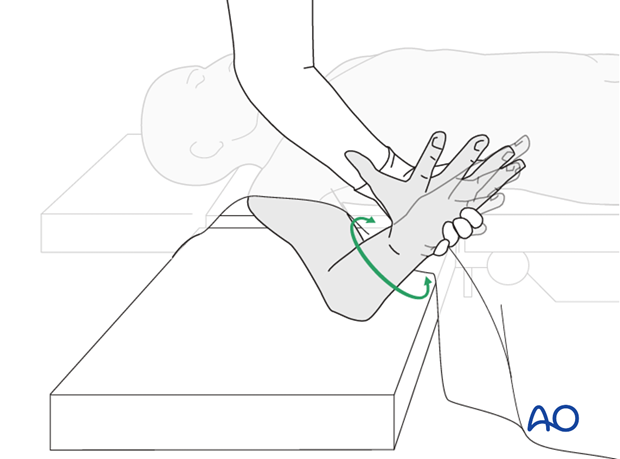
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
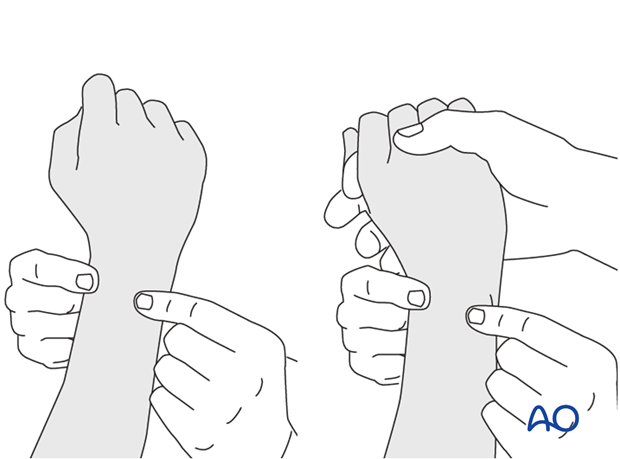
This is repeated with the wrist in full supination and full pronation.
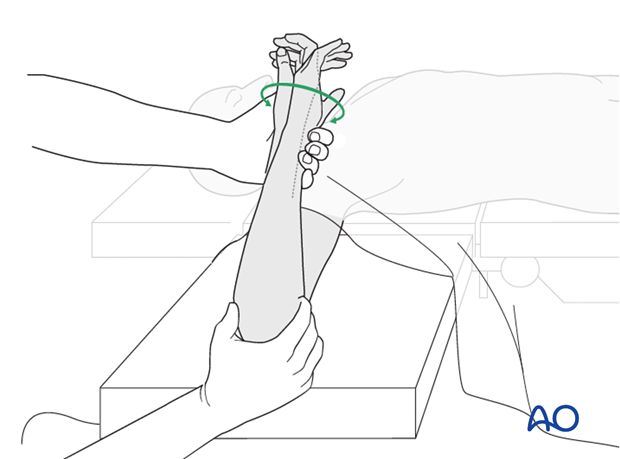
Method 2
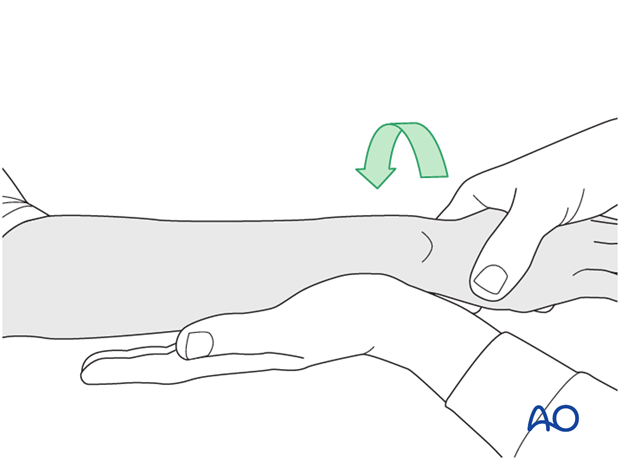
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
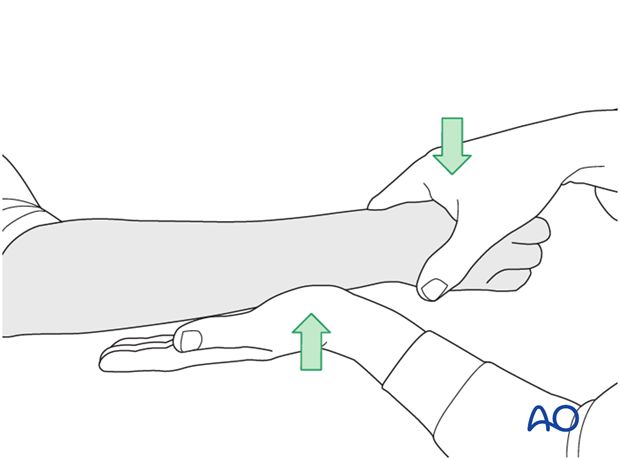
...while the forearm is passively put through full supination...
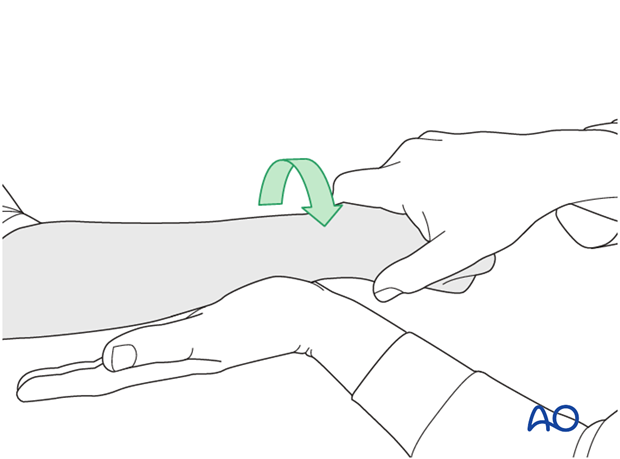
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
7. Postoperative treatment
Functional aftercare
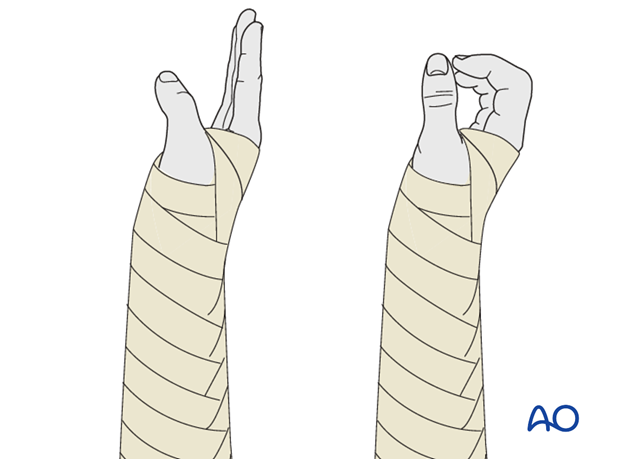
Following stable fixation, postoperative treatment is usually functional.
Immobilization in a circular cast may compromise the range of motion later. However, since soft-tissue swelling, and edema are associated with these high-energy fractures, a temporary immobilization with a well-padded, bulky splint for 10-14 days is advised to allow adequate soft-tissue healing. During this period, elevation, gentle finger motion, active and passive, together with elbow flexion/extension and shoulder motion, can be started. The splint is then removed and active assisted range of motion exercises, including gentle forearm rotation, begin.
Lifting and resisted exercises are restricted until radiographic signs of healing appear. More intensive exercises, such as progressive resisted exercises can start at that time. Timing of return to sport will depend on the individual patient and the nature of the sport.
Follow-up
Close postoperative follow-up is required in these fractures. In those that have been treated by means of relative stability, secondary bone healing with callus formation is anticipated and early signs of delayed union should alert the surgeon to consider secondary interventions, such as bone grafting.
Follow-up x-rays should be obtained according to local protocol. X-rays to assess fracture position are usually taken at 1, 2, and 4 weeks after operation. Subsequent x-rays are usually taken to assess bony healing at appropriate intervals from 6-8 weeks, depending on the fracture configuration and potential for healing.
Implant removal
In forearm shaft fractures, the issue of implant removal is controversial. As the radius and ulna are not weightbearing bones, and as removal of plates can be a demanding procedure, implant removal is not indicated as a routine. There is a high risk of nerve damage associated with procedures to remove forearm plates.
Furthermore, as there is significant risk of refracture, most surgeons prefer not to remove plates from the forearm.
The general guidelines today are:
- removal only in symptomatic patients, possibly only on the ulna where the implants are subcutaneous
- removal no earlier than 2 years after osteosynthesis
- If both bones have been plated, sequential removal of implants with a least 6 months in between is recommended (risk of refracture).