Compression plate and screw fixation
1. Principles
Displaced fractures of the greater trochanter are often not amendable to tension band wiring or cerclage cable fixation. This may be due to fracture complexity or extension into the proximal diaphysis. The goal of fixation is to create compression of the fracture site and allow for early mobilization.
2. Approach
Direct lateral approach extension
Direct lateral approach to the femoral diaphysis is typically utilized. This will require an extension to the proximal femur.
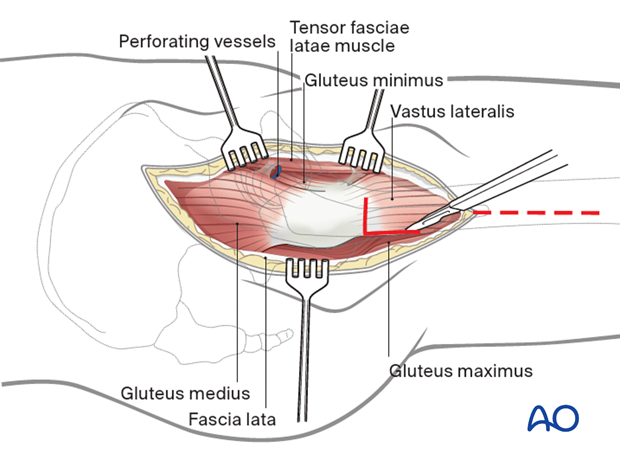
Option: Vastus lateralis origin release or split
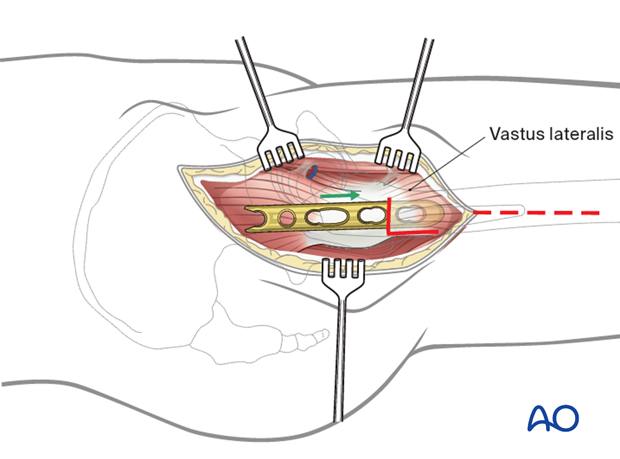
To apply a plate to the lateral aspect of the femur, the vastus lateralis origin can be released and this can be repaired after stabilization is obtained.
Alternatively, if the patient has a very large proximal femoral anatomy, the vastus lateralis origin may be split in its mid portion and the plate slipped below the muscle belly. This avoids the morbidity of a more complex tenotomy.
Other approaches
Other approaches that can be used to perform this procedure are:
- Anterolateral approach
- Direct anterior approach
- Iliofemoral (Smith-Petersen) approach
- Posterolateral approach
- Trochanteric osteotomy
These approaches can be performed with the patient in a lateral or supine position.
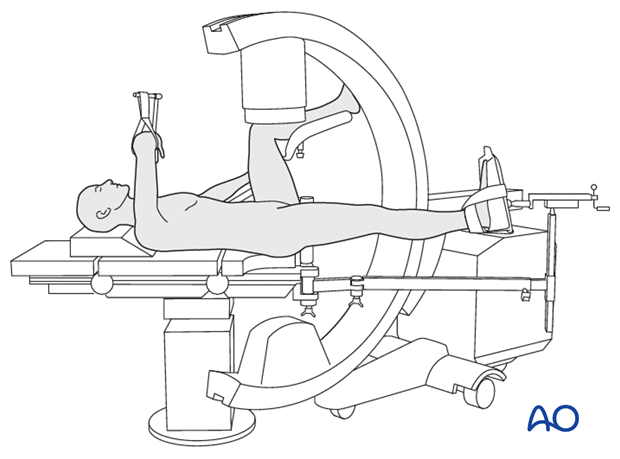
Option: use of a radiolucent or fracture specific table
A radiolucent table or a fracture specific table may be used.
3. Reduction
Direct reduction
Reduction is typically carried out using a combination of direct and indirect methods. Limb abduction will help in an indirect manner. Direct reduction with clearance of fracture hematoma and stabilization with pointed bone reduction clamps can then be completed.
The Collinear reduction clamp can be extremely helpful in facilitating reduction. It is applied from the direct lateral incision with proximal extension.
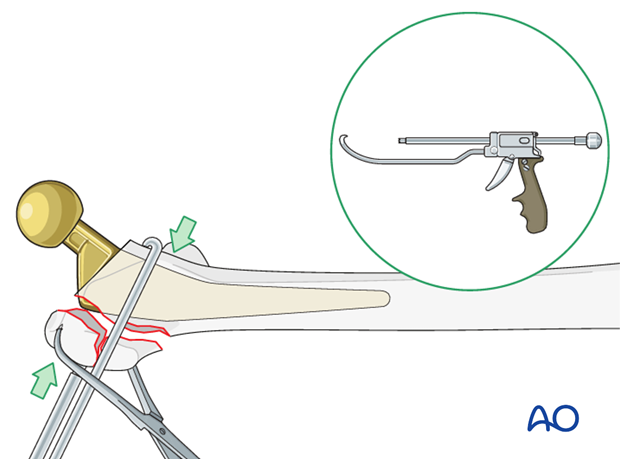
Option: reduction aid
Depending on the quality of the bone, utilizing a strong nonbioabsorbable stitch in a Krackow fashion into the gluteus medius tendon can help facilitate reduction.
This can be anchored either below the plate or in a tension band technique to the proximal femur.

4. Fixation
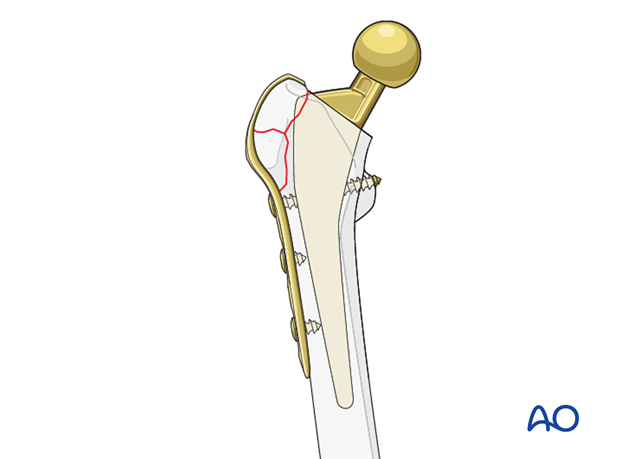
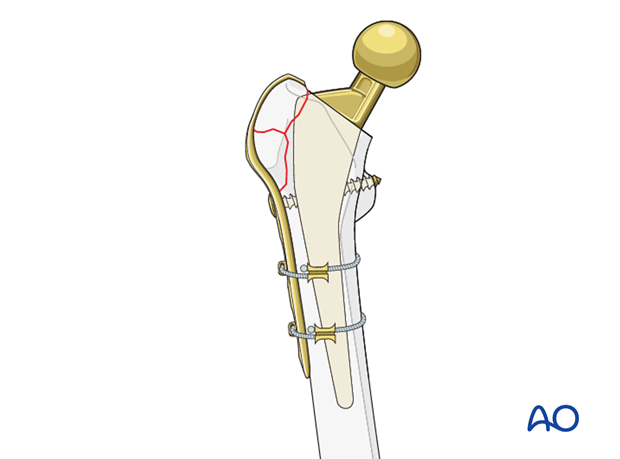
Implant selection
It is advantageous to utilize a plate construct that has a hook to wrap around the greater trochanter.
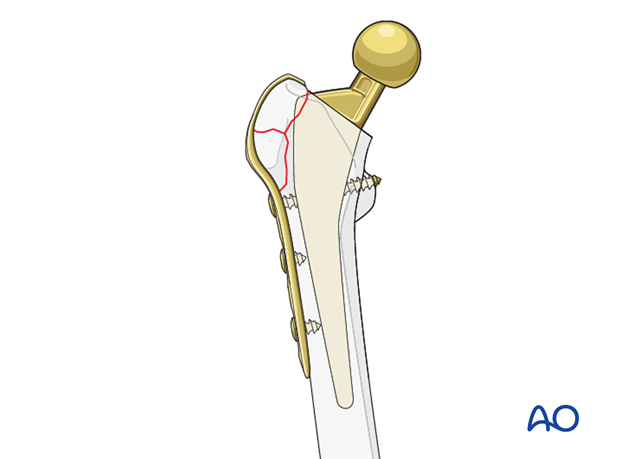
Plate application
Employing the dynamic compression feature of the plate will further engage the hooks in to the greater trochanter.
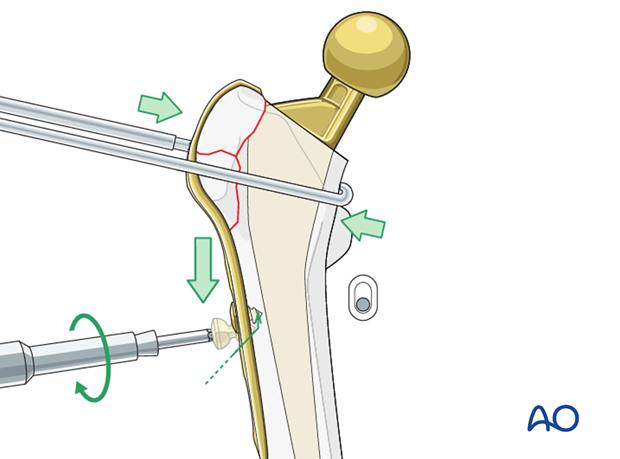
Screws may be inserted into the lesser trochanter and around the stem distally. It is frequently possible to insert bicortical screws posterior to the stem.
Alternatively, unicortical screws may be added to the construct.
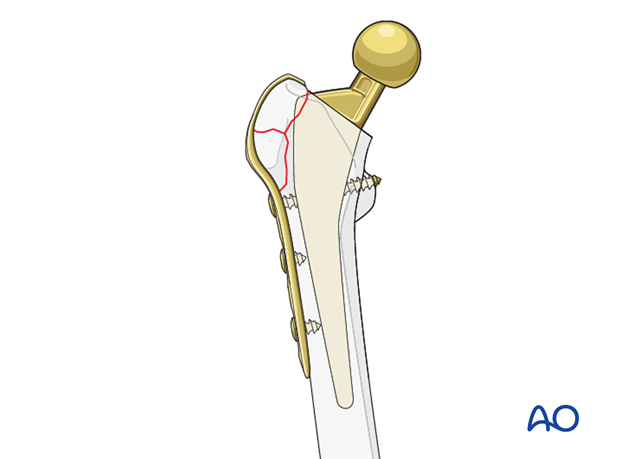
If the canal does not allow for adequate screw fixation, cerclage cables may be passed around the medial aspect of the femur and engaged in the plate laterally. For additional details on these implants please refer to adjunct plate options.
5. Closure
A layered closure is preferred for periprosthetic fractures. If the vastus lateralis has been released, it should be primarily repaired with a nonabsorbable braided stitch. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied and negative pressure incisional wound care can be considered.

6. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
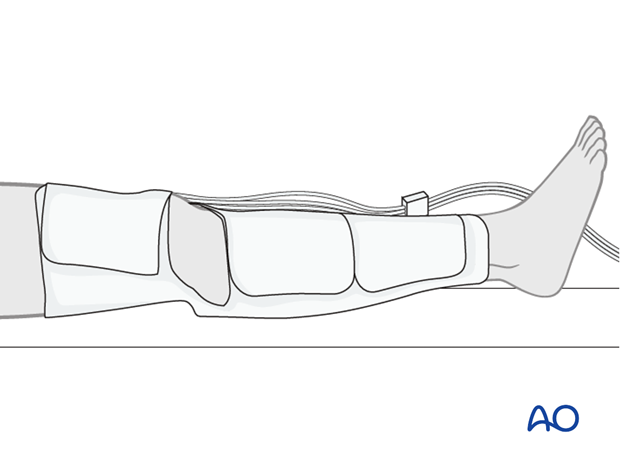
Activity limitations following greater trochanteric fracture treatment
If a greater trochanteric fracture has been treated, the patient should not be allowed to perform active abduction exercises until at least 6 weeks postoperatively. An abduction brace may be considered.
Traditionally, extended periods of limited weight bearing were utilized, however increasing stability of the fracture should be a priority to facilitate mobilization.
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.