Posterior C1–C2 fusion
1. Introduction
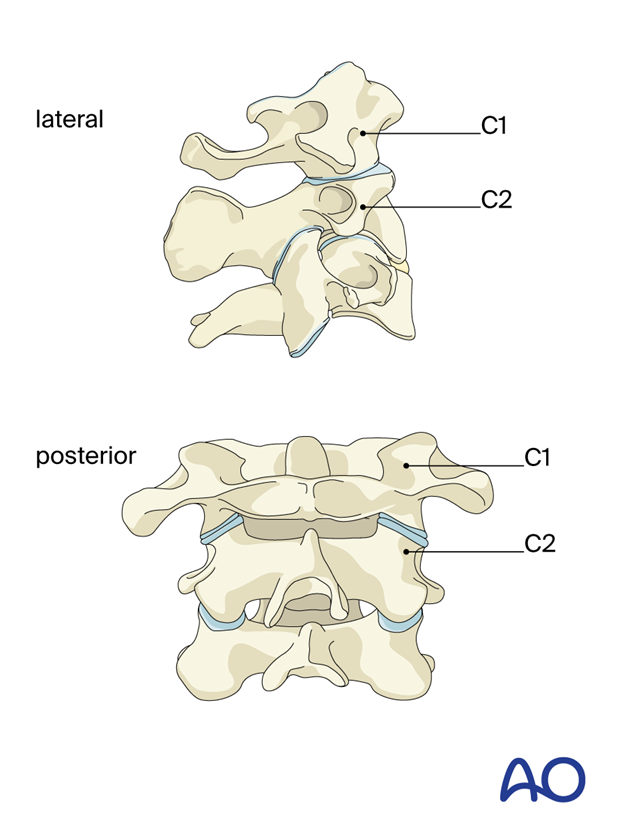
C1 and C2 are anatomically unlike any other vertebrae in the spine. Their unique anatomy allows for about 35° of the flexion-extension motion at the occipital C1 joint and about 50° of the rotational motion at the C1–C2 joint. Consequently, they are the most important vertebrae for the cervical range of motion.
When treating fractures of these two vertebrae, every effort should be made to avoid arthrodesis of the two joints.
The treatment goals are to stabilize the spine until the fractures have healed or to perform an arthrodesis in cases where stability cannot be achieved after healing is completed (such as with ligament ruptures).
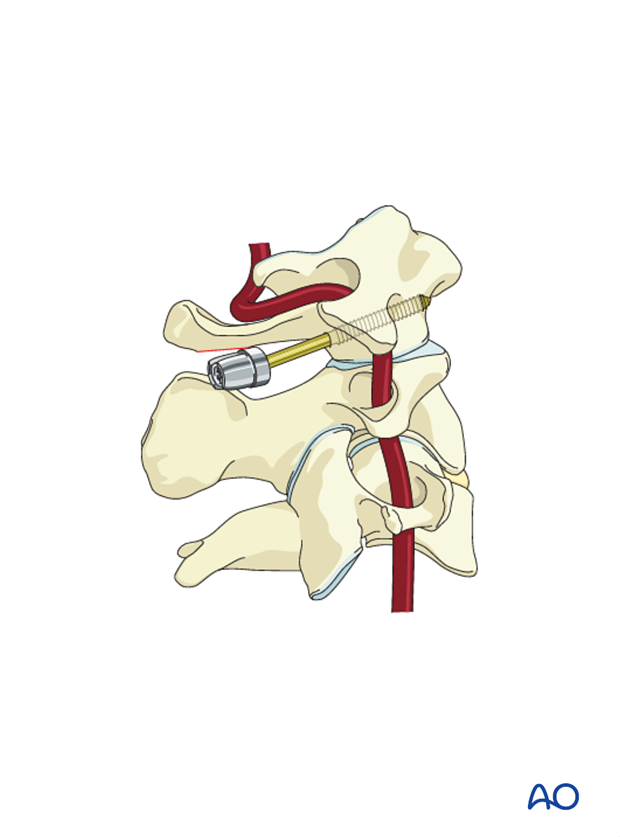
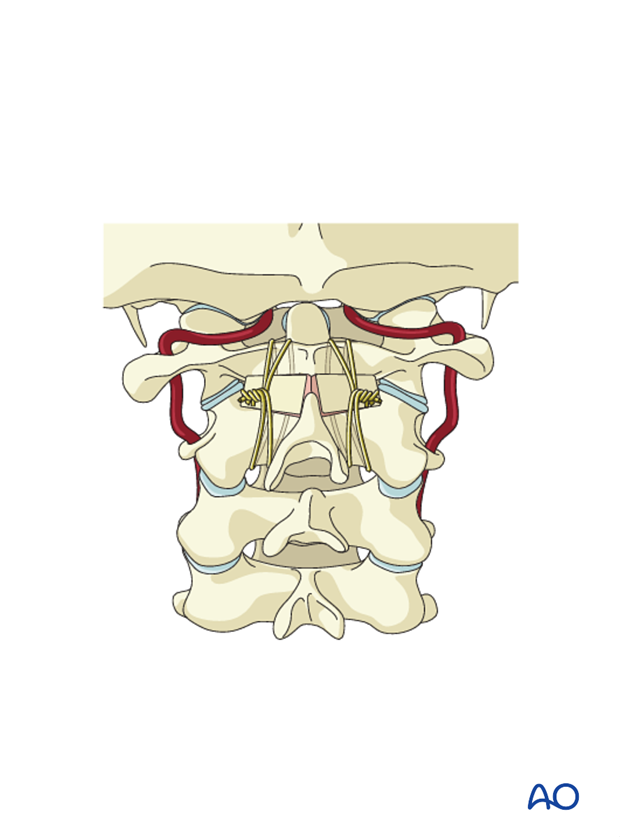
The vertebral artery trajectory must be fully evaluated before any surgery in this area.
With acute fractures, reduction is usually not difficult. With chronic fractures the fractured fragment can be manipulated by placing a lateral mass screw into it and using the screw as a "joystick".
While a range of techniques can be used to treat this fracture, if a C1 lateral mass screw can be placed lateral to the fracture line, it can aid in the anatomic reduction of the displaced fracture, which minimizes the risk of posttraumatic arthritis.
In rare cases, the transverse atlantal ligament remains intact. If the fracture fragments can be reasonably closely realigned such that healing is likely, internal fixation can be performed.
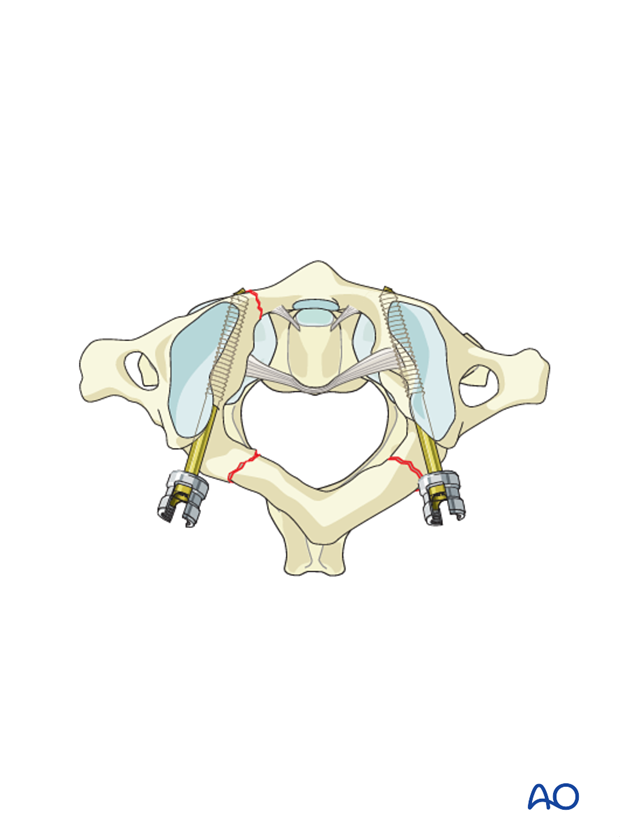
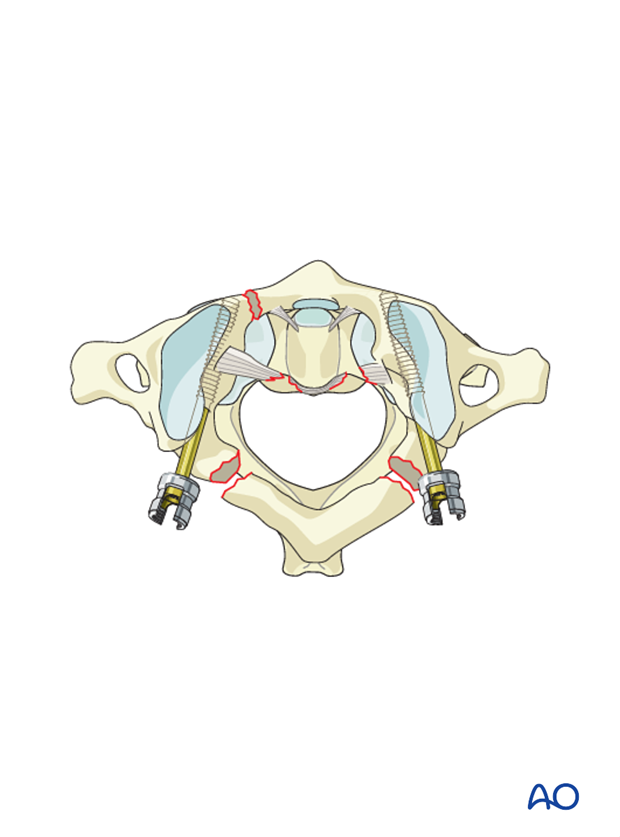
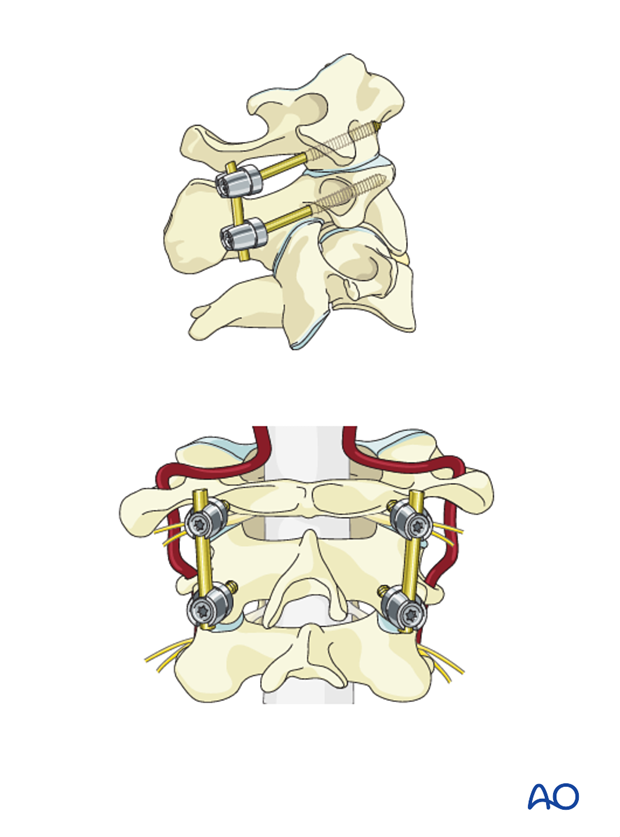
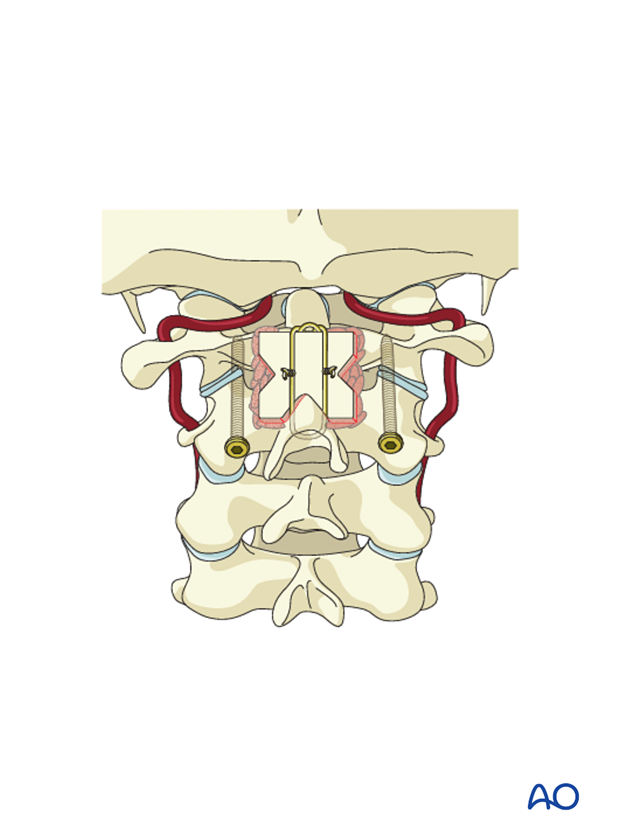
Bilateral C1 lateral mass screws compressed with a rod are the preferred choice.
2. Approach and positioning
This procedure is performed through a posterior approach with the patient placed in the prone position.
3. Wires and structural bone grafts
In the past a technique that utilized wires and structural autograft was used. This technique is rarely used now and will not be described here.
4. Magerl technique
Magerl first described the use of transarticular screws. This is a relatively simple and inexpensive way to fix the C1–C2 joint. The disadvantage is that screw insertion requires fluoroscopy. Furthermore, the C2 pars must be large enough to accommodate a 3.5 mm diameter screw.
5. Goel-Harms technique
Goel (1994), and subsequently Harms (2001), described the use of C1 lateral mass and separate C2 fixation techniques.
Further reading
Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir 1994;129(1–2): 47–53.
Harms J, Melcher P. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26: 2467–71.
C1
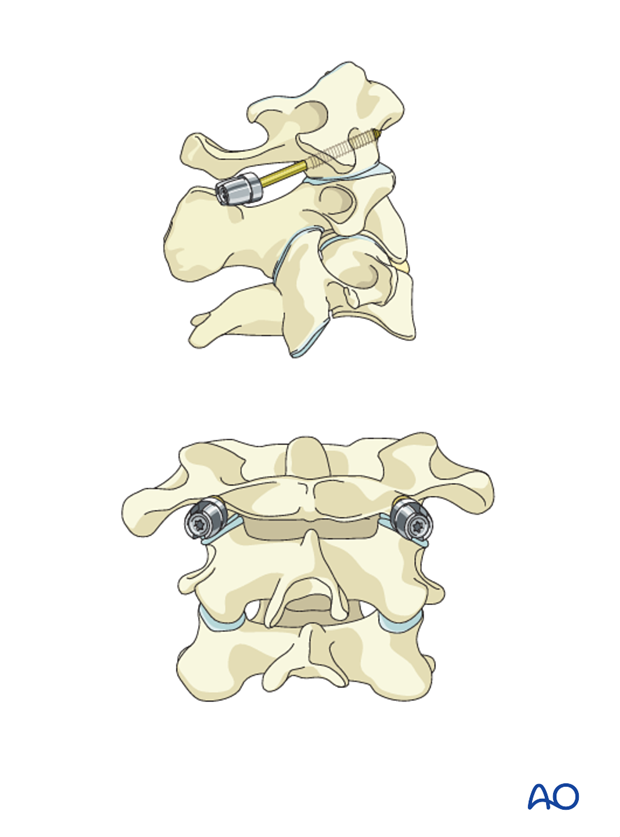
C1 can be fixed using either lateral mass screws that start just caudal to the posterior arch or that start on top of the posterior arch and then capture the lateral mass. The latter can only be used if the posterior arch is thick enough to allow the screw.
C2
C2 can be fixed using one of the following techniques:
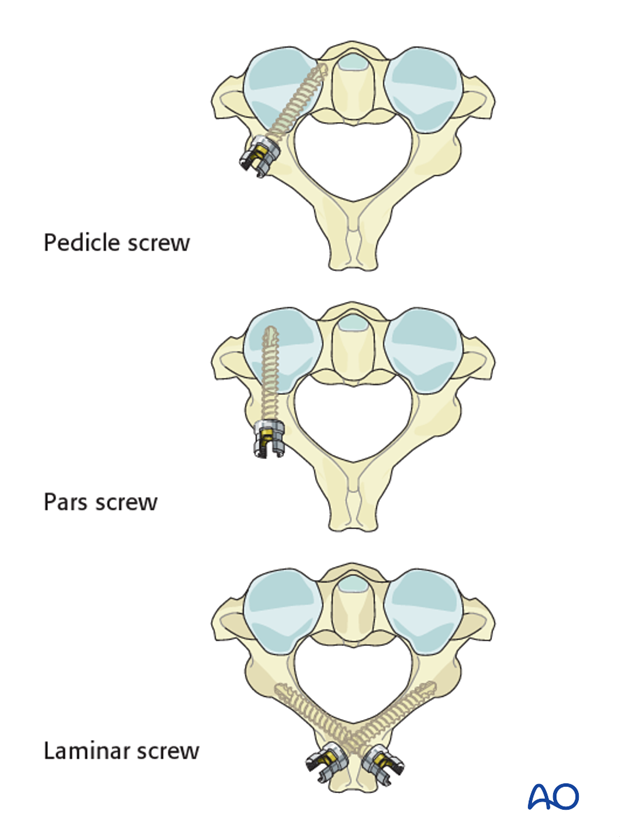
Be aware that some posterior arches have a ponticulus posticus that appears to be a thick posterior arch but, in fact, is a small bridge of bone that overlies the vertebral artery.
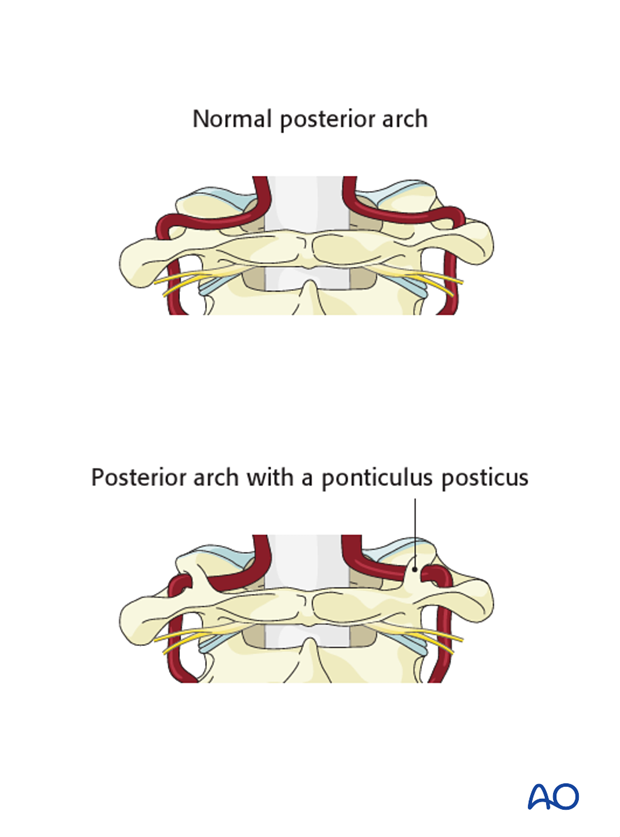
This x-ray shows the ponticulus posticus.

Rod placement
Since there are only two screws on each side, there is no need for rod bending. A straight rod is placed and tightened. Keep the rods as short as possible.
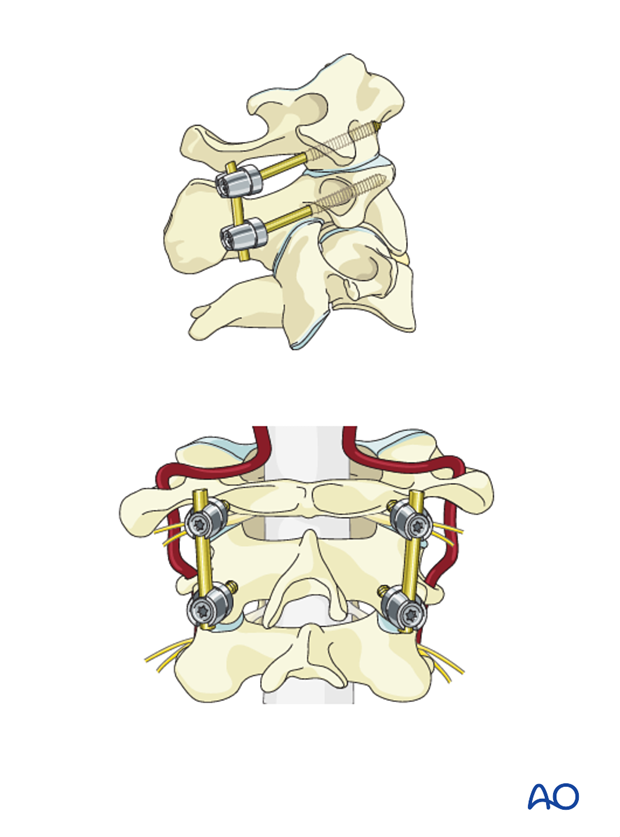
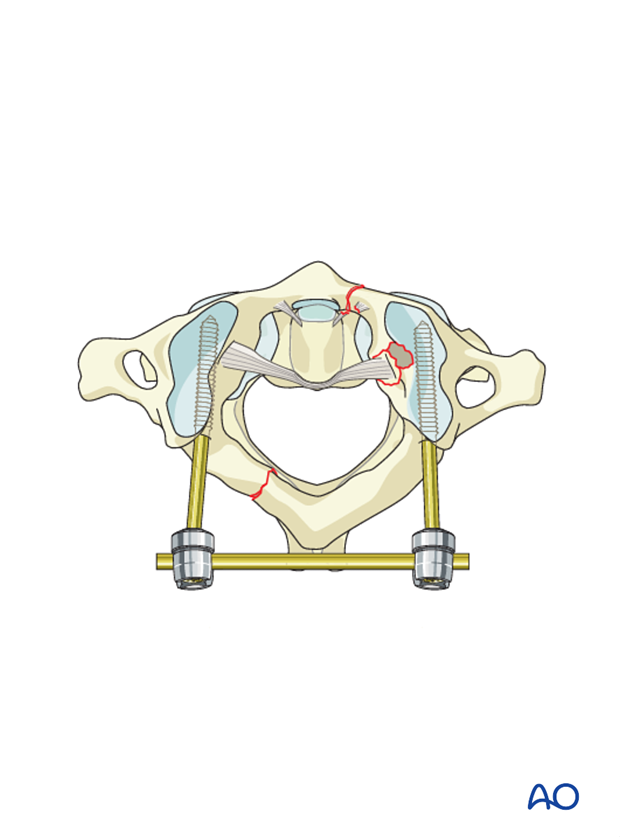
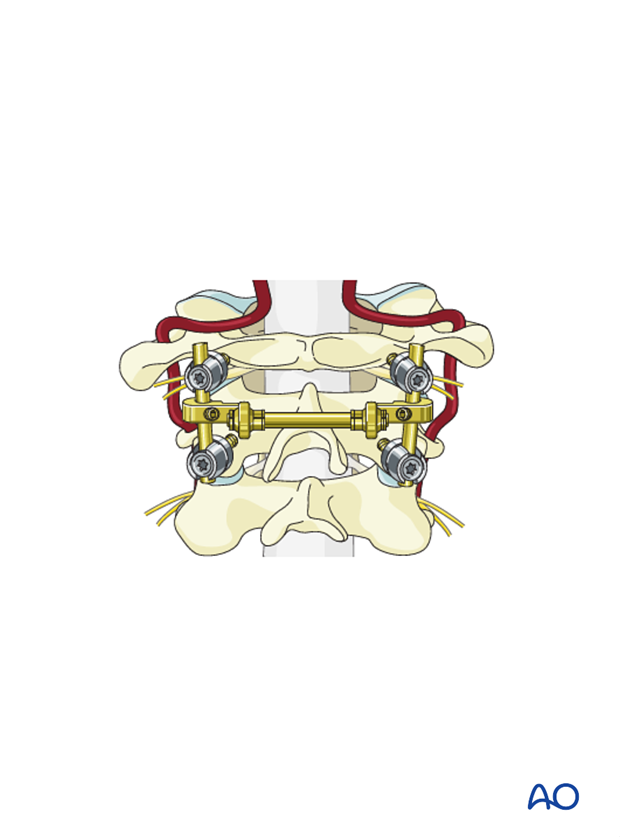
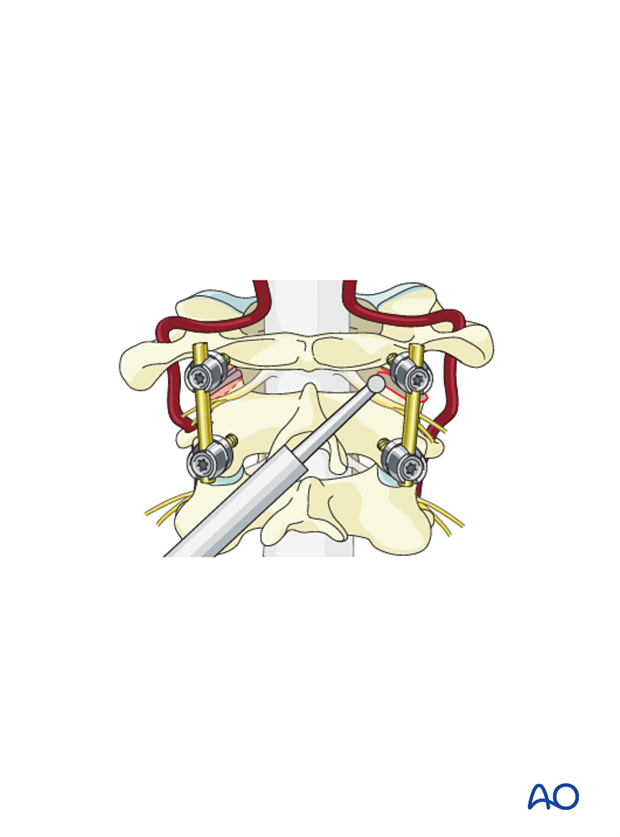
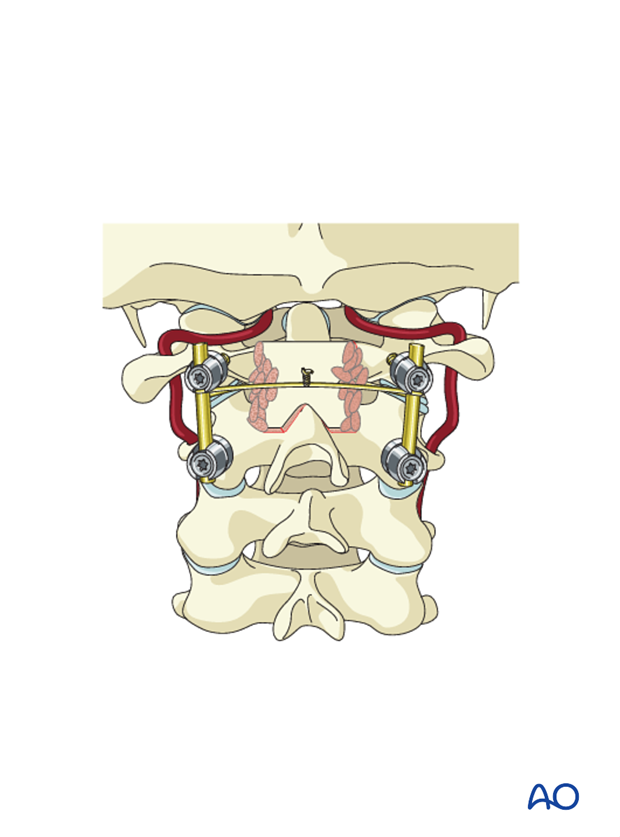
If there is spreading of the ring of C1 or a laterally displaced intra-articular fracture, the C1 lateral mass screws can be used to reduce the displacement. After placing bilateral C1 and C2 screws and rods, a cross link can be placed and used to compress the rods together, thereby reducing the fracture.
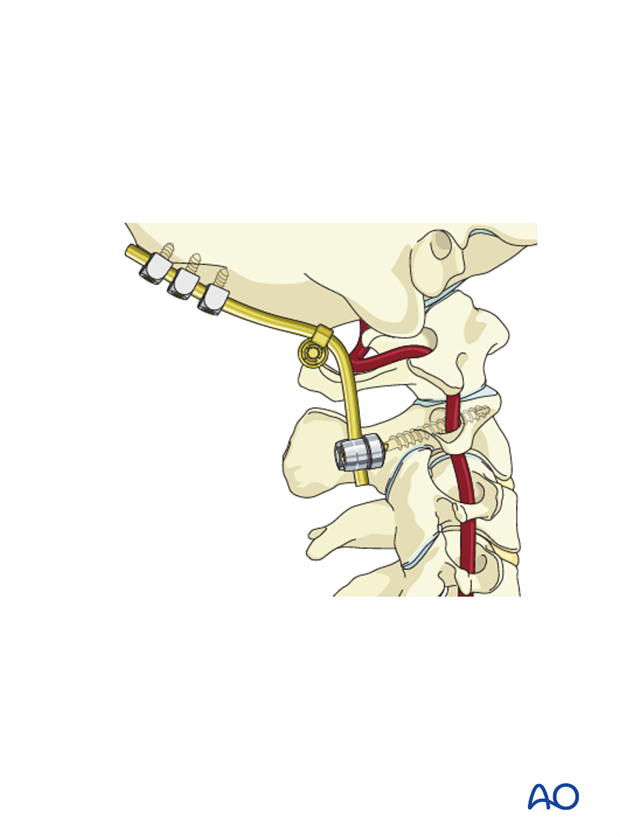
An alternative in patients with an anatomic reduction of the lateral mass fracture, but in whom C1 lateral mass fixation is not possible, is to instrument up to the skull but only fuse the C1–C2 joint. Once the fractures have healed, the instrumentation can be removed.
6. Posterior fusion
Cancellous allograft can be placed over the decorticated area.
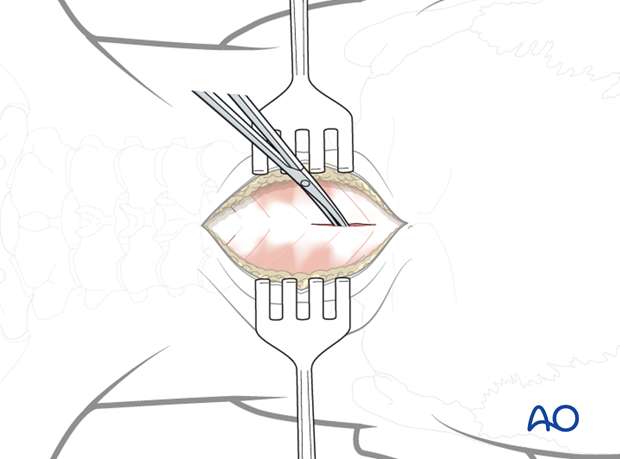
To decorticate the joint, and add interarticular graft, the C2 nerve must be reflected caudally.
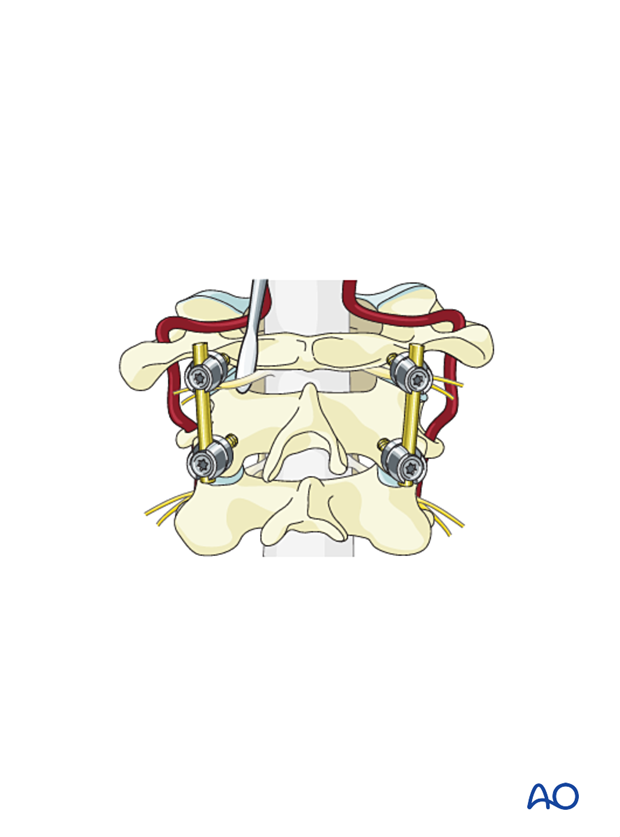
Burr into the joint or use a curette to scrape the articular cartilage. Be aware that the vertebral artery can, in some cases, be just below the articular surface of C2. This must be checked previously with a CT scan.
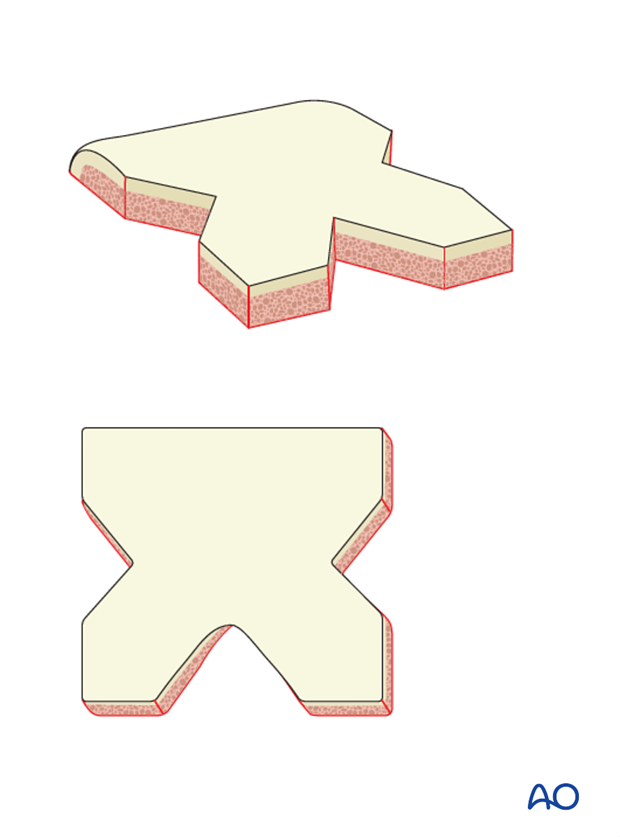
If an intra-articular fusion is not performed, a structural cortical, cancellous graft must be used to bridge the C1 posterior arch to the C2 lamina. Autograft from the iliac crest is the most reliable.
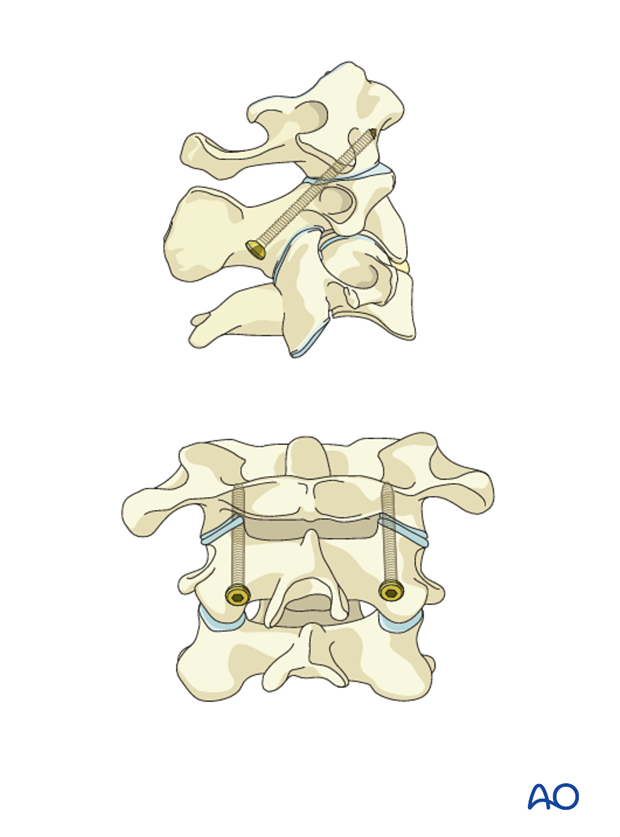
Bone grafting following Goel-Harms technique
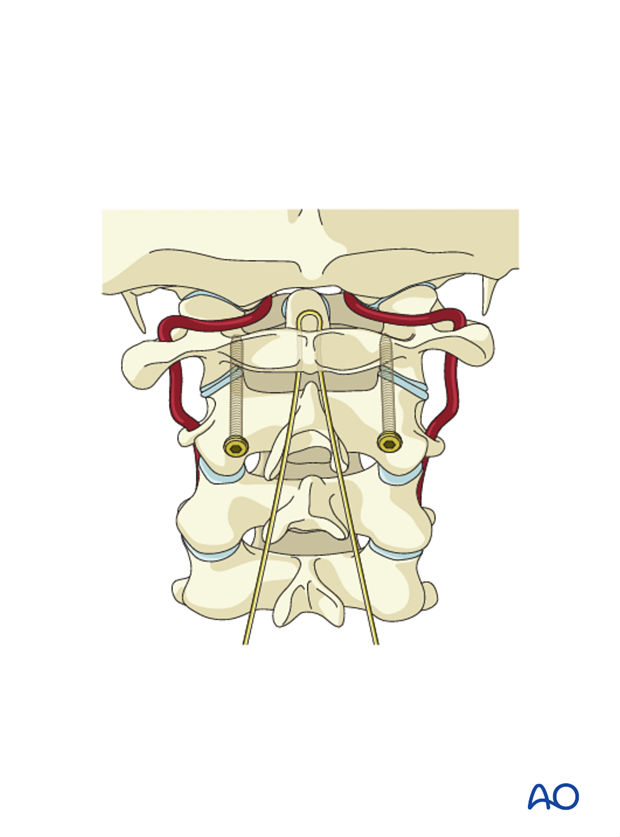
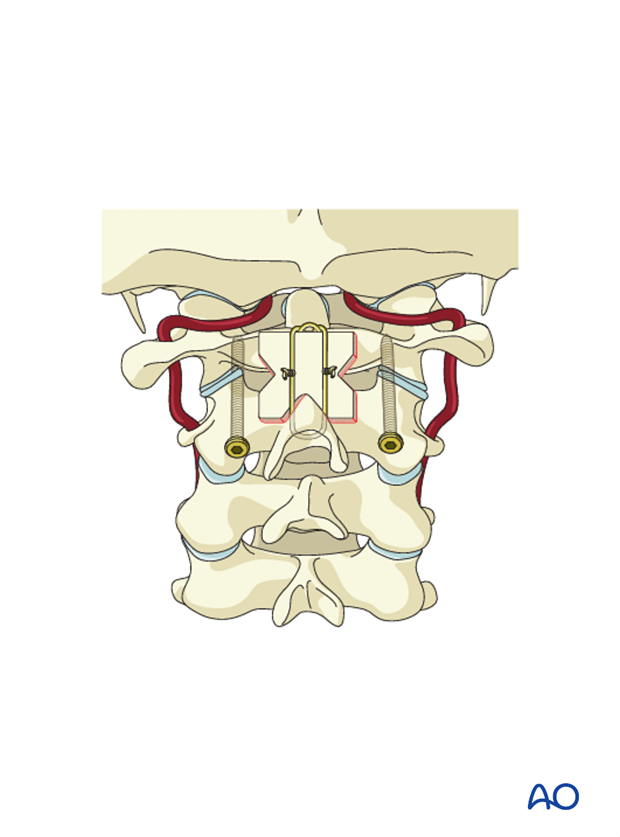
Fashion the bone graft as illustrated.
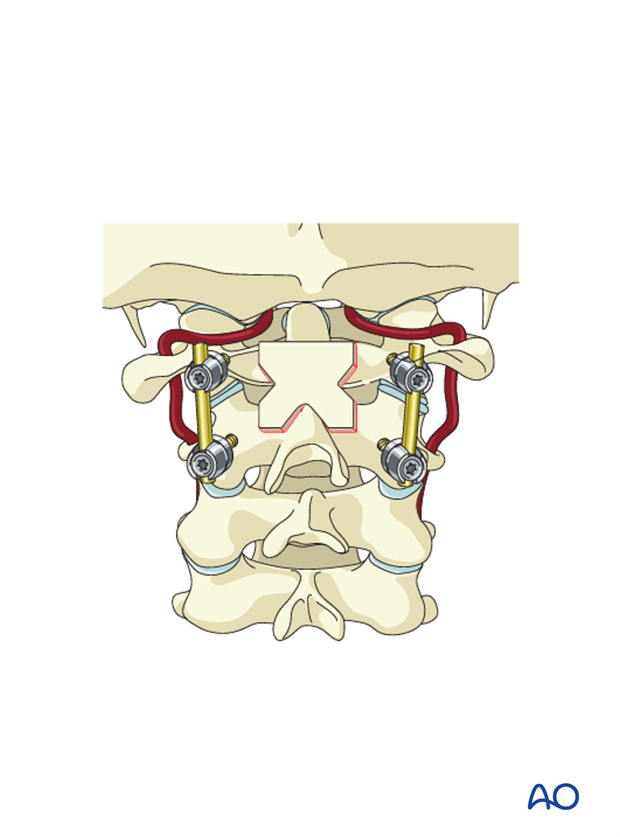
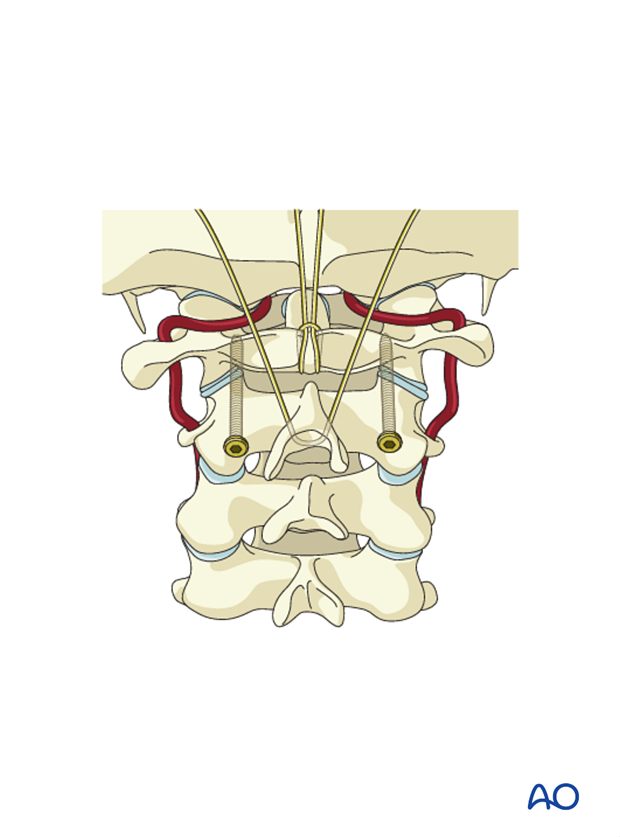
To keep the graft in place, a wire can be used around the rods.
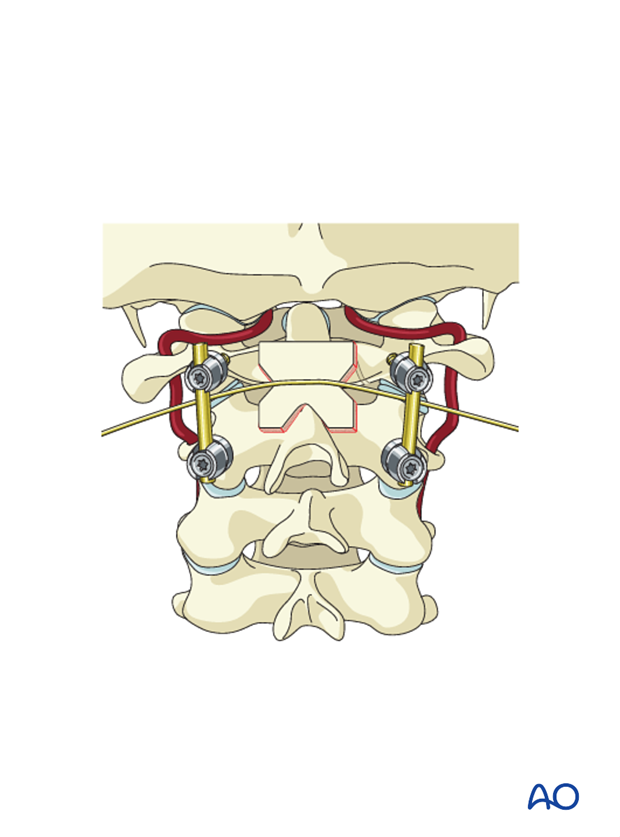
Add additional cancellous autograft strips to fill the voids between the lamina of C2 and the structural autograft.
Bone grafting following transarticular screw insertion (Magerl technique)
Since there are no rods, the graft is secured with wires. A loop of wire is passed under the arch of C1.
The two free ends are passed through this loop. A second wire is then passed through the spinous process of C2.
After decorticating the C1 posterior arch and the C2 lamina, the graft is placed, and the two wires are twisted together over the graft.
Additional cancellous autograft strips are added to fill the voids between the lamina of C2 and the structural autograft.
7. Aftercare
Patients are made to sit up in bed in the evening after the operation.
Patients with intact neurological status are made to stand and walk on the first day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.













