Posterior C1–C2 fusion
1. Introduction
The posterior C1–C2 stabilization techniques are generally more biomechanically stable.
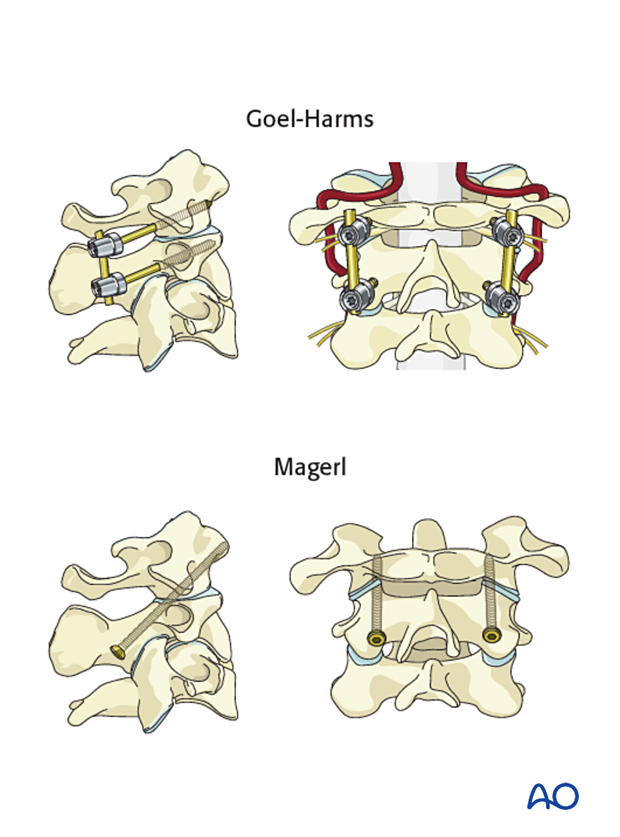
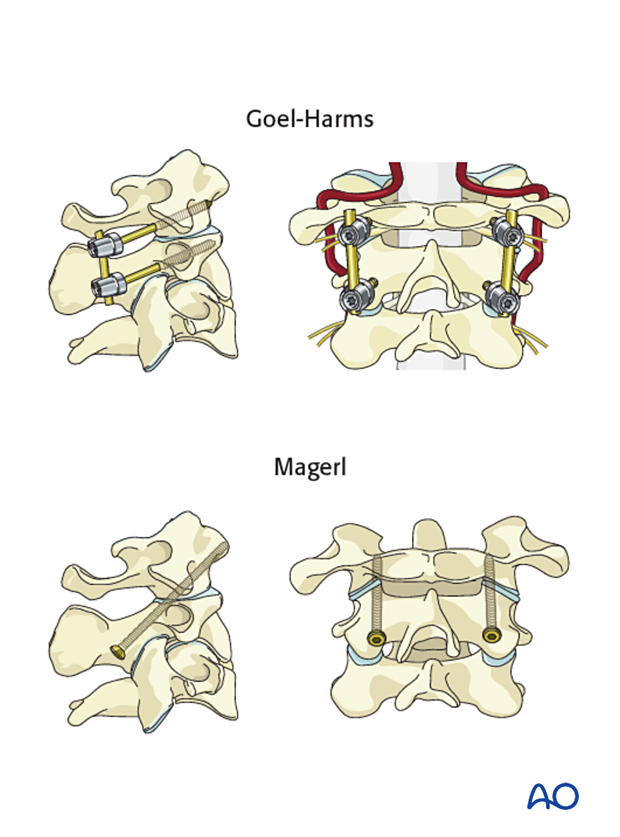
The two main techniques are:
- C1–C2 stabilization according to Goel, and subsequently Harms
- C1–C2 transarticular screw fixation according to Magerl
Both techniques can be combined with spondylodesis (fusion).
The choice between these two techniques will mainly depend on the following factors:
- Local anatomy
- Nature of the injury
- Patient factors
- Surgical skill
Reduction
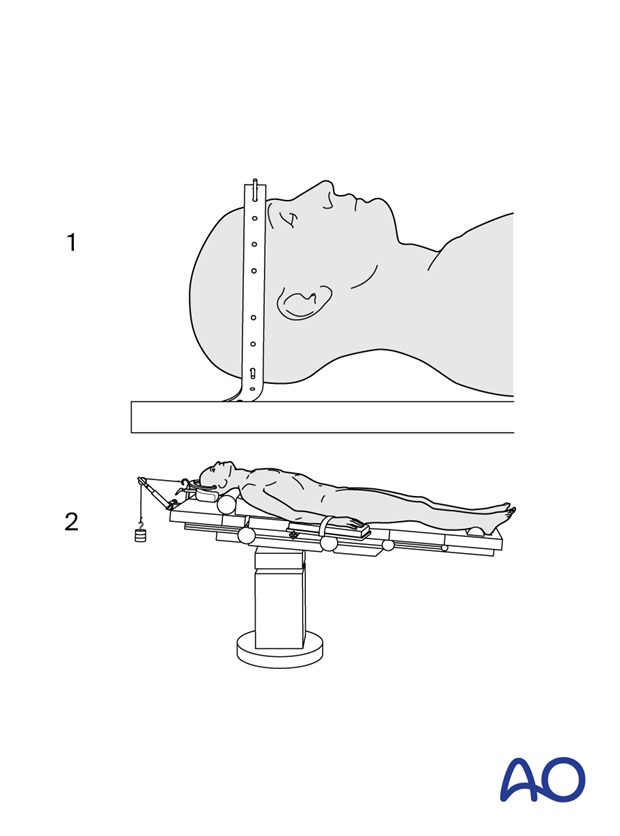
Prior to surgical access the fracture should be reduced anatomically.
Anatomical reduction is essential for the success of transarticular C1–C2 screw fixation. If this is not possible, the Goel-Harms technique should be used.
Reduction can be performed by utilizing the following techniques:
- Using halo traction preoperatively
- Using a Mayfield clamp or a similar tool intraoperatively
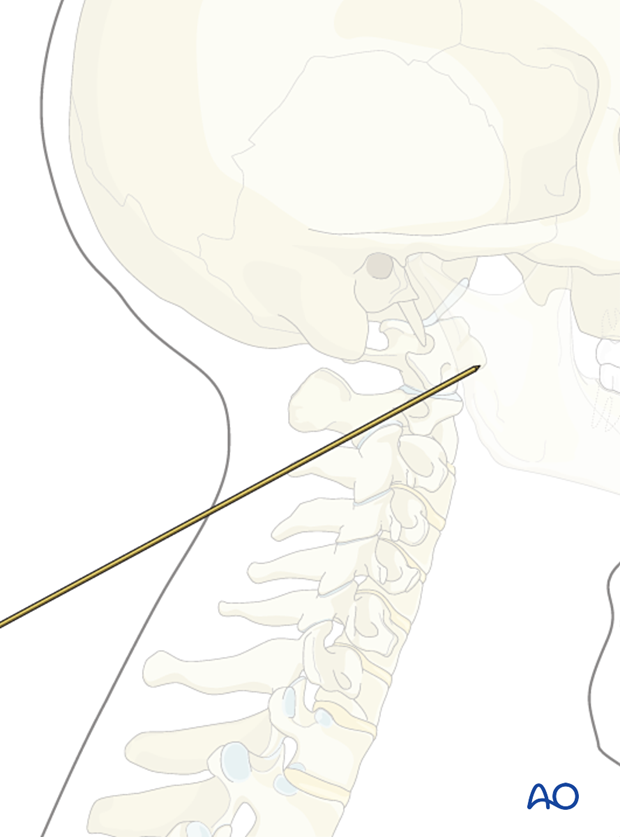
Approach
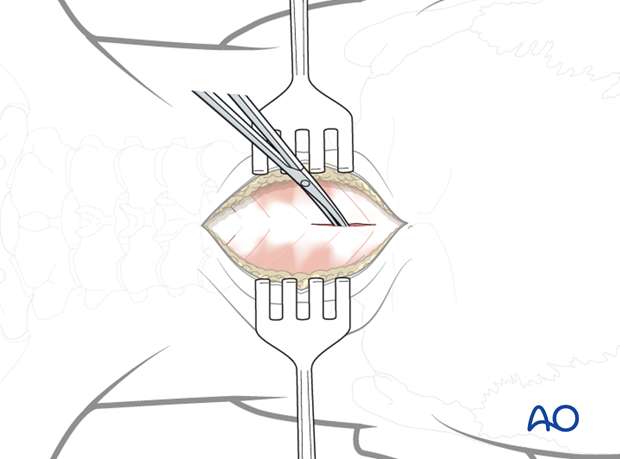
The location of the skin incision needs to be determined prior to draping the patient for insertion of transarticular screws. This is done by placing a long K-wire along the side of the neck in the intended direction of the screw and viewing on the image intensifier.
Fixation
One of the two following techniques is chosen:
- C1–C2 transarticular screw fixation according to Magerl
- C1–C2 stabilization according to Goel-Harms
2. Approach and positioning
This procedure is performed through a posterior approach with the patient placed in the prone position.
3. Magerl technique
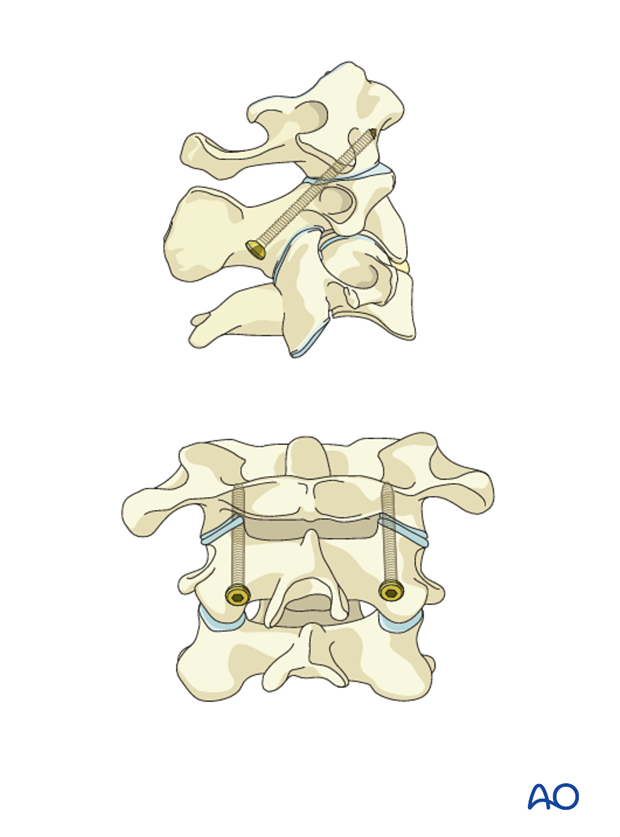
Magerl first described the use of transarticular screws. This is a relatively simple and inexpensive way to fix the C1–C2 joint. The disadvantage is that screw insertion requires fluoroscopy. Furthermore, the C2 pars must be large enough to accommodate a 3.5 mm diameter screw.
4. Goel-Harms technique
Goel and, subsequently, Harms described the use of C1 lateral mass and separate C2 fixation techniques.
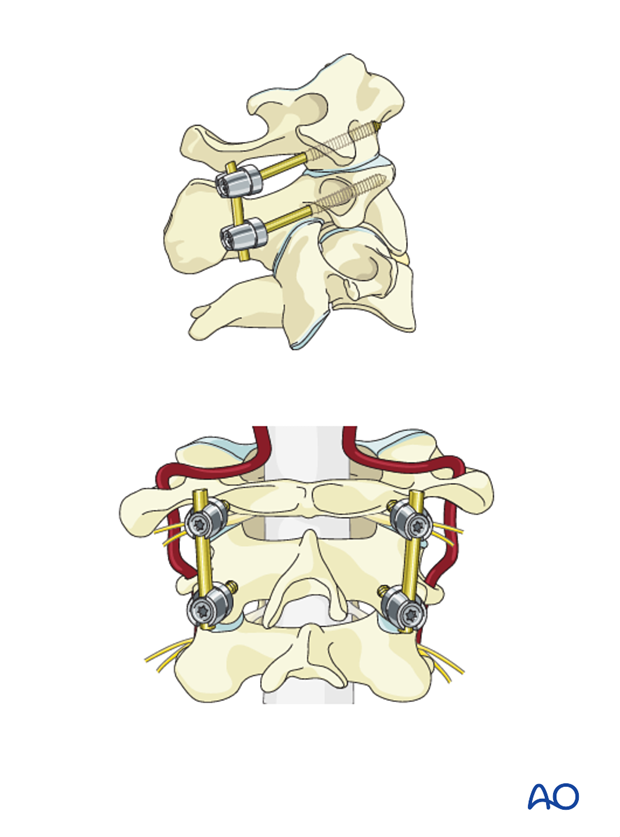
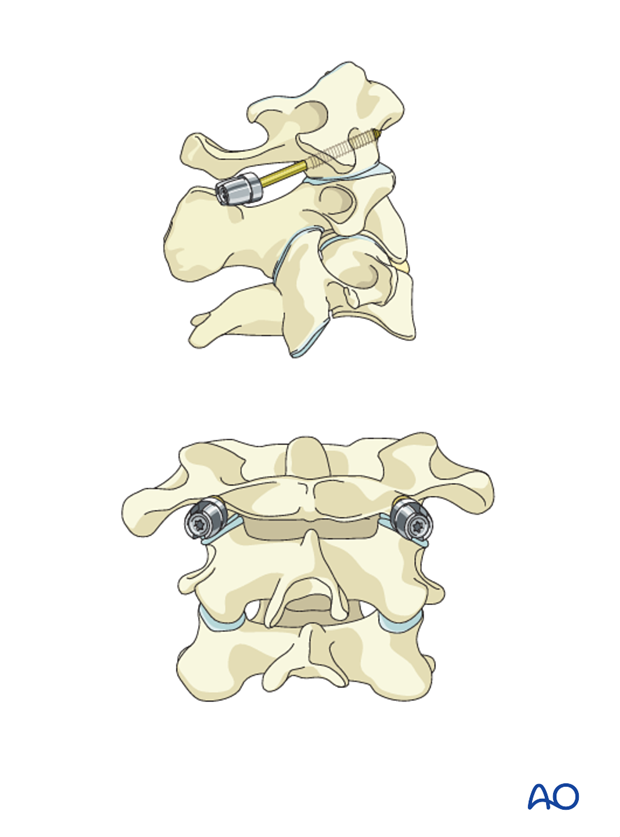
C1
C1 can be fixed using either lateral mass screws, which start just caudal to the posterior arch, or that start on top of the posterior arch and then capture the lateral mass. The latter can only be used if the posterior arch is thick enough to allow for the screw.
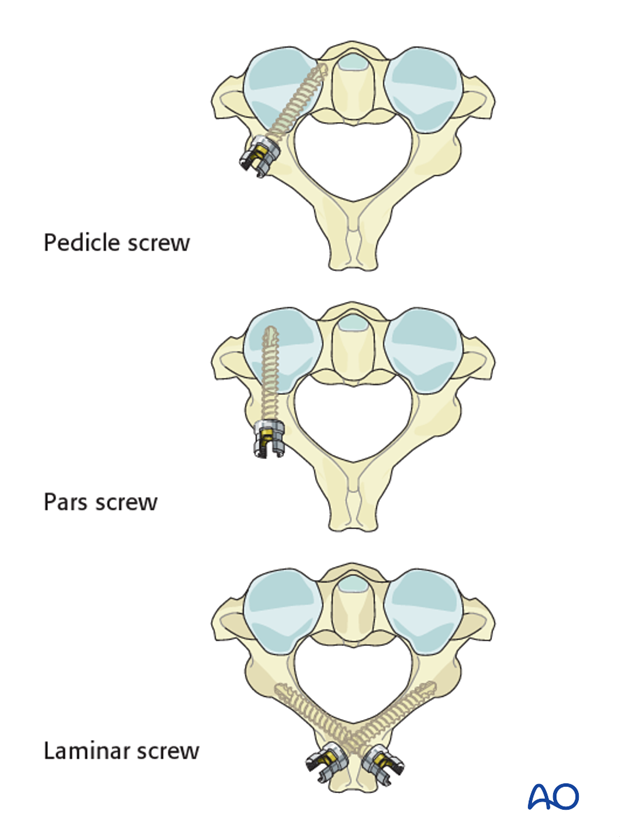
C2
C2 can be fixed using one of the following techniques:
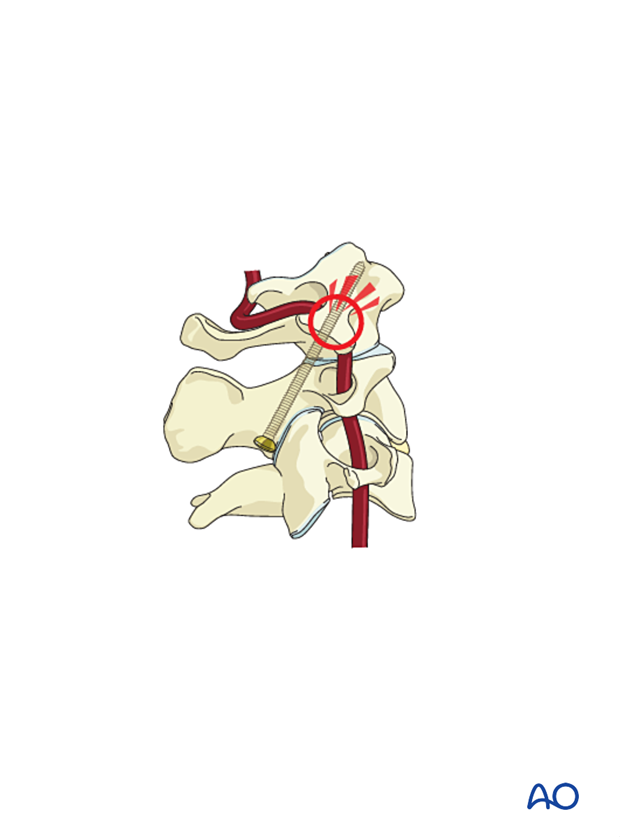
Be aware that some posterior arches have a ponticulus posticus that appears to be a thick posterior arch, but in fact is a small bridge of bone that overlies the vertebral artery.
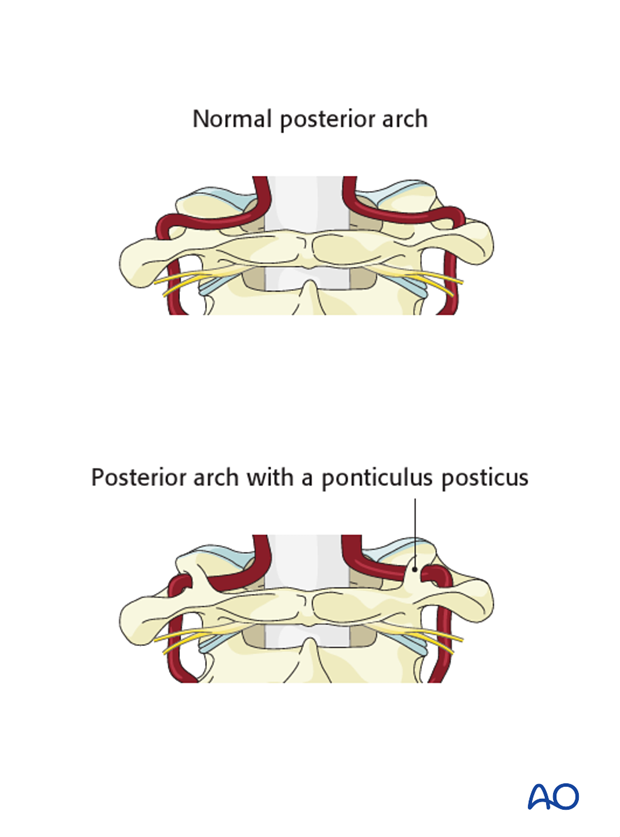
This x-ray shows the ponticulus posticus.

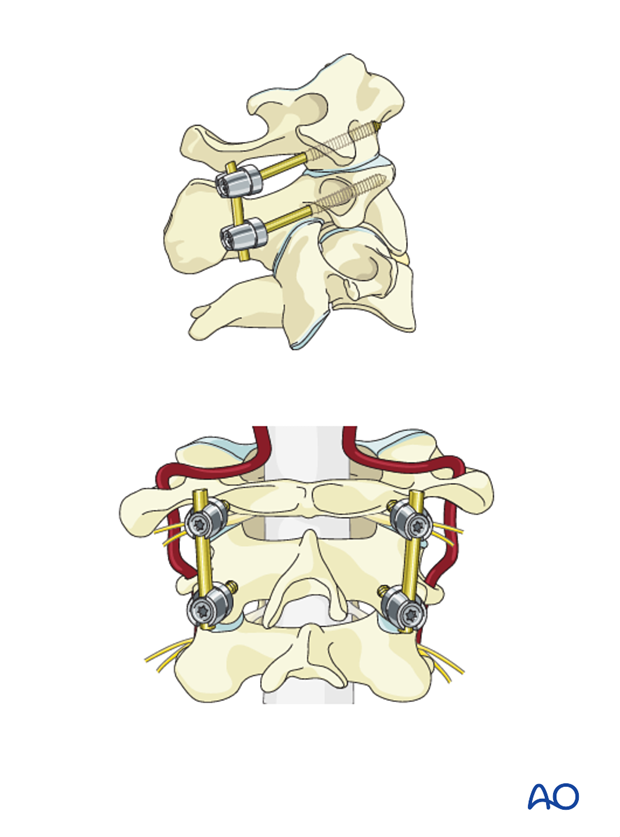
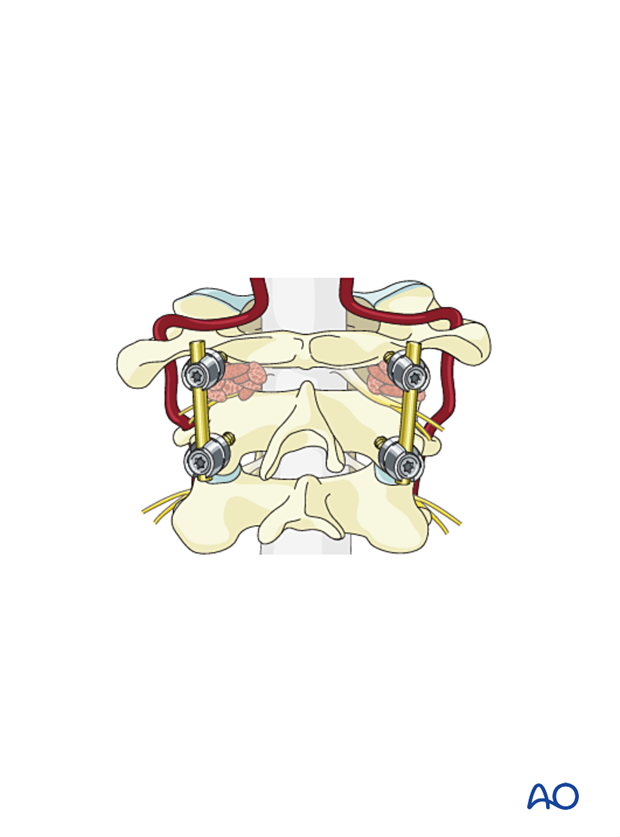
Reduction and rod placement
In case the fracture is not reduced yet, reduction can be achieved by pulling C1 posteriorly.
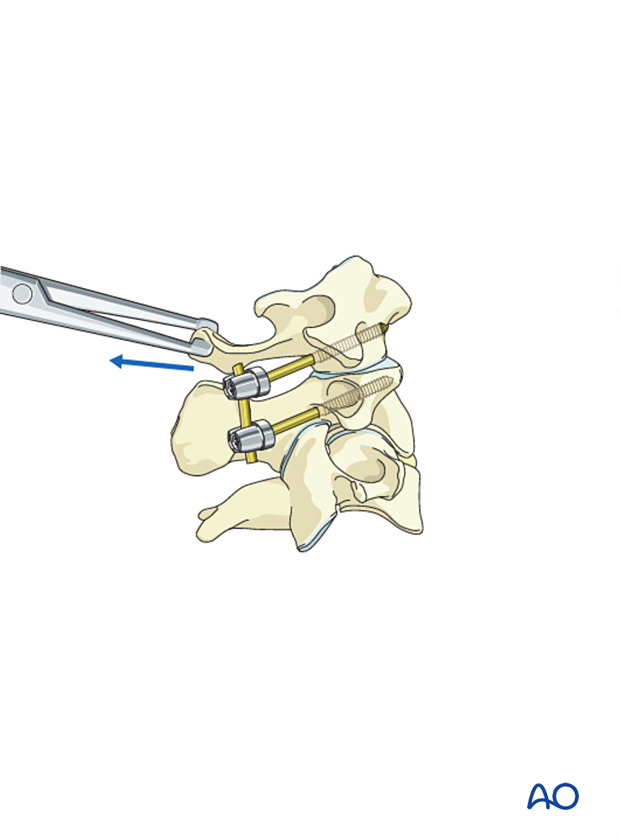
Since there are only two screws on each side, a straight rod is placed to link them. The nuts are then placed and tightened. Keep the rods as short as possible.
5. Posterior fusion
Fusion is typically indicated in:
- elderly patients when implant removal is not planned
- complex injuries requiring a long time to heal
Bone grafting following Goel-Harms technique
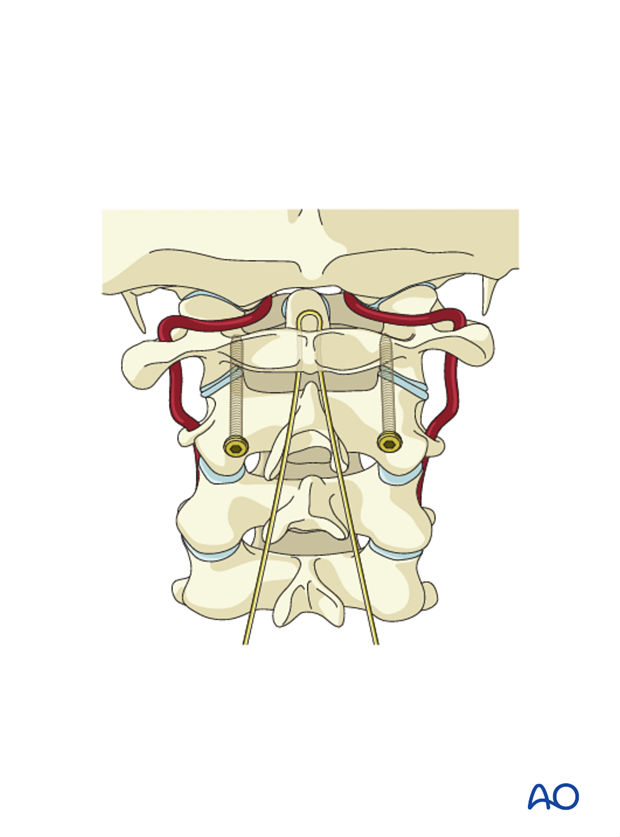
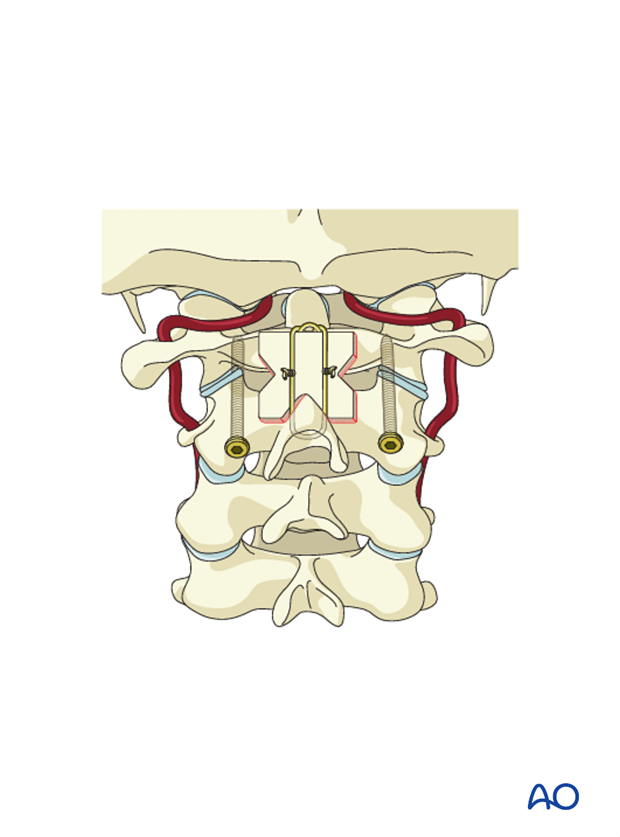
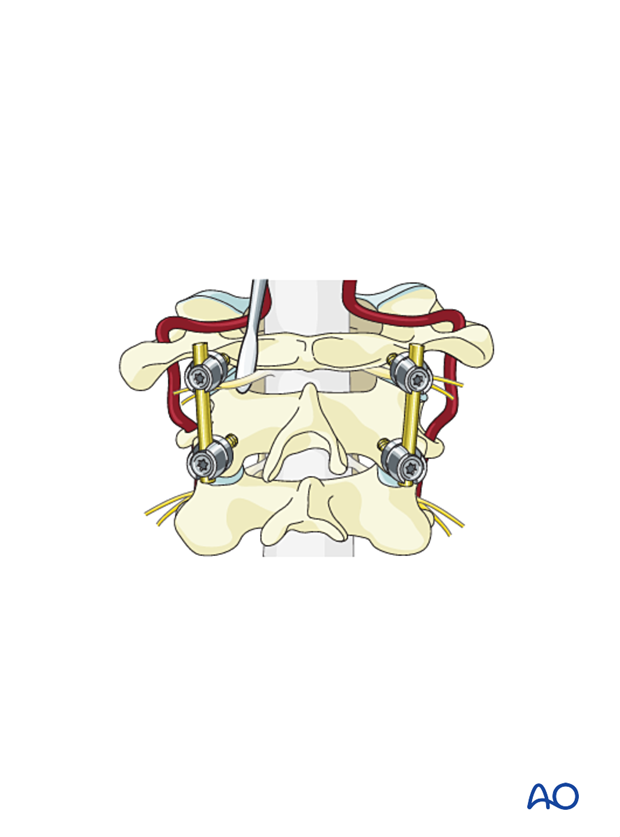
Fashion the bone graft as illustrated.
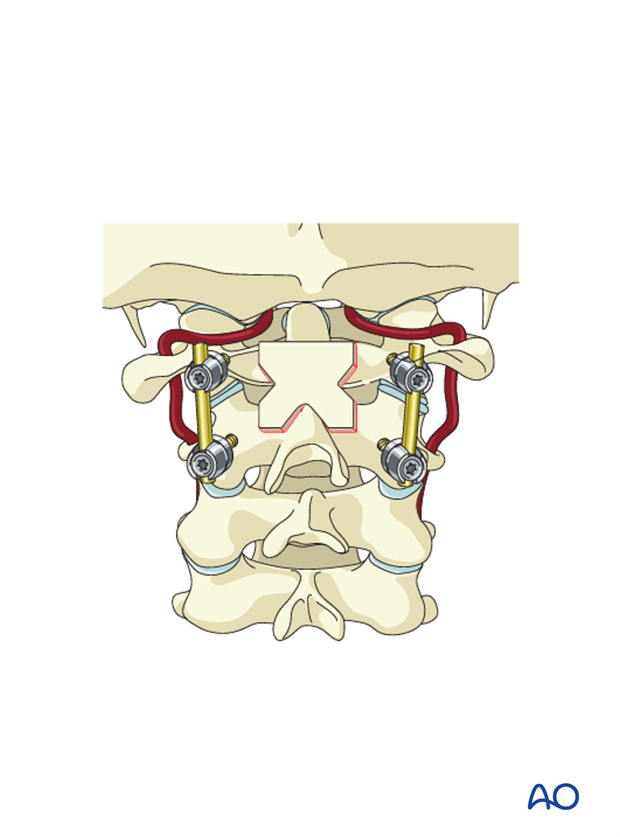
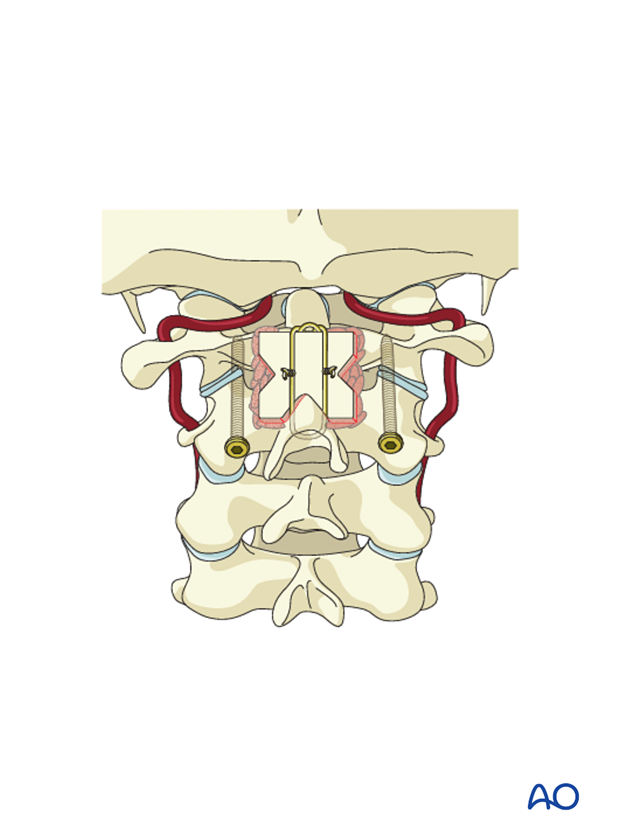
Place a wire under the left rod over the graft and under the right rod and cinch it in place to push the graft onto the decorticated C1 posterior arch and C2 lamina.
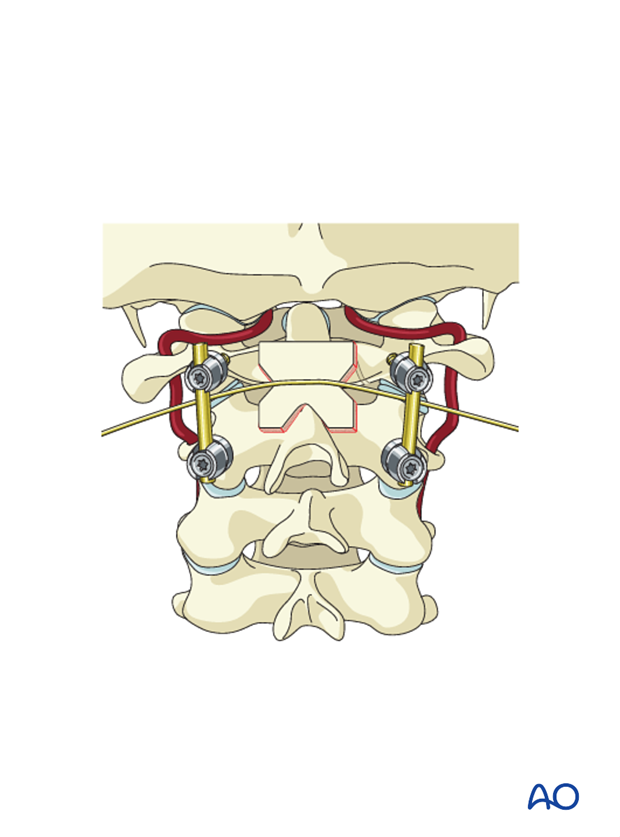
Add additional cancellous autograft strips to fill the voids between the lamina of C2 and the structural autograft.
Bone grafting following transarticular screw insertion
Optionally, bone grafting following trans-articular screw insertion can be used. The bone graft is the same as for the Goel/Harms technique, but the wiring technique differs. Since there are no rods, the graft is secured with wires.
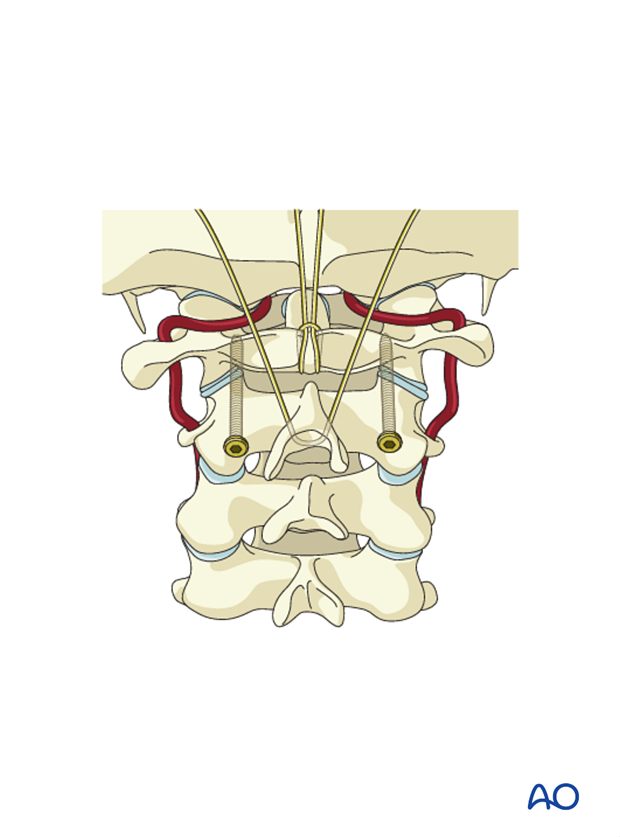
A loop of wire is passed under the arch of C1.
The two free ends are passed through this loop. A second wire is then passed through the spinous process of C2.
After decorticating the C1 posterior arch and the C2 lamina, the graft is placed, and the two wires are twisted together over the graft.
Additional cancellous autograft strips are added to fill the voids between the lamina of C2 and the structural autograft.
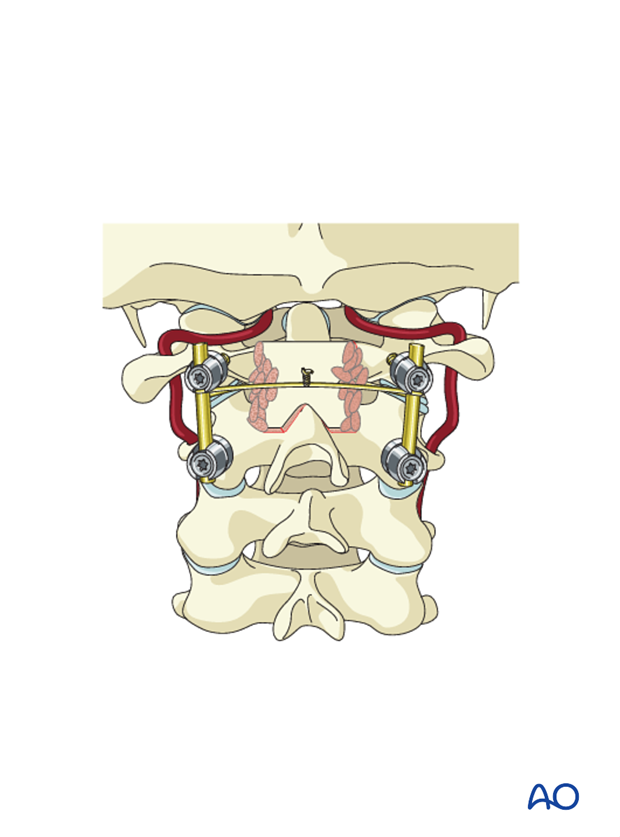
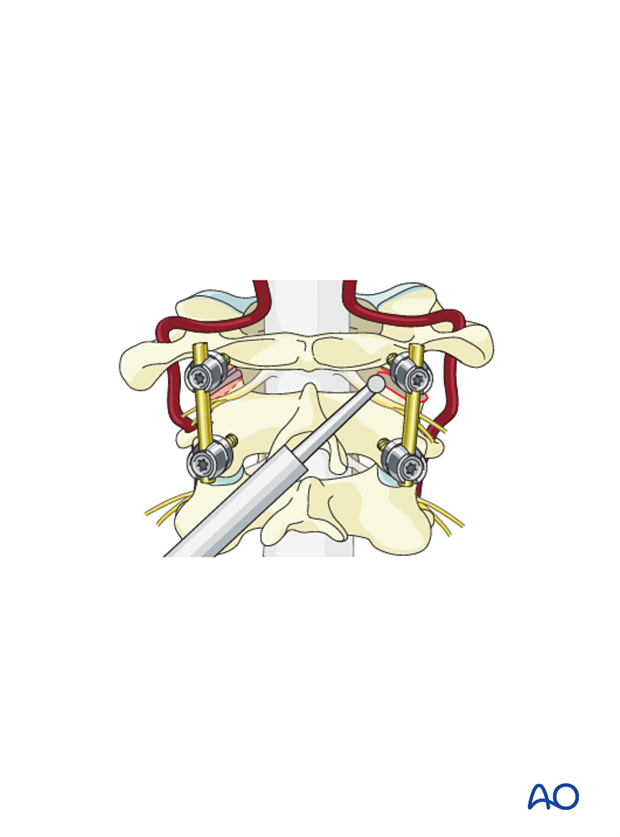
Intraarticular C1–C2 fusion
Alternatively (or additionally) the facet joints of C1–C2 can be opened, decorticated, and fused.
Cancellous allograft can be placed intra-articularly after decorticating.
To decorticate the joint, reflect the C2 nerve caudally.
Burr into the joint or use a curette to scrape the articular cartilage. Be aware that the vertebral artery can in some cases be just below the articular surface of C2. This must be verified by CT scan prior to the surgery.
6. Aftercare
Patients are made to sit up in bed on the evening following the operation.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed favorable for fracture healing. A collar is optional.
Patients with intact neurological status are made to stand and walk on the first day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.













