Posterior access to C1–C2
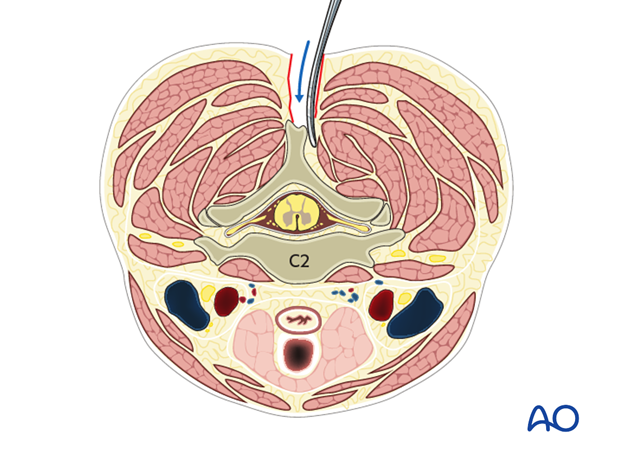
1. Incision
An incision is made in the midline starting at the top of C1 and ending at the bottom of C2. The incision is typically no more than 5–7 cm in length.
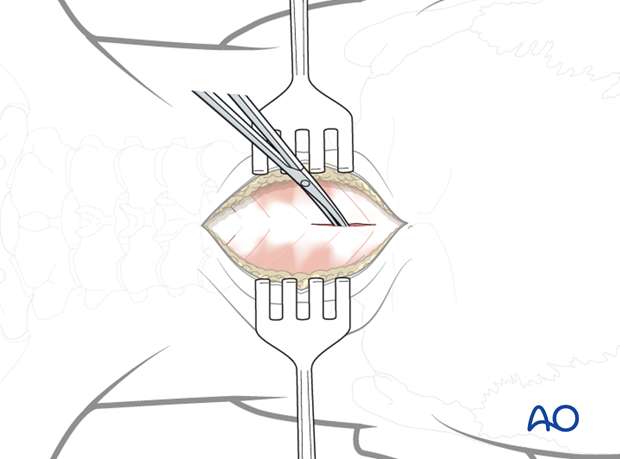
2. Dissection
Using electrocautery or scissors, dissect down to bone in the intermuscular and relatively avascular plane of the midline.
Wandering laterally into the muscles will markedly increase blood loss.
Identify the midline of the posterior arch of C1.
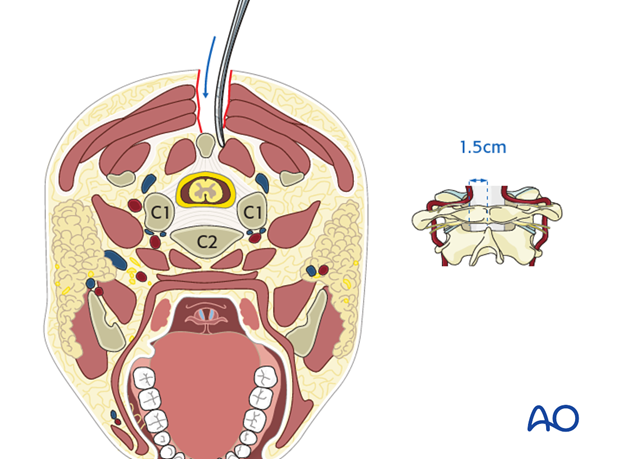
3. Exposure of posterior aspect of C1
Using a Cobb elevator, gently push the soft tissues subperiosteally off the posterior arch of C1.
If lateral mass screws are planned for C1, the posterior ring is exposed all the way to the lateral border of the lateral mass.
Careful dissection is essential to avoid compromising the vertebral artery, which lies only 1.5 cm lateral to the midline.
4. Exposure of posterior aspect of C2
Subperiosteally, dissect the soft tissues off the spinous process, lamina, and facet of C2.
Do not detach the soft tissues between C2 and C3 to prevent postoperative kyphosis.
The semispinalis cervicis, the most important extensor muscle of the neck, attaches to the spinous process of C2. Care must be taken to preserve the attachment of this muscle to the caudal border of the C2 spinous process.
5. Dissection for C1 lateral mass screw insertion
If C1 lateral mass screws are planned, reflect the C2 nerve root and its associated veins caudally. This dissection can result in severe bleeding and must therefore be performed with great care.
Using a Penfield 4 dissector, gently push the C2 nerve root off the caudal border of the posterior arch of C1 until the lateral mass can be palpated with the Penfield 4.
If bleeding is encountered, pack it off with Gelfoam soaked in thrombin together with a small paddy. Leave this in place and expose the other side. If bleeding is encountered on the contralateral side, continue the dissection on the ipsilateral side.
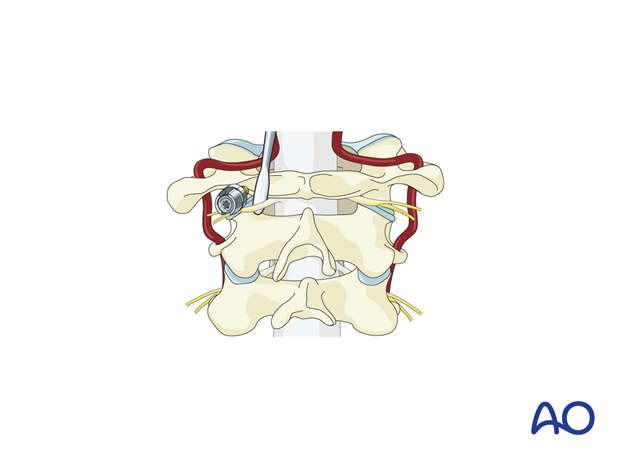
Some surgeons prefer to cut the C2 nerve to gain wide exposure to this area. However, 15–20% of patients whose C2 nerve is cut will develop chronic pain requiring medication.
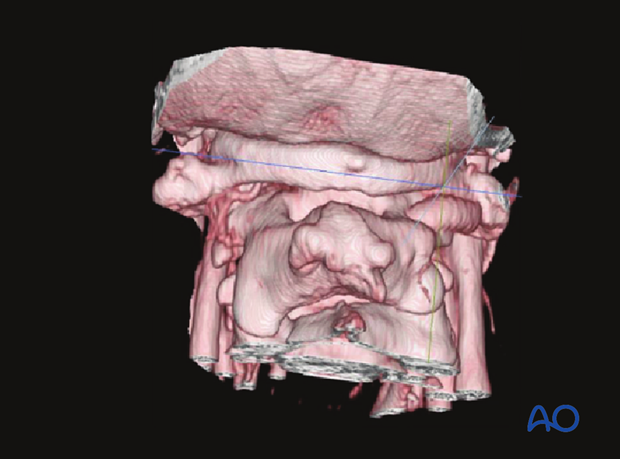
Also, 10–15% may have an intersegmental artery or an anomalous vertebral artery along with the nerve in this region. A preoperative CT angiogram is recommended if the surgeon plans to cut the C2 nerve.
In the 3D CT angiogram shown there is an intersegmental artery bilaterally with the right side being dominant.
6. Closure
Prior to closure:
- Achieve meticulous hemostasis
- 500 mg of vancomycin powder may be placed in the wound at the surgeon’s discretion
Do not use Gelfoam over an open dura as it will expand and compress the spinal cord.
Meticulously reapproximate all the muscles with numerous interrupted sutures placed 1 cm apart. This will prevent wound and muscle dehiscence as well as provide a cosmetically pleasing result. With each layer of closure, compress the wound for 30–60 seconds to prevent postoperative hematoma formation.
A drain is typically not necessary as long as meticulous hemostasis is achieved.