En bloc resection with posterior release and anterior tumor delivery (L1 to L5)
1. Introduction
En bloc resection of a primary tumor is a significant undertaking, even in the most experienced hands. We therefore recommend referring these cases to quaternary centers with experience in primary spine tumor surgery.
En bloc resections
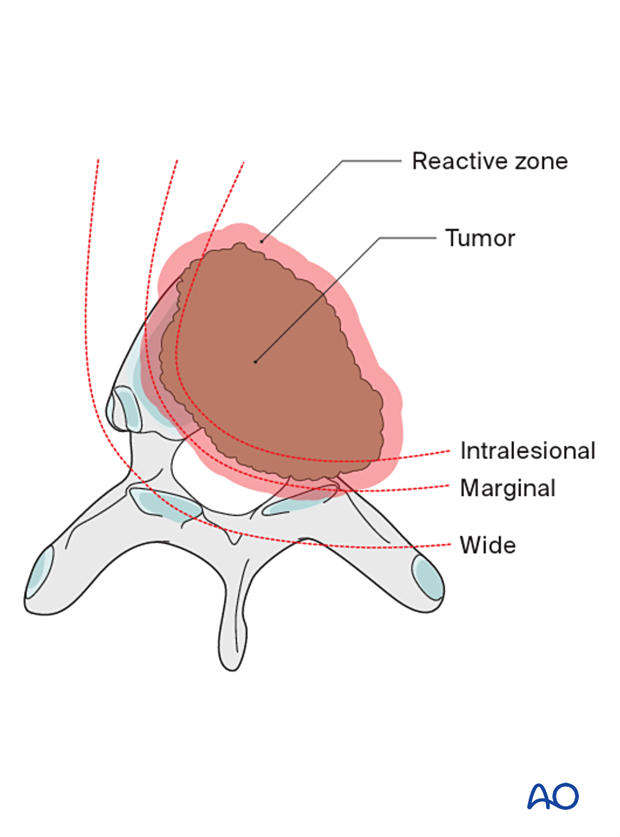
Terminology is essential in primary tumor management.
An en bloc resection refers to a surgical attempt to remove a tumor in one piece without violating it.
On the other hand, an intralesional resection or a curettage refers to a deliberate intralesional resection.
An en bloc resection needs to be associated with a pathological margin description to be correctly defined.
Four types of margins are described:
- Intralesional – resection margin is within tumoral tissue
- Marginal – resection margin is within a reactional zone or pseudocapsule (in the spine, the epidural margin is often marginal)
- Wide – resection margin is within normal tissue
- Radical – this is extracompartmental resection and, as such, does not apply to spine tumors
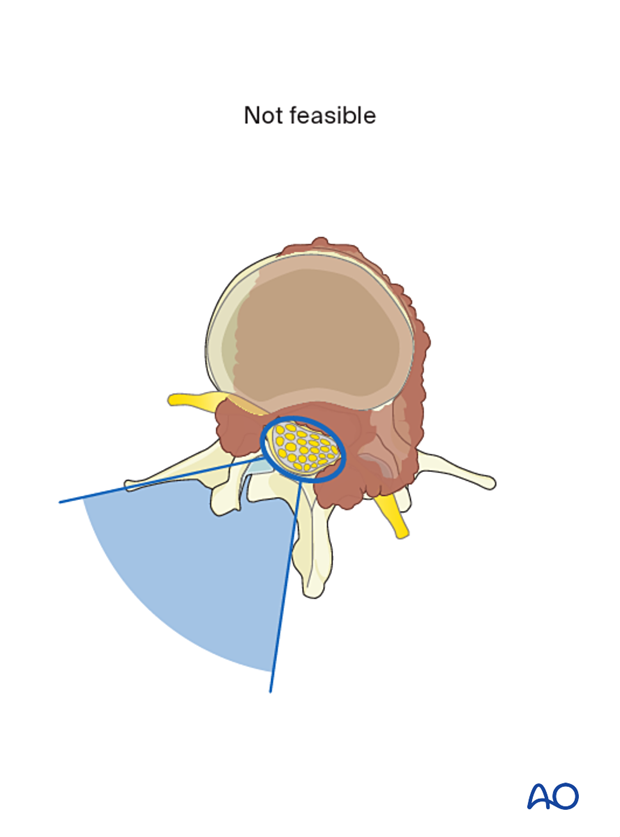
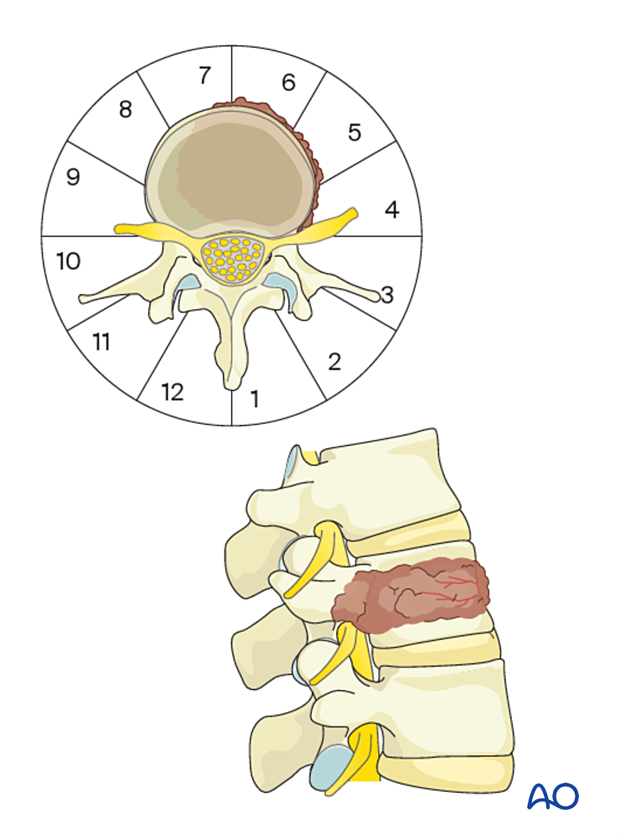
Feasibility
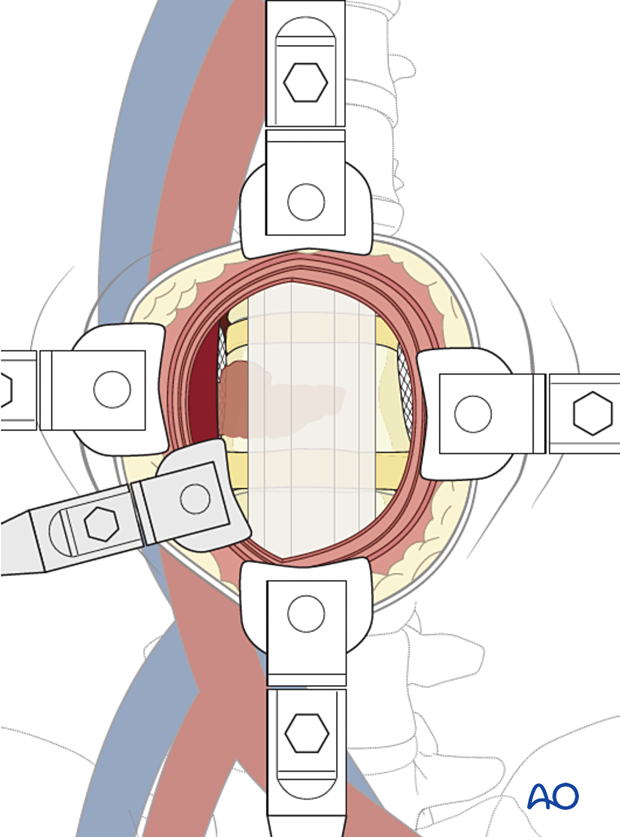
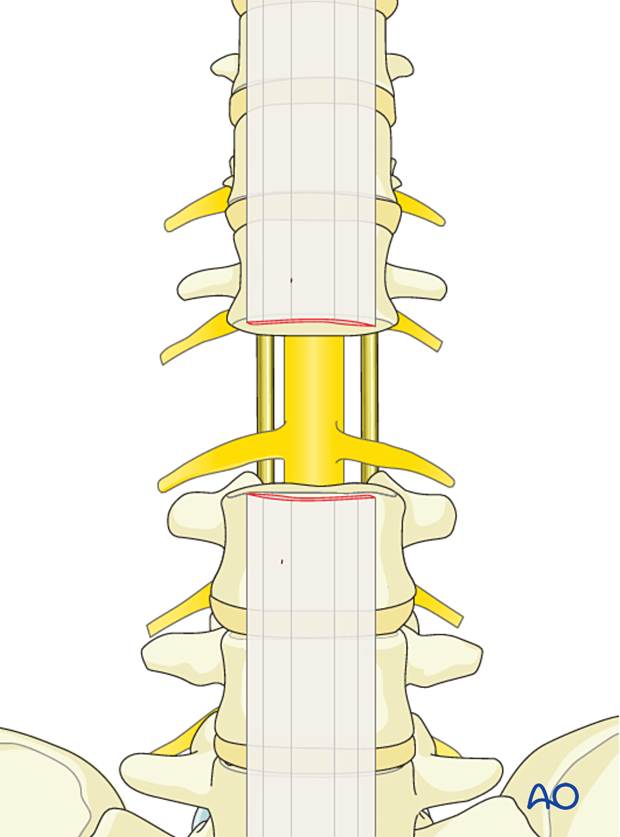
Two conditions need to be met for an en bloc resection to be deemed possible:
- If we consider the spinal canal as a ring, there needs to be enough circumference of that ring to be removed piecemeal to allow delivery of the neural element
- Access to the nerve root sleeve at its dural origin is required
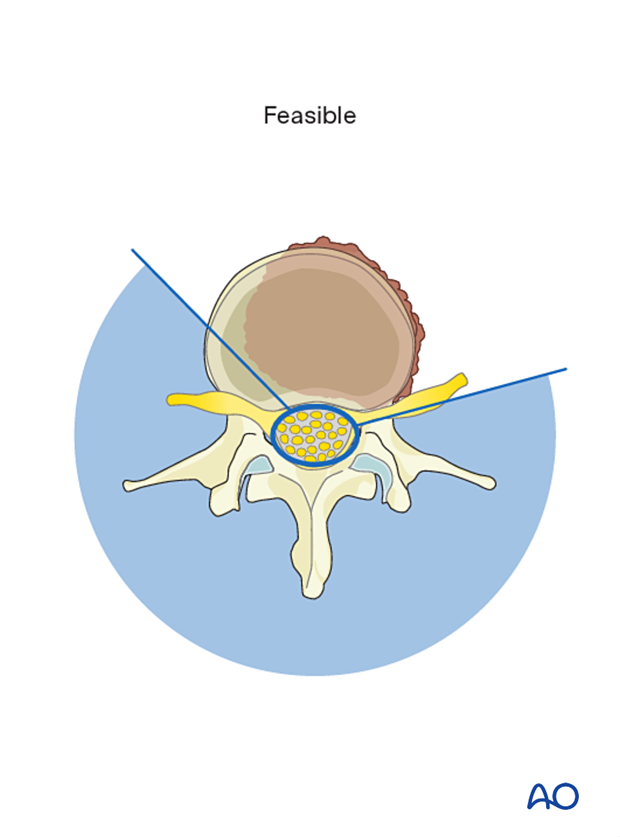
If these conditions are not met, an en bloc resection will not be possible without a planned transgression of the tumor.
In this illustration, the spinal canal is circumferentially surrounded by a tumor. There is not enough uninvolved portion of the ring to allow an en bloc resection.
2. Planning
Preoperative management
Proper planning is instrumental in the management of primary spine tumors. A multidisciplinary approach may be required depending on the localization of the tumor.
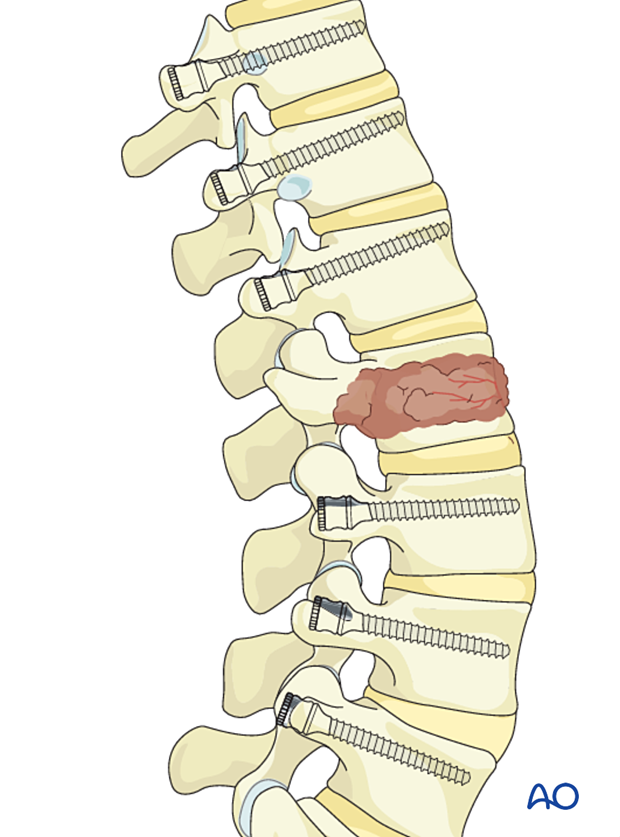
This picture shows an example of an L3 chordoma.

Embolization
Embolization procedures are recommended to reduce operative blood loss in hypervascular tumors, especially during more extensive resections.
Embolization should be considered for hypervascular tumors, such as giant cell tumors, aneurysmal bone cysts, and hemangiomas.
The role of the embolization is:
- To reduce the vascularity of the tumor
- To facilitate dissection around the tumor
- Mapping of spinal cord vascular supply
Embolization on its own may also have a therapeutic effect.
This image shows the embolization of a hypervascular tumor.

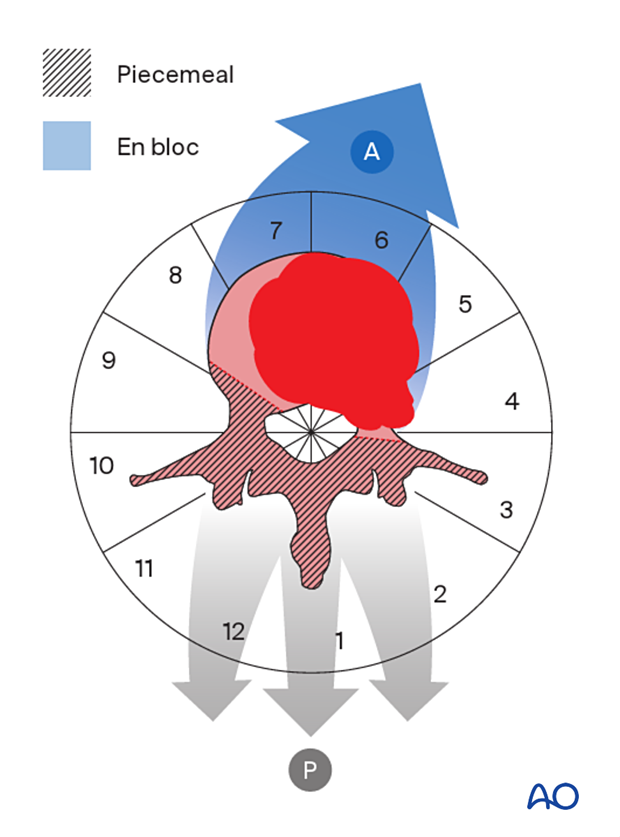
Resection strategy
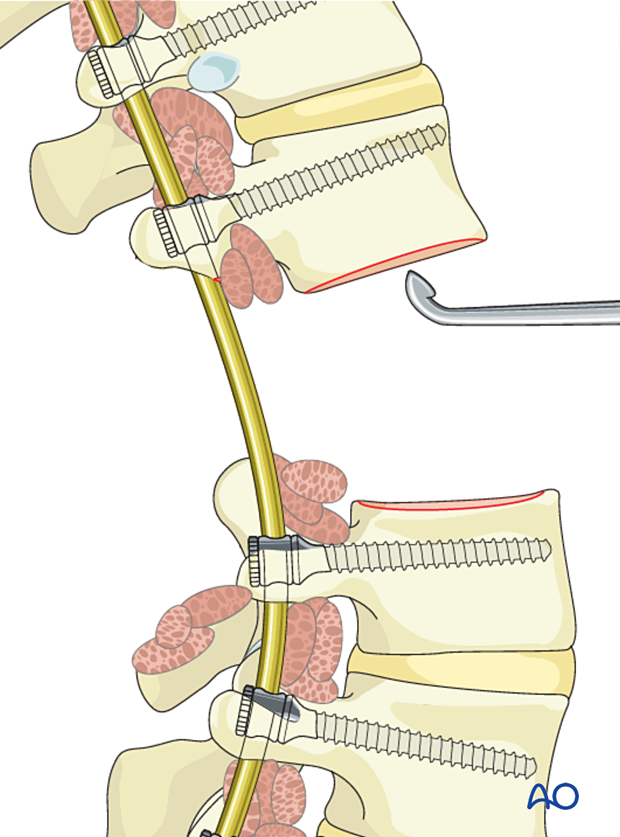
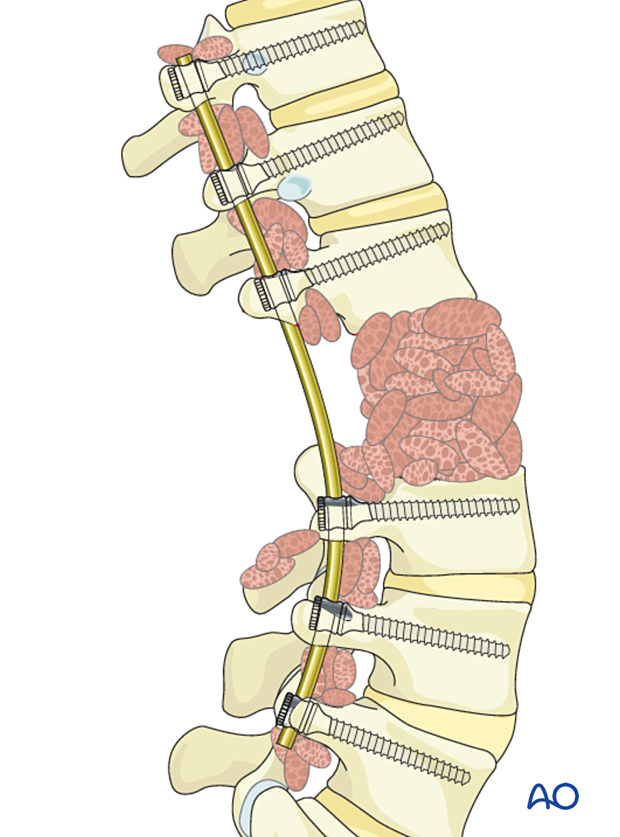
A posterior tumor release followed by anterior delivery is generally recommended for a lumbar tumor involving the vertebral body.
During the posterior approach, the uninvolved part of the spinal ring will be resected in a piecemeal fashion, and osteotomies and soft tissue dissections will be performed.
A wide visualization is essential in these cases, and a laminectomy involving half a level above and below the tumor is recommended.
The goal is to achieve:
- Good visualization of normal and abnormal anatomy
- Safe decompression of the neural elements
Appropriate posterior tumor mobilization allows the tumor to be delivered during the anterior approach.
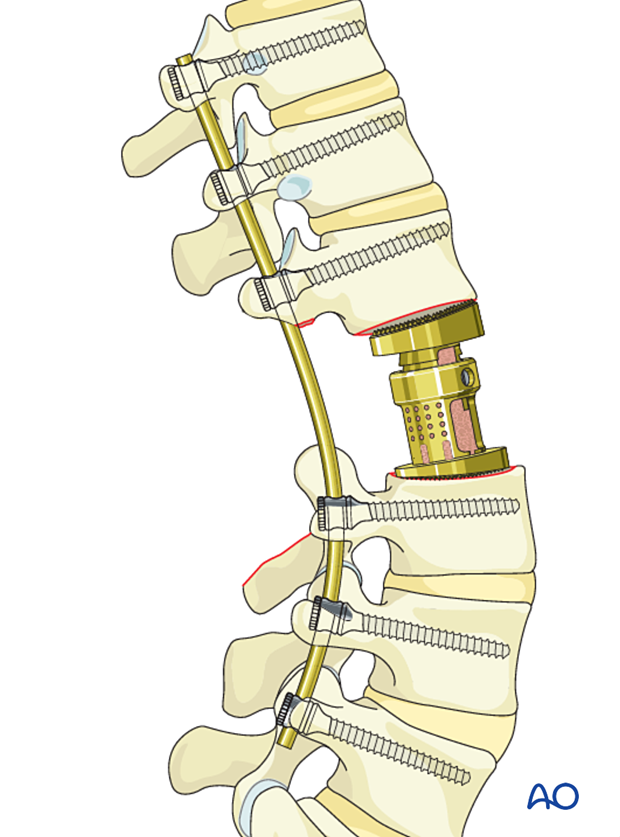
Reconstruction strategy
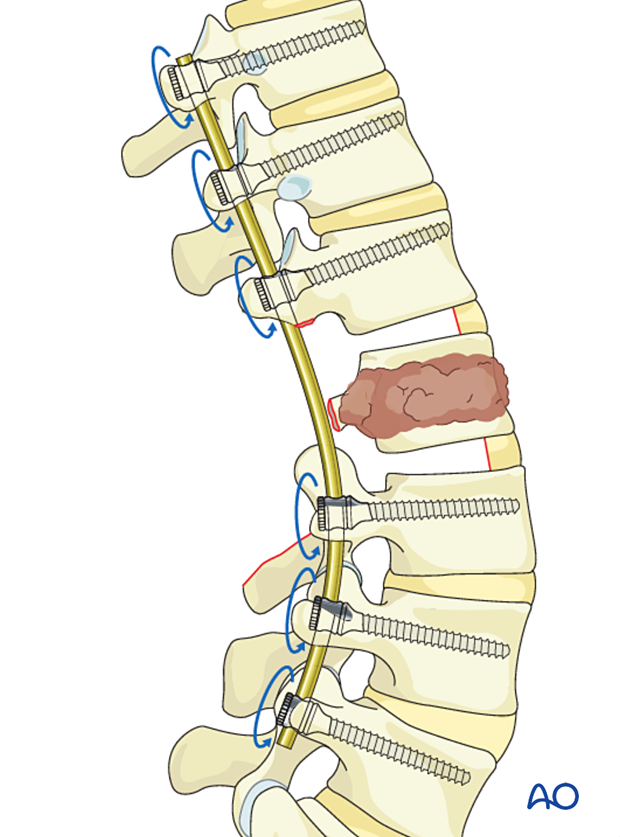
En bloc resection is a destabilizing procedure. As such, long constructs are required.
Generally, two to three vertebrae above and below the tumor are included in the construct. In multilevel tumors, or when there is poor bone quality, this construct can be extended.
The risk of implant failure may be decreased by using cemented fenestrated screws in patients with poor bone quality. Alternatively, other techniques like hooks or sublaminar wires can be used.
As the procedure is often curative, it is important to verify that the spine is reconstructed in good alignment, and a solid bony union should be attempted.
Case-based scenario
Every case is unique.
To illustrate the surgical principle of an en bloc resection with posterior release and anterior delivery in the lumbar spine, we will use an L2 tumor located in segments 4–8 of the WBB classification.
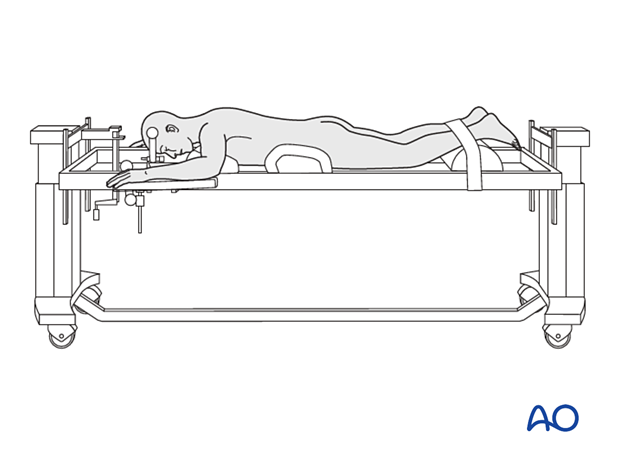
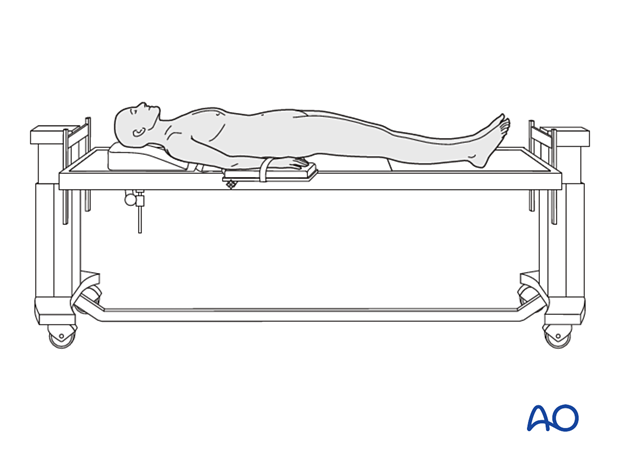
3. Patient preparation and surgical access for posterior release
Patient preparation
The patient is placed prone.
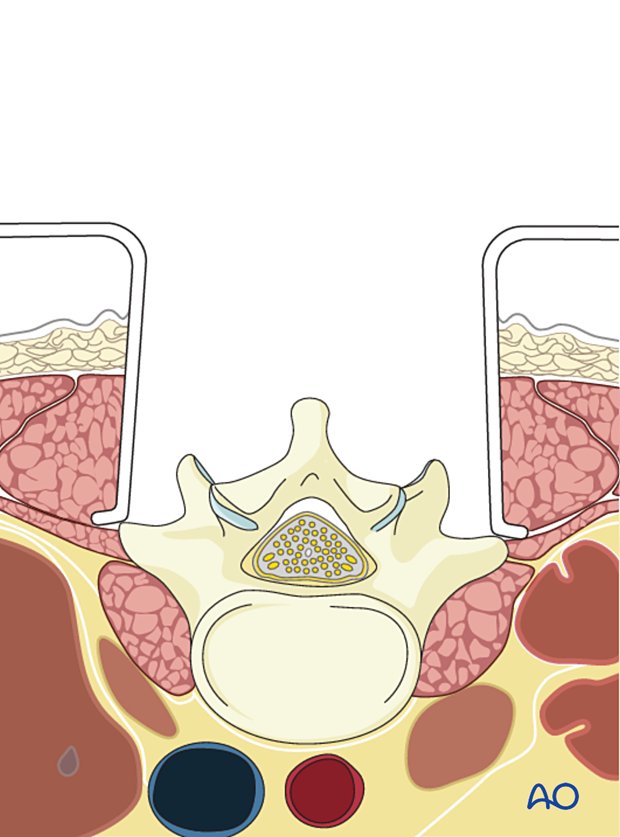
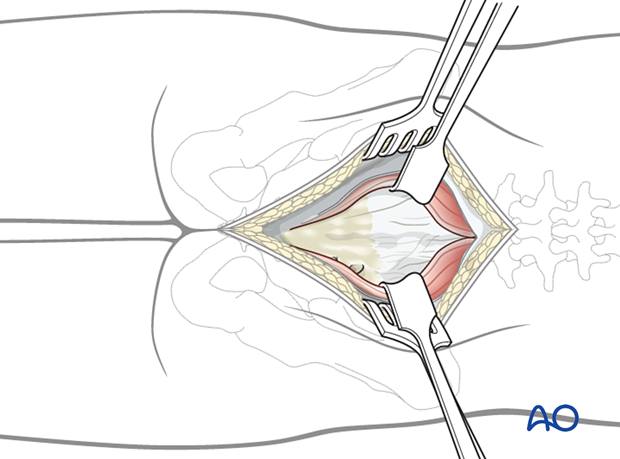
Surgical access
A posterior midline approach to the lumbar spine is performed.
A wider dissection will typically be performed for primary tumors compared to a trauma case.
Great care should be taken not to enter the tumor during exposure.
Review preoperative images to verify whether the tumor invades the lamina. In such cases, exposure of the posterior elements should be performed with great care, and the use of Cobb elevators should be avoided.
The incision may need a caudal extension when the tumor involves the lower lumbar spine.
4. Instrumentation
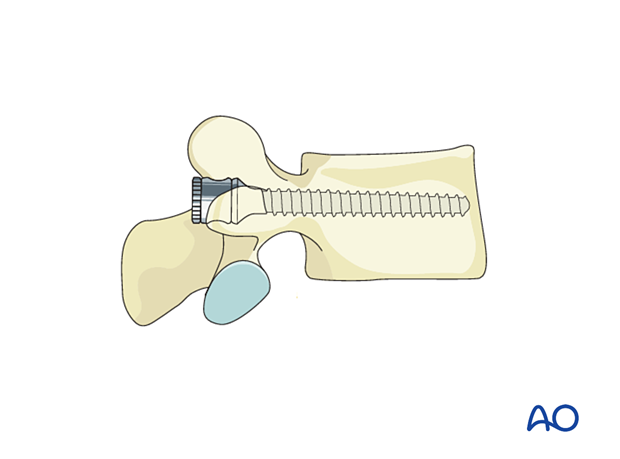
Screw insertion
Insert all screws according to the preoperative plan.
Optimal pedicle screw purchase will, in order of importance, be achieved by:
- Selecting the largest possible screw diameter according to the pedicle diameter
- Selecting the longest possible screw
- Positioning of the screw under the cranial endplate
- Cement augmentation of the screw
Lumbar pedicle screws are inserted according to the standard technique.
Rod preparation
Every effort should be made to contour the rod to decrease the risk of induced sagittal or coronal malalignment.
For further details about sagittal spinal alignment refer to this page.
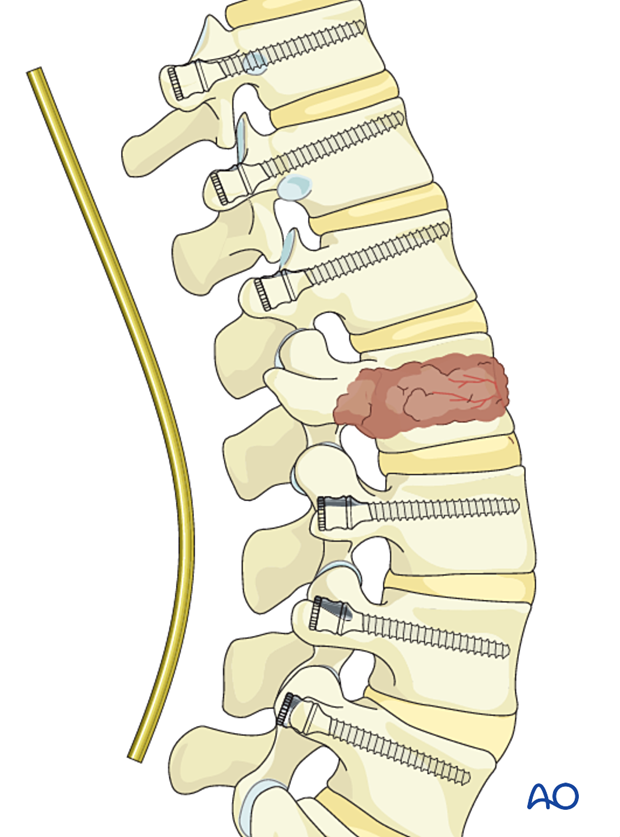
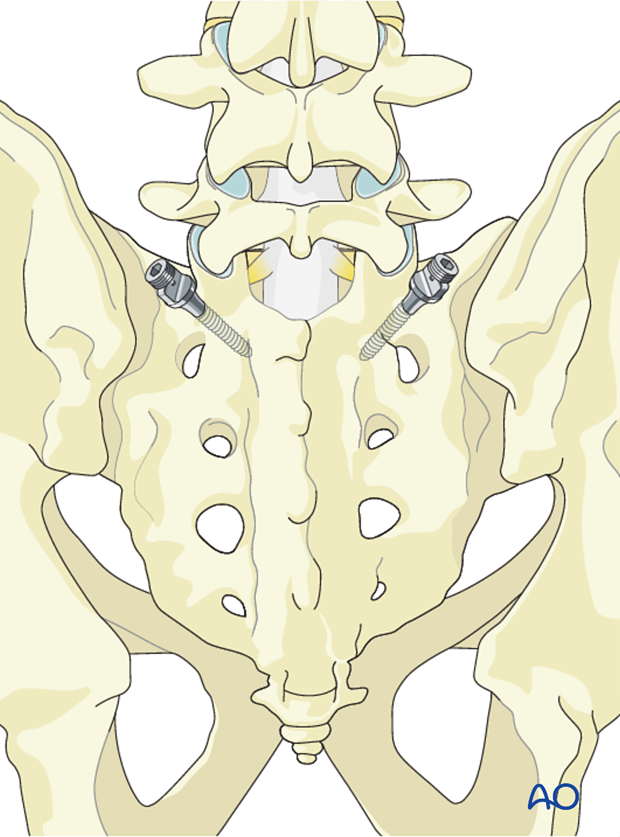
Sacral and iliac instrumentation
When the tumor involves the lower lumbar spine, extending instrumentation to S1 and the iliac may be necessary.
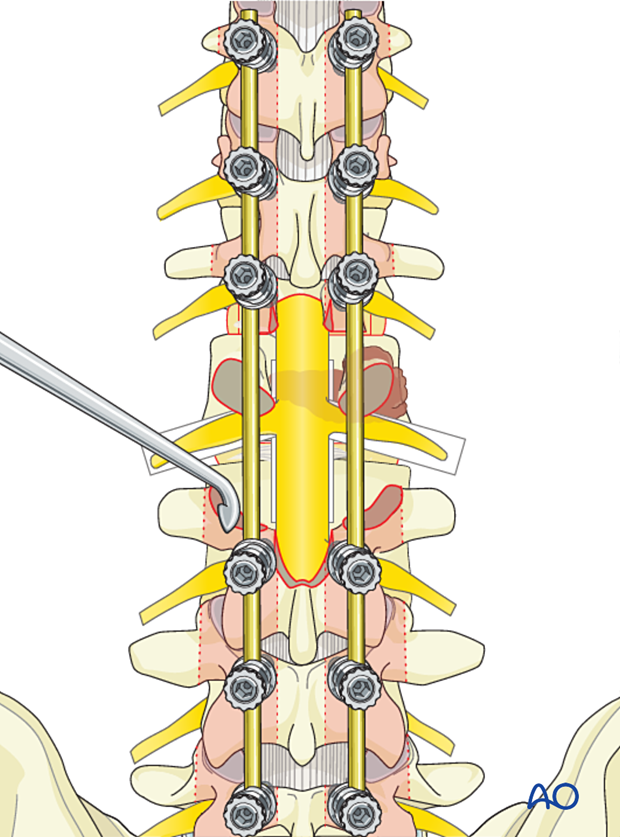
5. Posterior release
Laminectomy
Perform a laminectomy according to the preoperative plan.
Dissection should progress from normal to abnormal tissues to protect normal neurological elements and facilitate dissection.
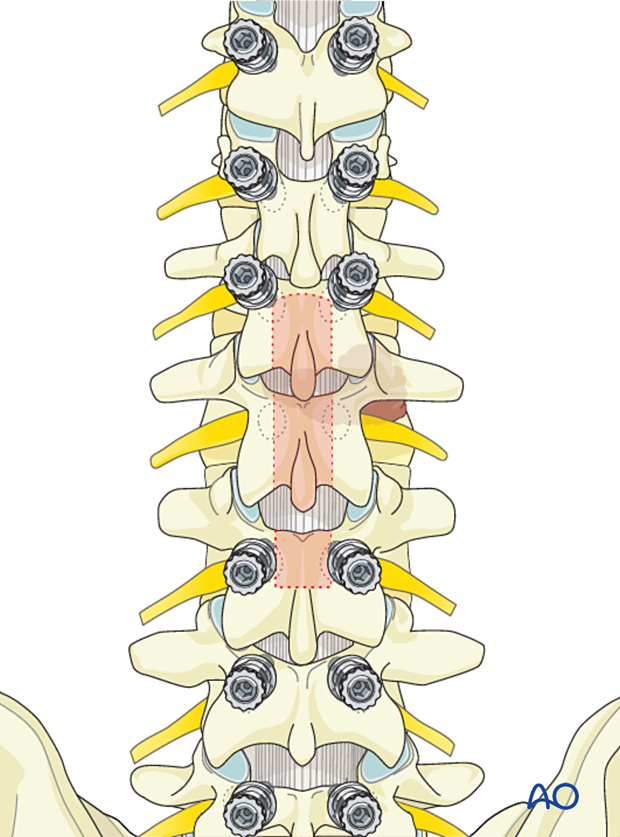
Bony release
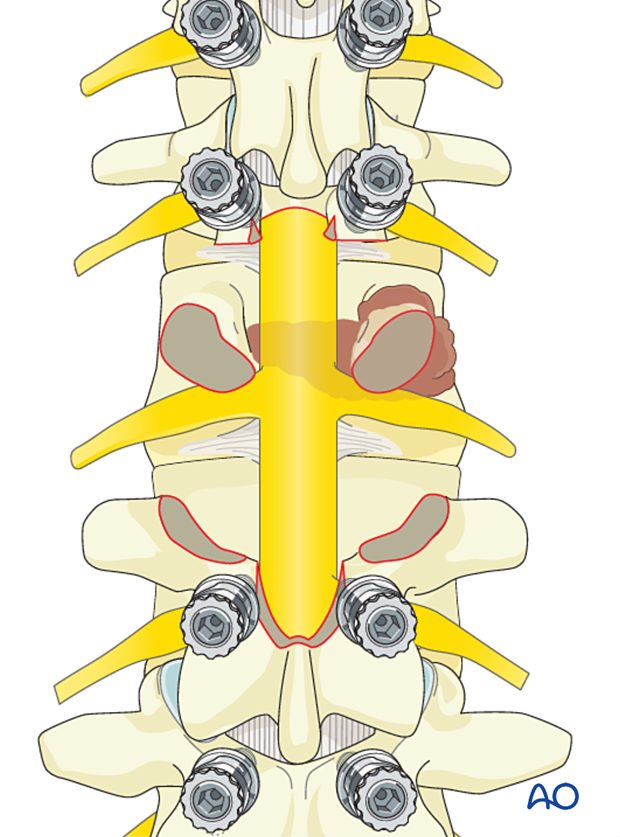
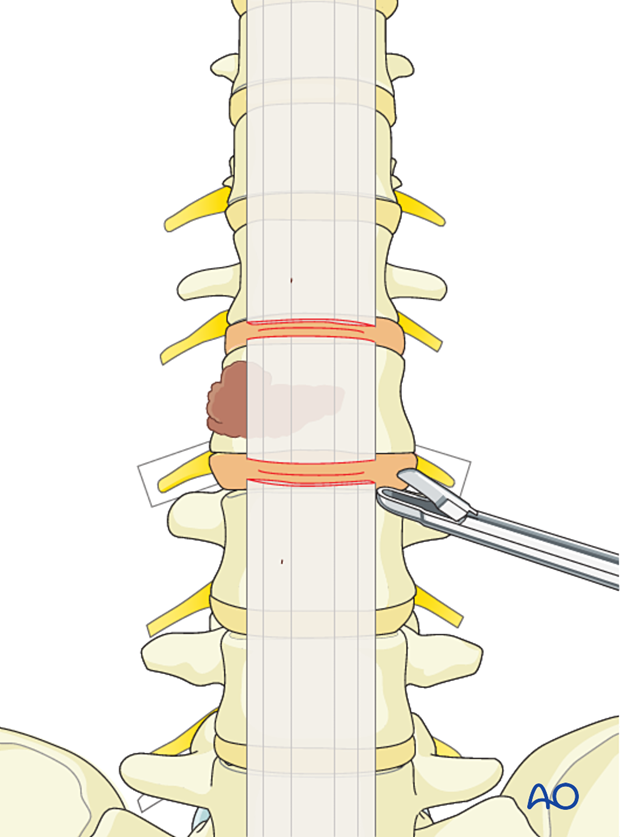
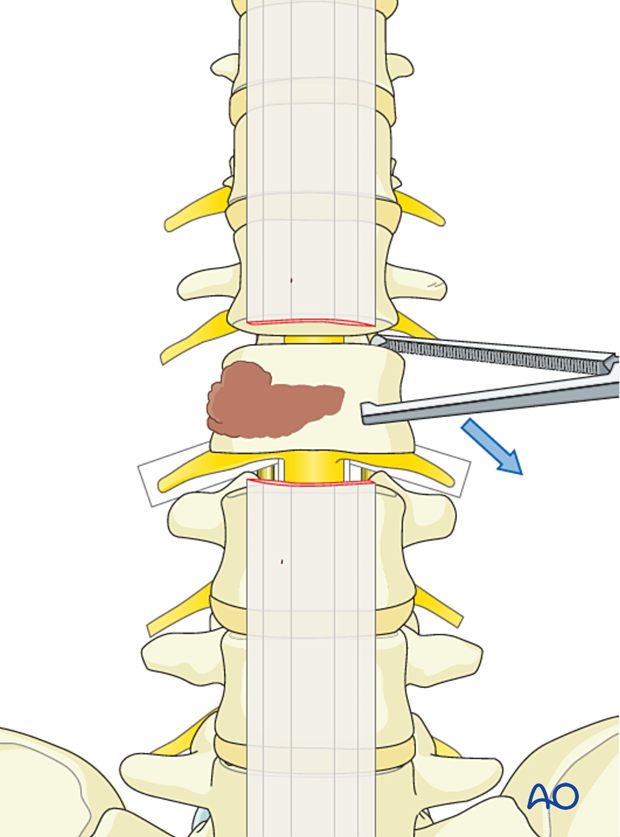
Perform an osteotomy of the inferior facet of L1 and L2 to isolate the pedicles of L2.
Perform an osteotomy of the superior facets of L2 and L3 to visualize the disc spaces.
If uninvolved with the tumor, resect the transverse processes of L2 (highlighted in red) and the uninvolved L2 pedicle.
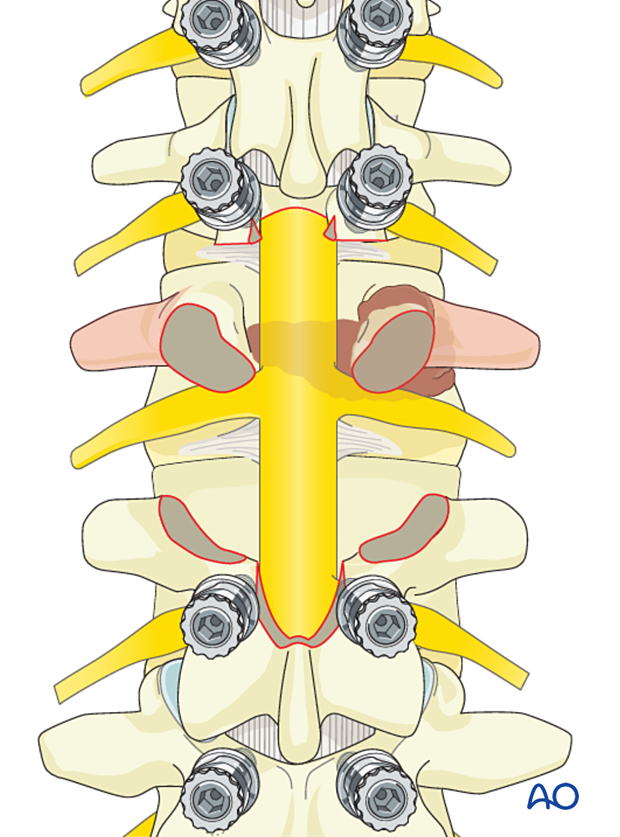
The L2 nerve roots are isolated and dissected laterally.
Every effort should be made to protect and preserve lumbar nerve roots if they are uninvolved with the tumor.
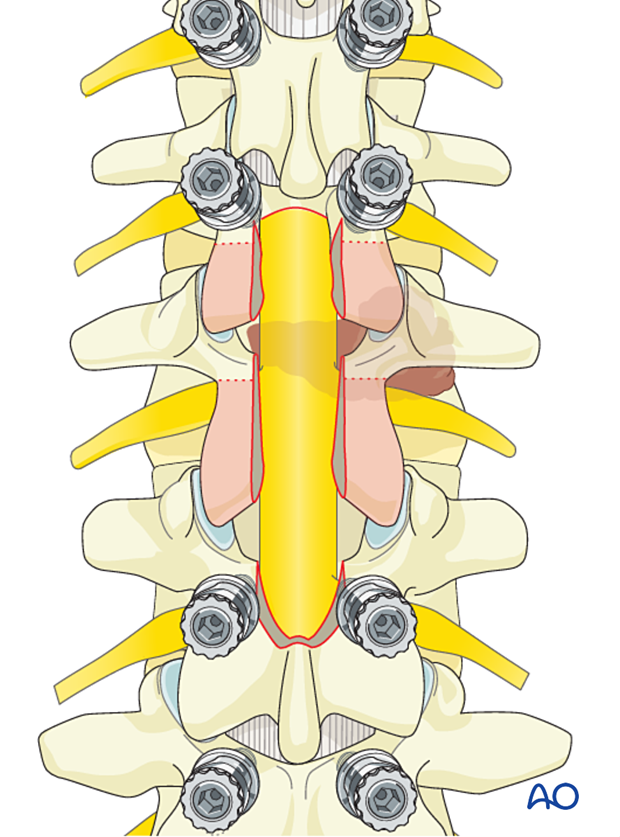
Soft-tissue release
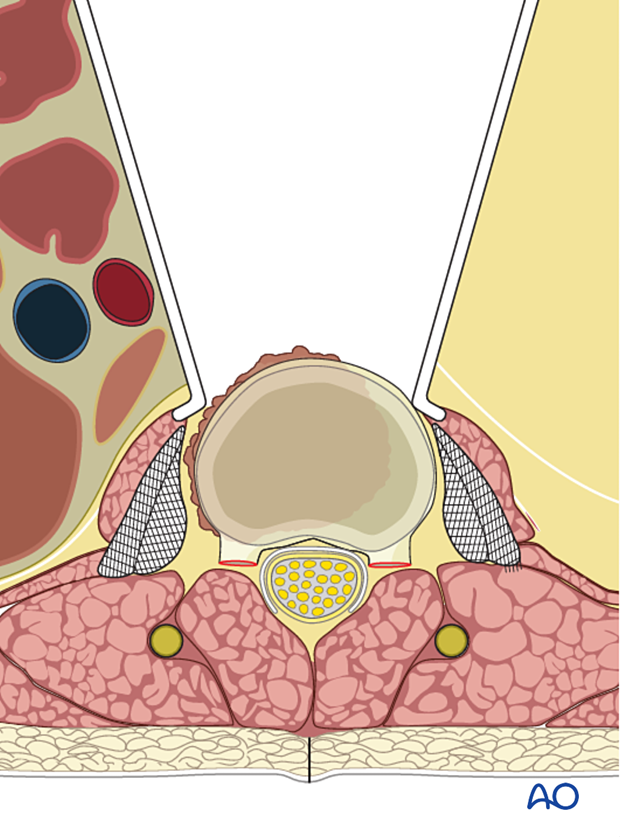
Identify the L1/L2 and the L2/L3 discs and perform an epidural dissection outside the tumor pseudocapsule.
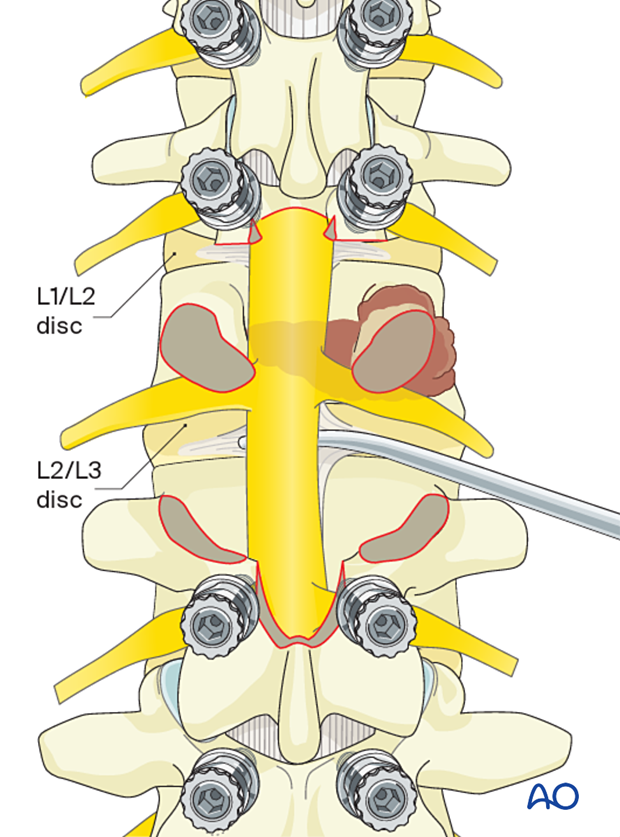
Transect the PLL at the L1/L2 and the L2/L3 disc levels.
The transected PLL will be delivered together with the tumor through the anterior approach.
Perform a discectomy of the L1/L2 and the L2/L3 discs.
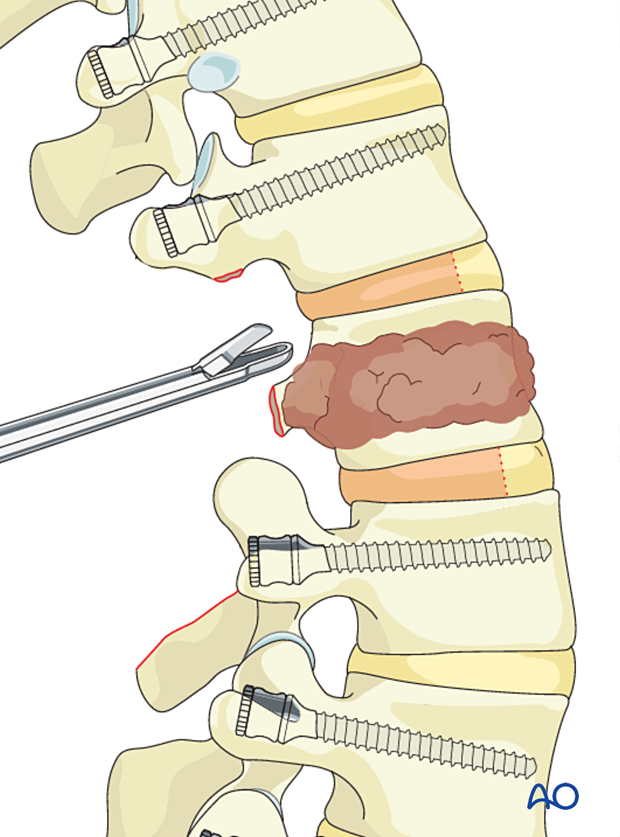
Develop a plane between the vertebra body and the psoas as anteriorly as possible.
The posterior part of the tumor release is now completed.
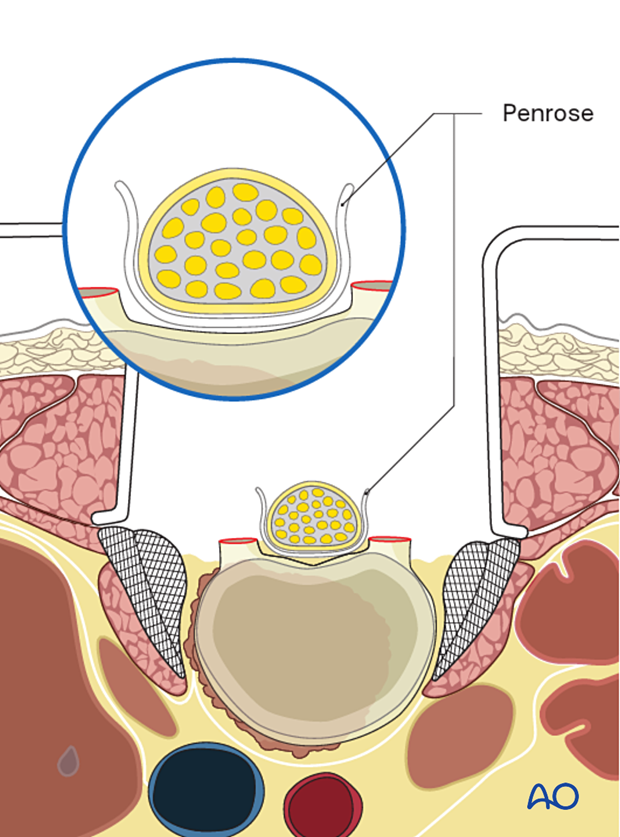
To facilitate anterior dissection, gauze paddies may be left in the dissected plane.
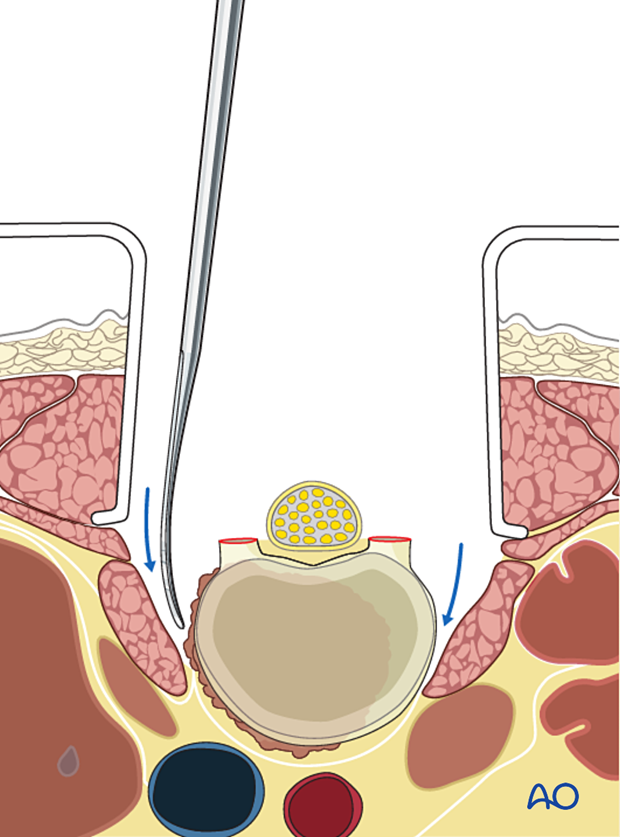
Similarly, a Penrose is left in the anterior epidural space.
Rod insertion and fixation
Insert the rods into the screw heads and secure them by tightening the inner nuts.
6. Fusion
Preparation for fusion
Excise the facet capsule and denude/curette the joint surface cartilage surfaces and the posterior cortex.
Grafting
Insert pieces of bone graft (autograft, allograft) into the decorticated facet joint for fusion.
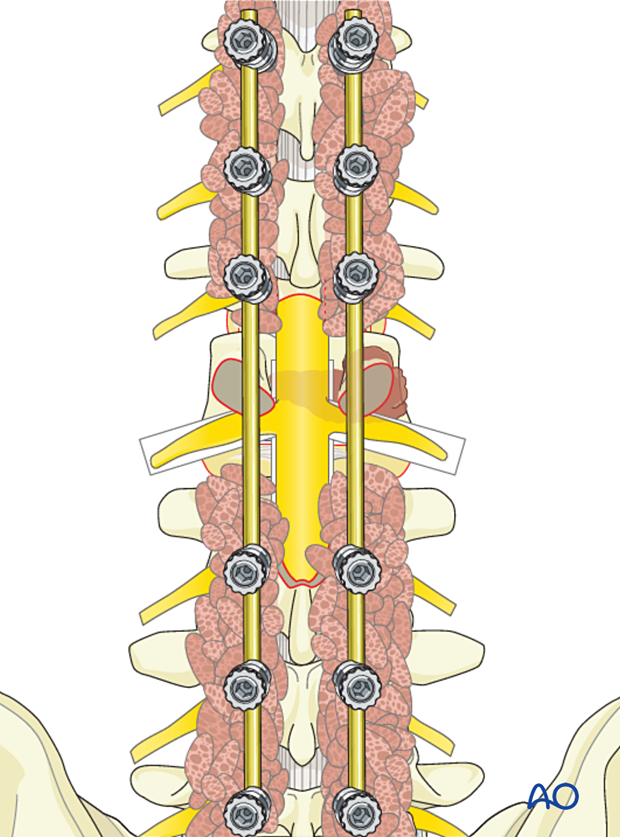
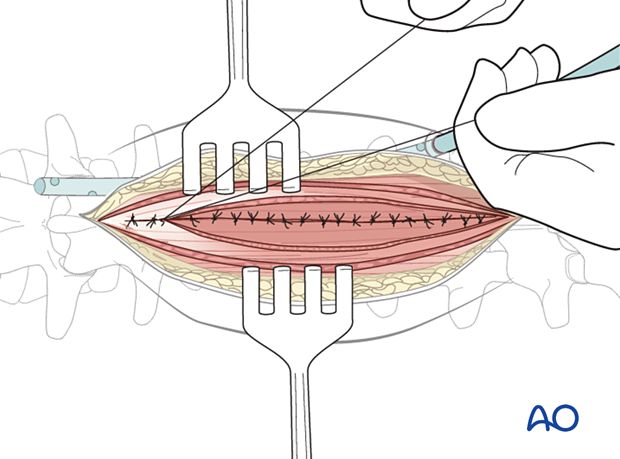
7. Posterior closure
Perform a multilayer closure as described in the approach.
For patients undergoing tumor surgery and/or with a history of radiation:
- Plastic surgery should perform soft-tissue reconstruction to decrease the risk of wound complications.
- Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications.
8. Patient preparation and surgical access for anterior delivery
Patient positioning
The patient is turned and placed in a supine position.
Surgical approach
An access surgeon is required to perform the anterior retroperitoneal approach. A lateral approach is favored for higher lumbar tumors.
This approach is, in principle, an extended version of the mini open approach.
The access surgeon mobilizes the vascular structures away from the spine and the tumor.
Great care should be taken not to enter the tumor during exposure.
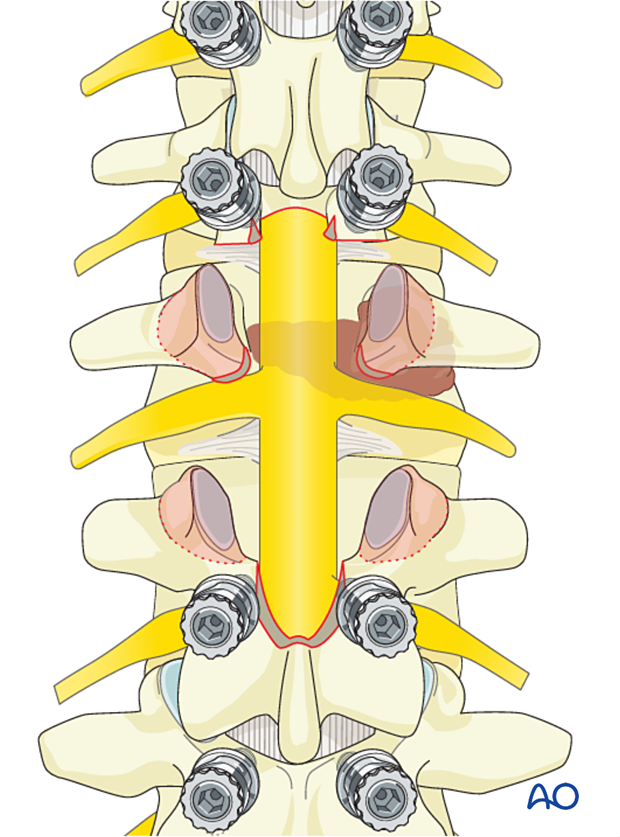
9. Tumor delivery
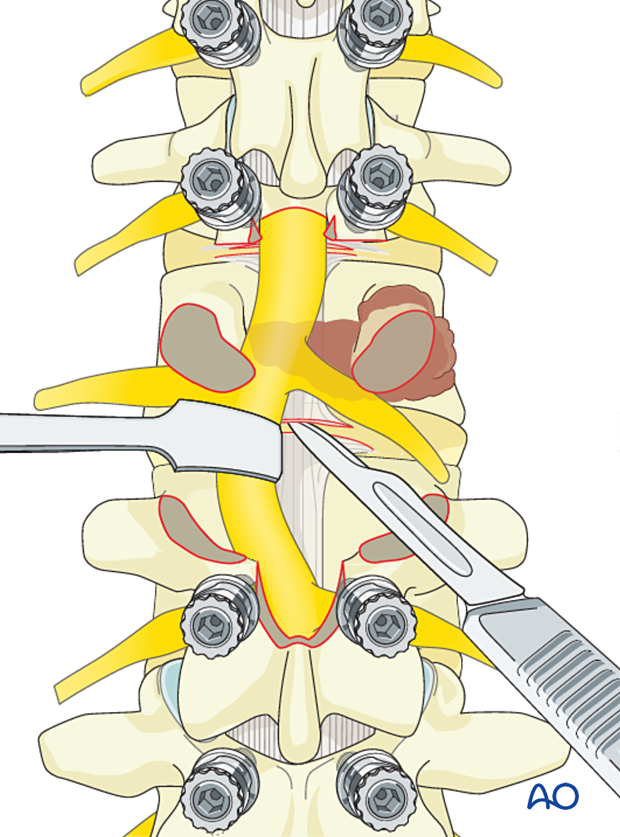
Develop the dissection plane between the vertebral body and the psoas. Dissect posteriorly until the dissection plane developed from posterior is encountered.
Transect the ALL at the L1/L2 and L2/L3 levels.

Complete the anterior portion of the L1/L2 and L2/L3 discectomy using a series of Kerrison rongeurs and curettes.
Once all soft tissue is released, the tumor is delivered.
The Penrose and the sponges left during the posterior approach are removed.
10. Anterior reconstruction
Preparation of endplates
Remove any remaining disc fragments and prepare the endplates using curettes and a rongeur.
Cage insertion
Use calipers and implant templates to measure the height of the defect.
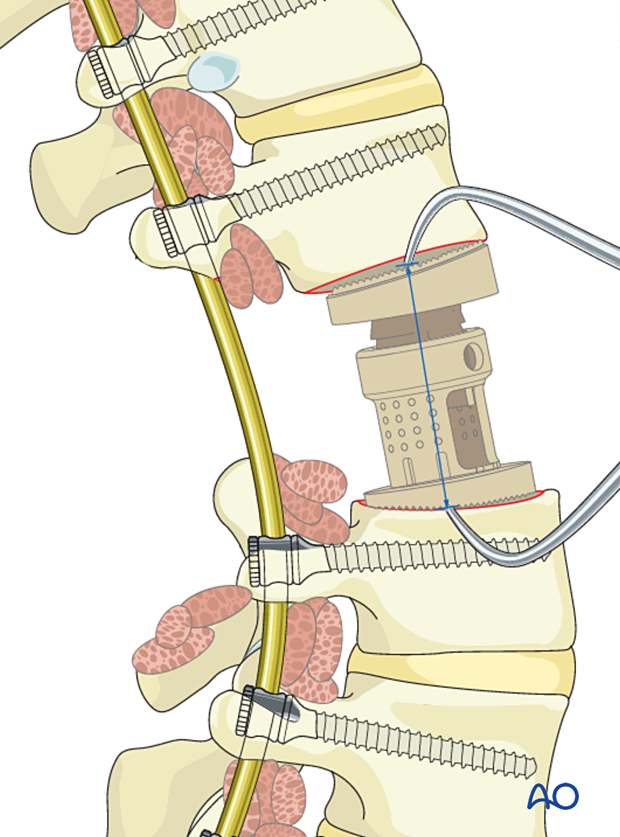
Insert an expandable prosthesis and expand it until the appropriate spinal alignment has been achieved.
Great care must be taken not to over-distract the cage.
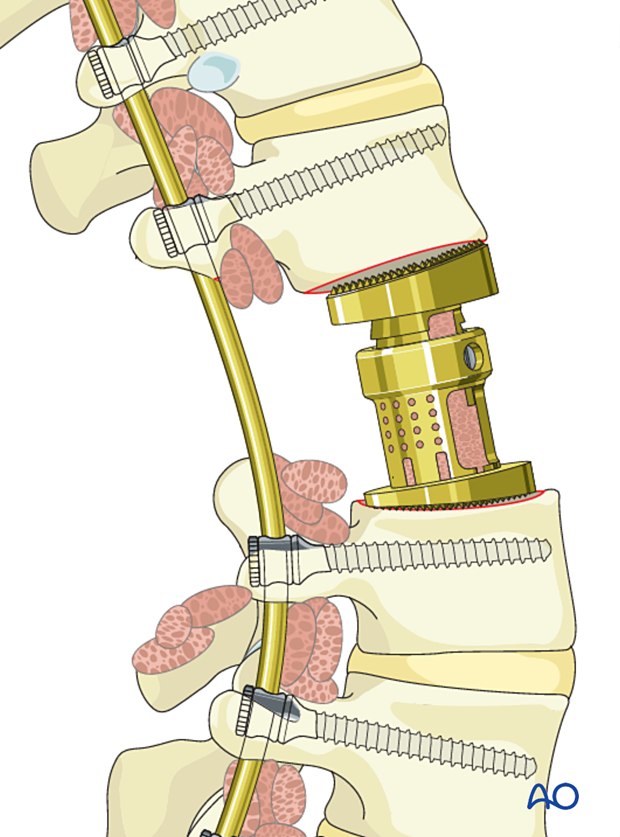
Bone grafting
Additional bone grafting can be used from the removed rib or allograft. Every effort should be made to achieve a solid bony fusion in this patient population.
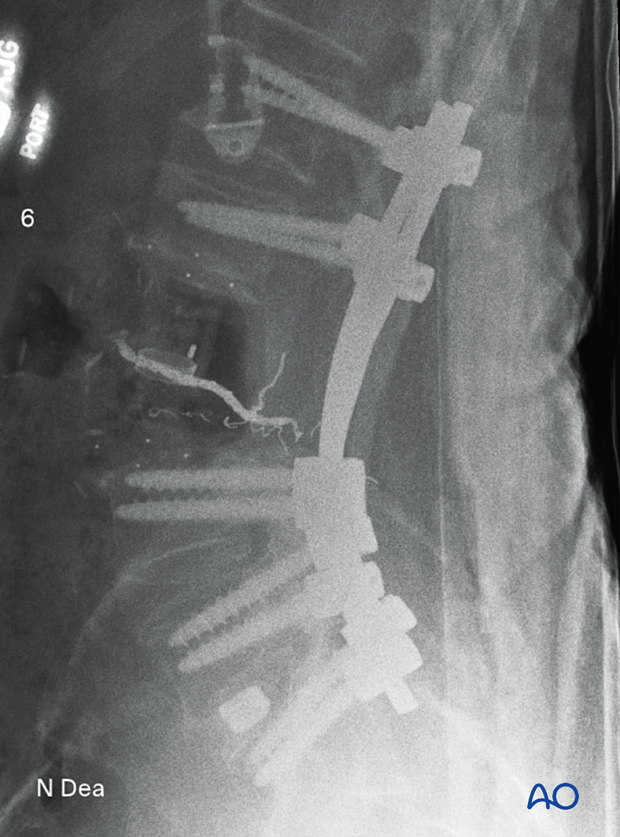
11. Intraoperative imaging
Before wound closure, intraoperative imaging is performed to check the adequacy of reduction, position, and length of screws, and the overall coronal and sagittal spinal alignment.
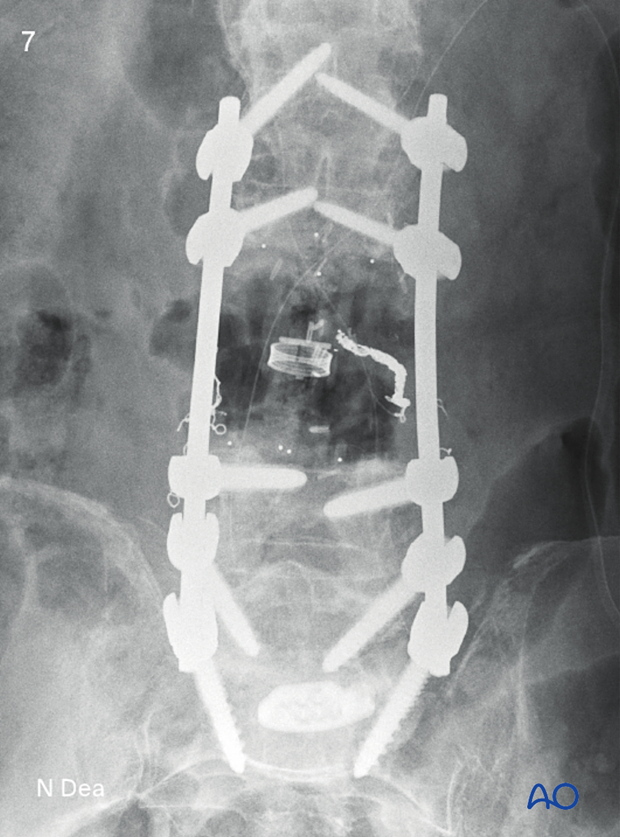
Lateral view of the above case
Axial view of the specimen

12. Anterior closure
The wound is closed in a multilayer fashion, as described in the approach.
For patients undergoing tumor surgery and/or with a history of radiation:
- Plastic surgery should perform soft-tissue reconstruction to decrease the risk of wound complications
- Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications
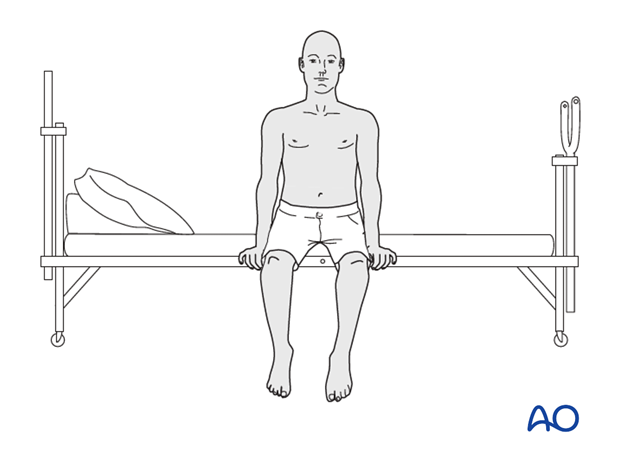
13. Aftercare
Patients are made to sit up in bed on the first day after surgery. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
Throughout the hospital stay, adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year to monitor for hardware failure and with an MRI every 6 months for tumor surveillance.
Some primary benign tumors of the spine can recur years after surgery, and long-term tumor surveillance is important.













