Posterior midline access to the thoracolumbar spine (T1–L5)
1. General considerations
The exposure for resection of primary tumors may be wider than in a trauma approach. Moreover, more lateral extension may be required. In the case of previous intralesional surgery, wound excision is advised to remove the scar as it could have been contaminated by the tumor during the first surgery. Lastly, some patients will need preoperative radiation therapy as part of their treatment plan, which could render the approach more difficult and more prone to postoperative complications. Meticulous surgical technique in the exposure and closure is warranted.
2. Skin incision
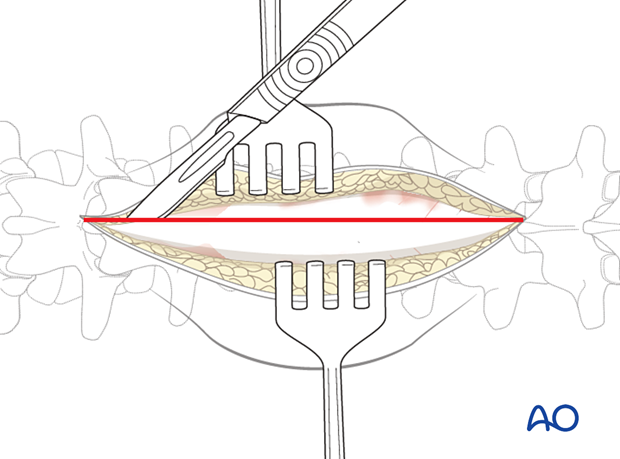
The skin and subcutaneous tissue are infiltrated with a 1:500,000 epinephrine solution to achieve hemostasis.
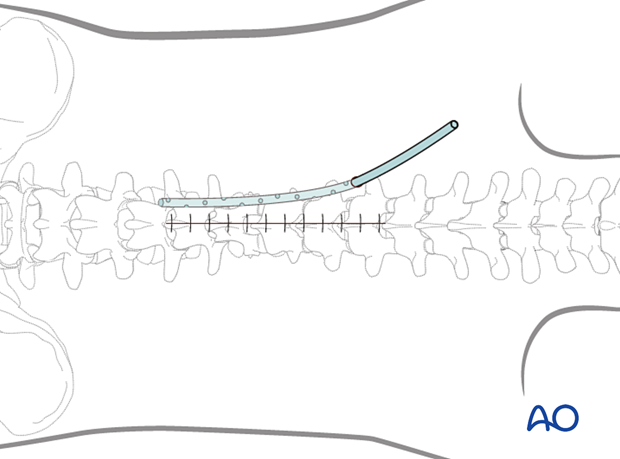
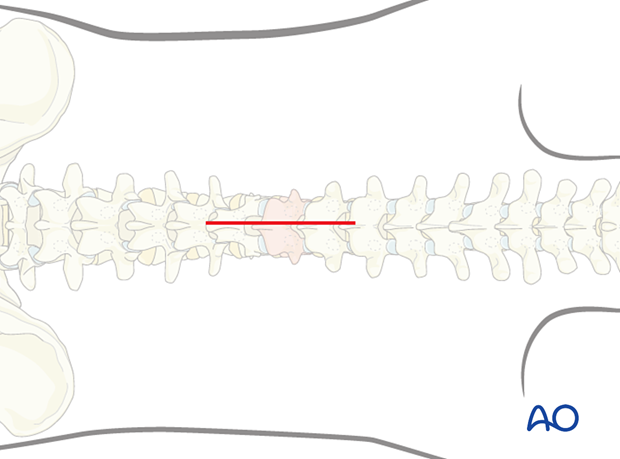
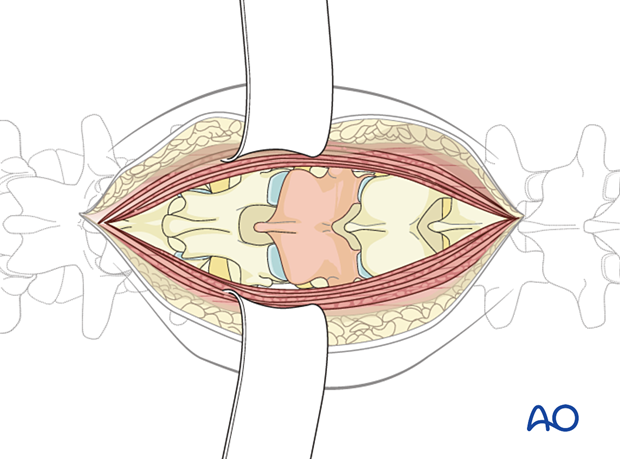
A midline skin incision is made centered over the involved segment. The length of the incision depends on the number of levels to be instrumented. For a primary tumor, at least two levels above and below the affected vertebra are exposed.
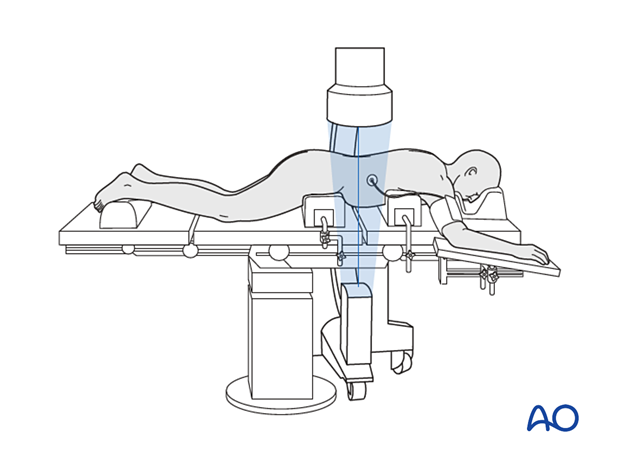
It is necessary to confirm the correct level of the approach with fluoroscopy.
3. Exposure
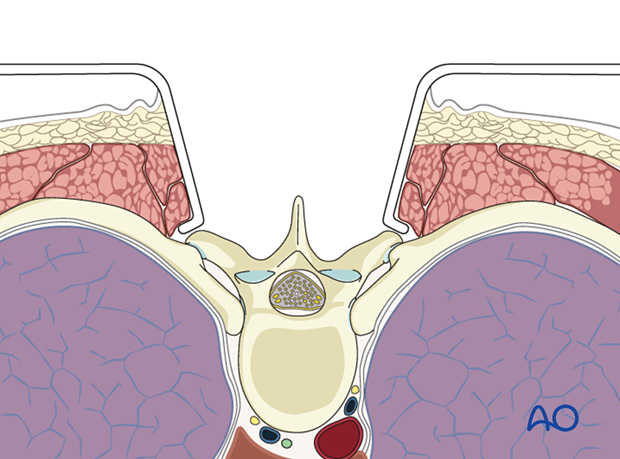
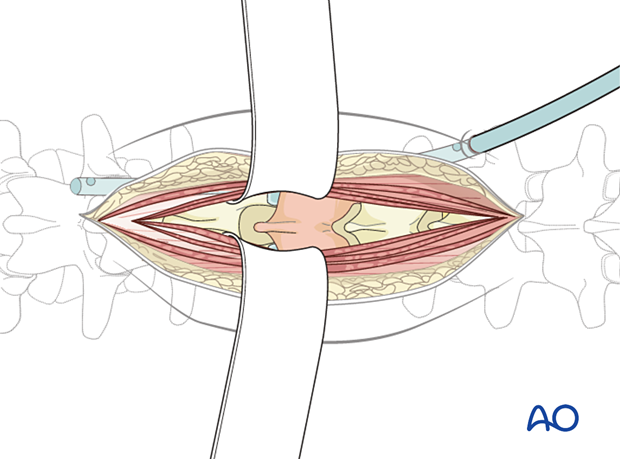
The dissection is carried out in the midline through the subcutaneous tissue and fascia to the tips of the spinous processes. Self-retaining retractors are used to expose the surgical field.
The paraspinal muscles are elevated subperiosteally from the underlying laminae, in distal to proximal direction, using a Cobb elevator. Dissection is done along the spinous process and lamina.
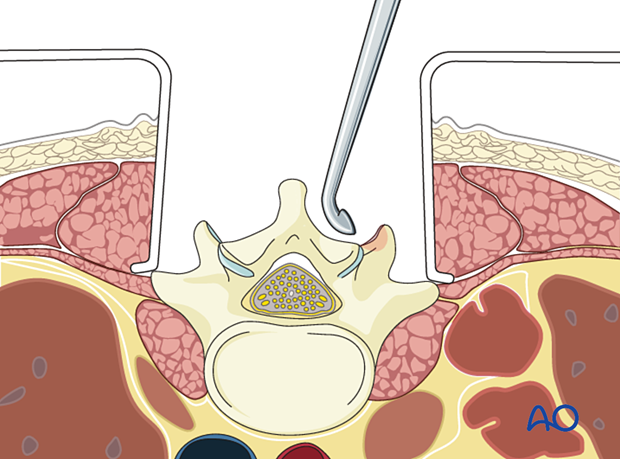
Review preoperative images to verify whether the tumor invades the lamina. In such cases, exposure of the posterior elements should be performed with great care, and the use of Cobb elevators should be avoided.
A subperiosteal dissection minimizes bleeding and muscle damage.
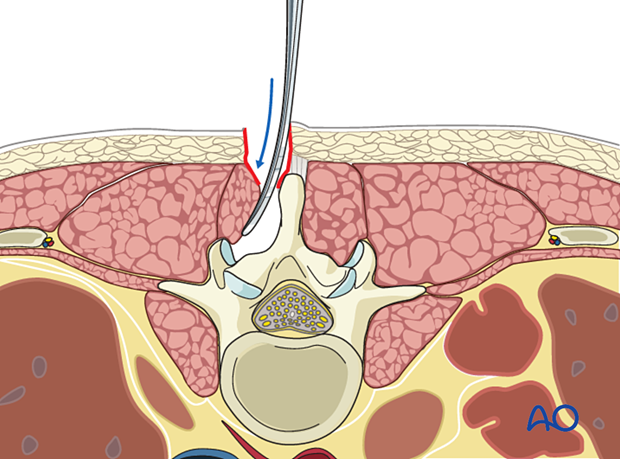
In the thoracic region, the dissection is usually taken to the tips of the transverse processes.
In the lumbar spine, the dissection is limited to the facet joints. The extent of dissection will depend upon the need and type of fusion planned.
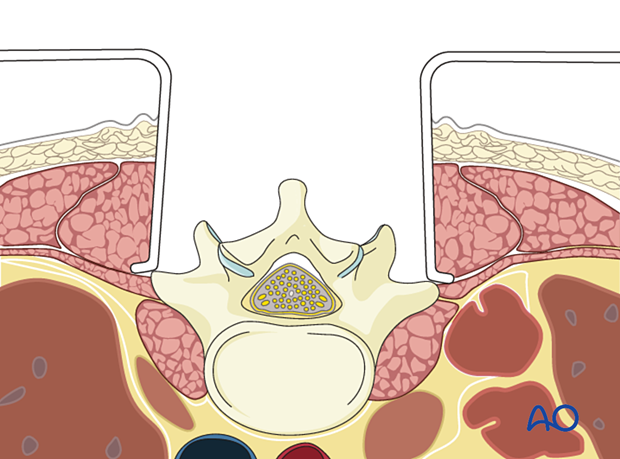
If the surgeon plans for a fusion, the facet capsule is excised, and the joint cartilage surfaces are denuded for fusion.
Posterior exposure of the thoracolumbar spine
A localizing x-ray or image intensifier check of spinal level should be obtained once exposure is completed.
4. Closure
Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications.
For patients undergoing revision surgery and/or with history of radiation, plastic surgery should perform the soft tissue reconstruction to decrease the risk of wound complications.
Drains are usually inserted via a separate stab incision.
Once the surgical procedure has been performed, tight closure of the muscle and fascial layer is performed with continuous or interrupted sutures.
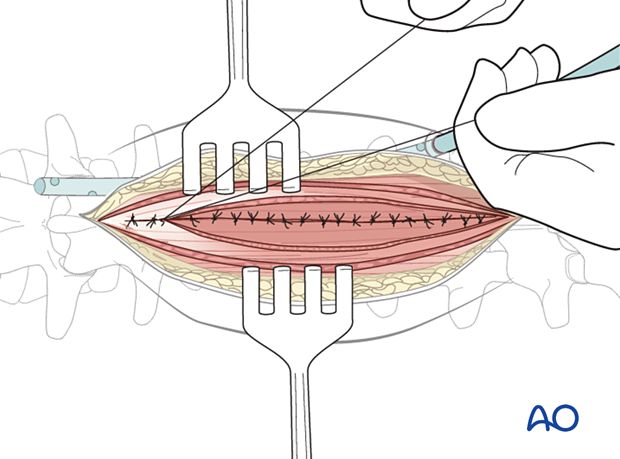
The subcutaneous layers and skin are sutured.