ORIF (plate and screw) of posterior fractures with or without cup revision
1. Principles
Successful treatment of acetabular fractures noted intraoperatively is critical to achieve component ingrowth, pain control and long-term survivorship of the arthroplasty.
For further information about standard techniques for ORIF in native acetabular fractures, please refer to the acetabulum section of the AOSR.
2. Approach and extension for fracture visualization
The primary surgical approach may predict the fracture location:
- Direct anterior and anterolateral approaches are more commonly associated with anteriorly based fractures.
- Direct lateral and posterior approaches to the hip are more commonly associated with posterior type fractures.
- Medial wall fractures can be associated with any approach
In the setting of a posterior acetabular fracture, and the cup is unstable, the standard surgical approach should be enlarged to evaluate the posterior column and the posterior wall.
The patient can be in a lateral or supine position.
If extending the surgical approach does not allow adequate fracture evaluation, removal of the cup and direct visualization of the acetabulum is beneficial.

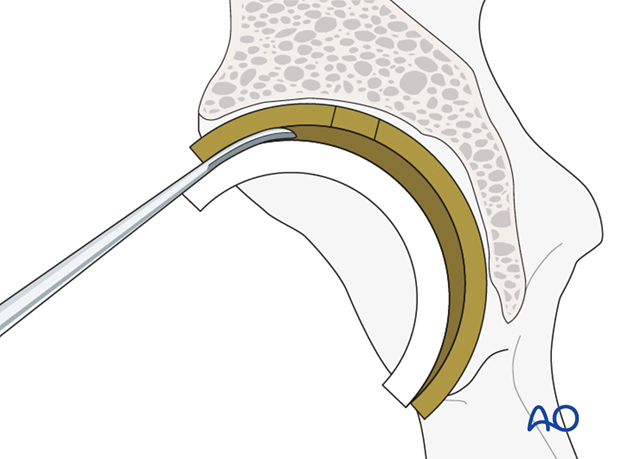
Posterior extension is achieved dissection outside the capsule of the hip onto the retroacetabular surface with placement of blunt, hand-held retractors into the greater sciatic notch.
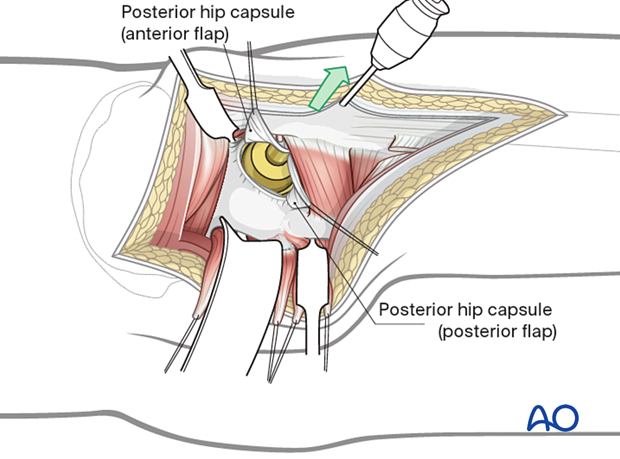
This is similar to a Kocher-Langenbeck approach; however, the short external rotators have typically been released at the level of the proximal femur. If a piriformis sparing approach has been utilized, but a fracture is suspected, the piriformis should be released to protect the sciatic nerve.
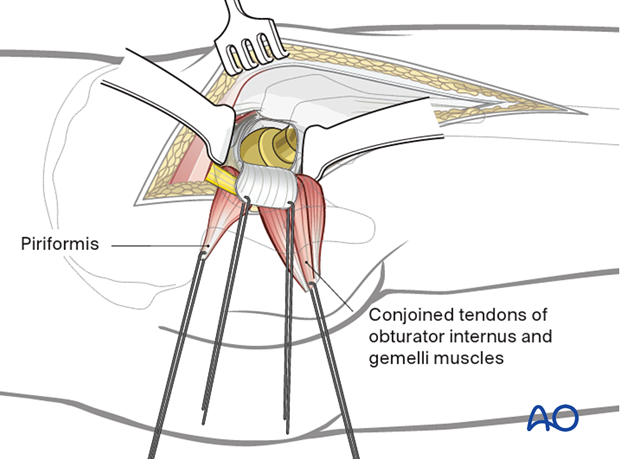
The hip should be extended past neutral, and the knee should be flexed greater than 60 degrees. This will allow fracture visualization.
The sciatic nerve is safely retracted with less tension.

3. Cup removal
In the setting of infection, loosening, or osteolysis, cup removal may lead to acute bone loss and/or the creation of periprosthetic fractures. If this destabilizes the acetabular support of the arthroplasty, fracture specific reduction and fixation techniques are necessary. Depending on the fracture pattern, ORIF with plate and screw and/or column fixation may be indicated.
It is critical to remove the cup without causing additional fractures or bone defects.
Liner removal
The cup liner is removed prior to cup removal.
Cup screw removal
Ensure that all the cup screws are removed prior to attempting to remove the cup itself.
Acetabular component removal
The acetabular component is removed. Details on how to remove an acetabular cup are described in the basic technique for acetabular cup removal.
4. Reduction and fixation of posterior fractures
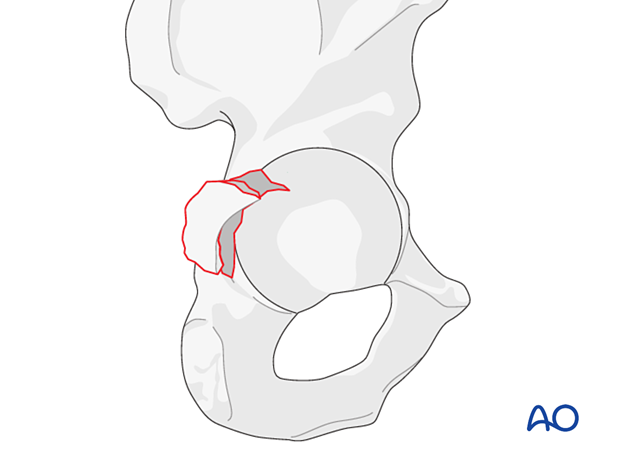
The surgeon should assess the location, stability, and extension of the fracture(s) by visual inspection. If available, intraoperative imaging may also be used.
Fracture reduction
In these fractures, anatomic reduction of the articular surface is not relevant. Columnar stability and wall containment are needed.
Posterior fractures can be treated as native fractures of the acetabulum with direct reduction of the cortical margin.
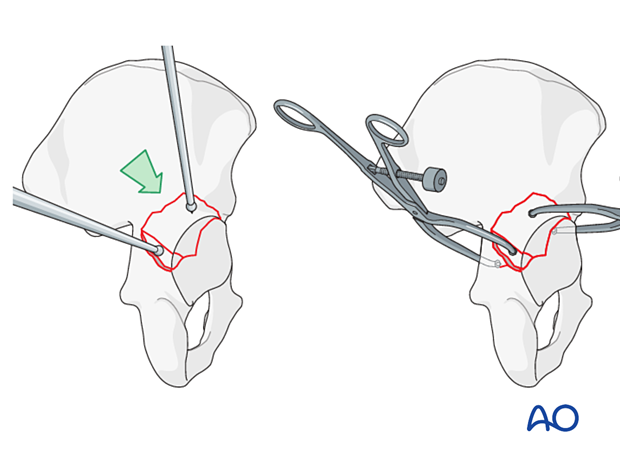
If there is a transverse fracture or a posterior column fracture, utilization of pelvic reduction clamps might be helpful.
Posterior wall fracture stabilization
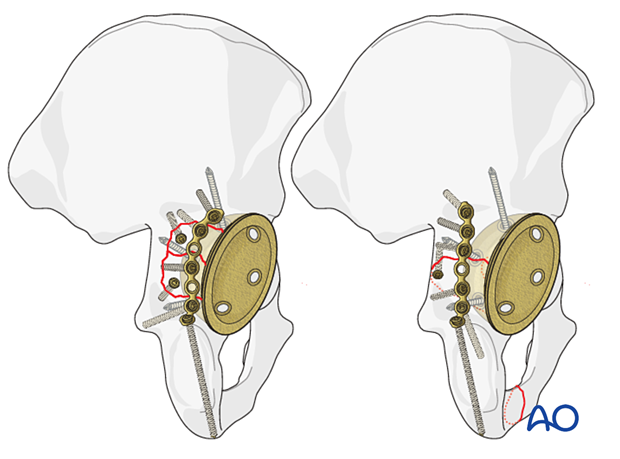
Posterior wall fractures should be stabilized in buttress mode with lag screw fixation when possible. Attention should be paid to maximal stability with minimal implants to avoid conflict between screws from the acetabular component and the fixation.
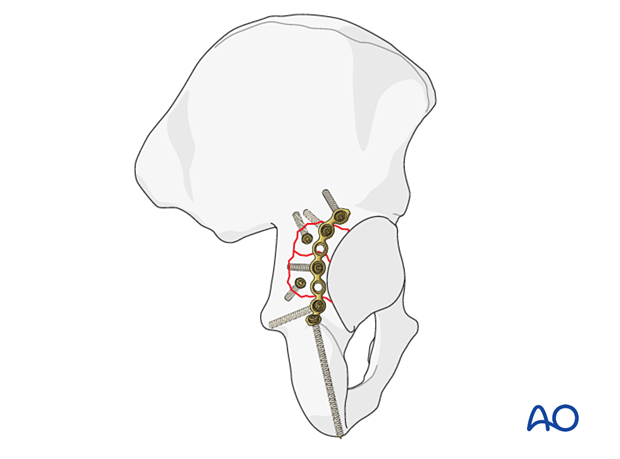
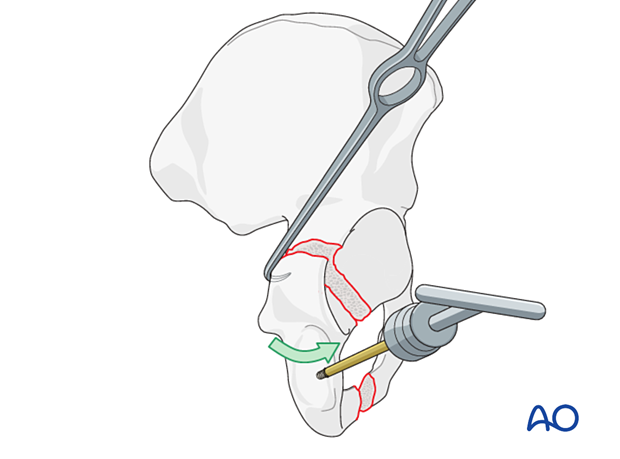
Posterior column fracture stabilization
Posterior column fractures can be stabilized utilizing intramedullary screws or compression with reconstruction plates as in native acetabular fractures.
Radiographic confirmation
Reduction and stabilization of the fracture should be confirmed using fluoroscopy.
5. New acetabular cup insertion
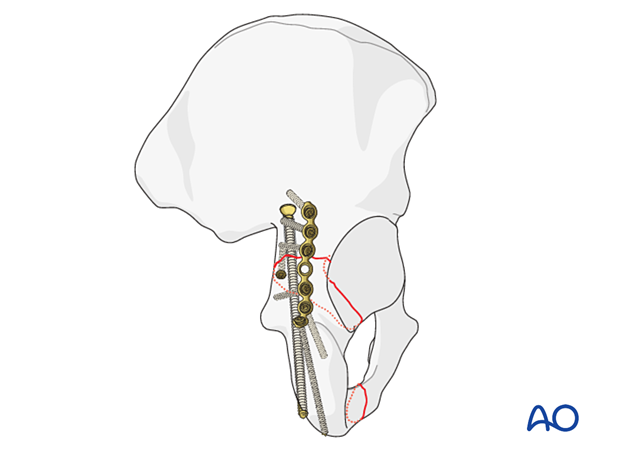
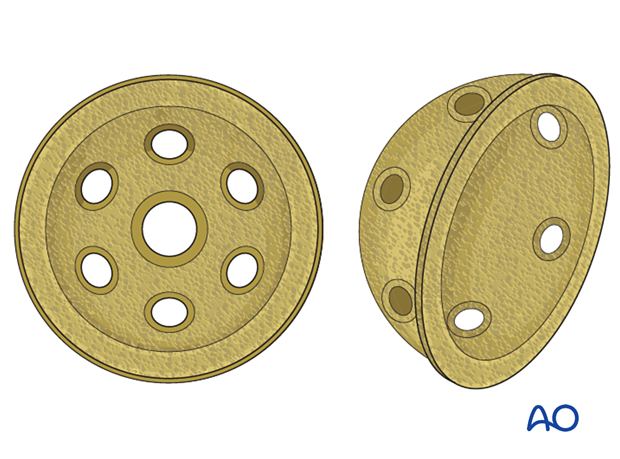
With the anatomy of the acetabulum restored, a standard multi-hole cup can be utilized.
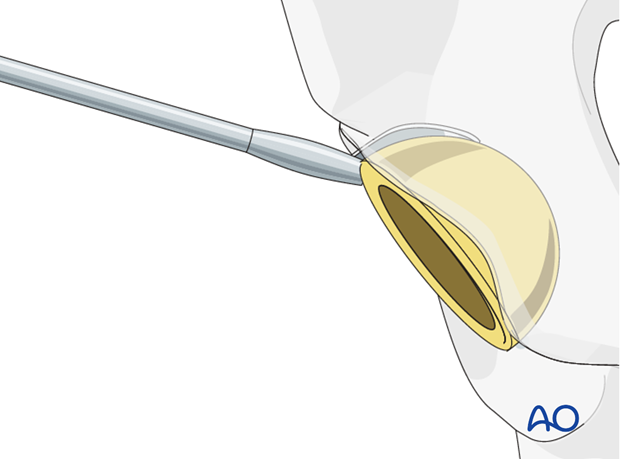
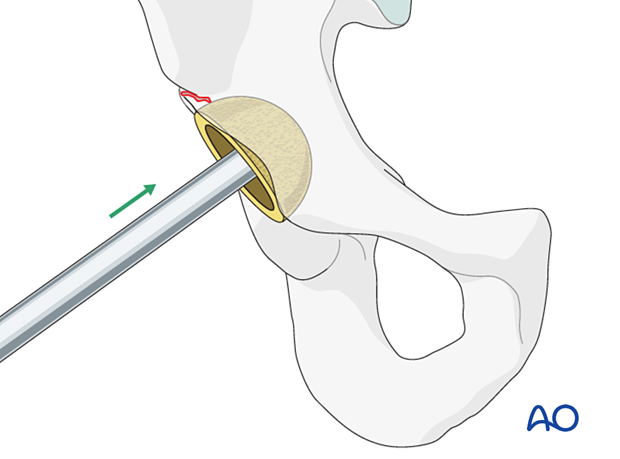
Acetabular reaming
The acetabulum should be reamed gently as not to compromise the reduction. The new cup can be implanted.

New cup positioning
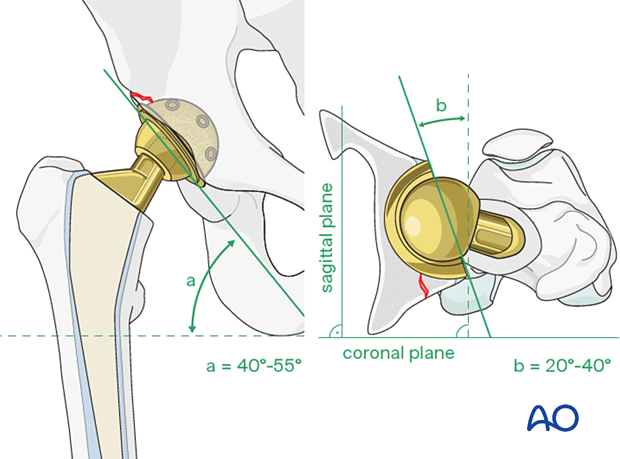
The surgeon should insert the new cup following the recommended position (inclination) and orientation (anteversion) guidelines.
The accepted "safe zone" is:
- cup inclination 40° to 55° (a)
- cup anteversion 20° to 40° (b)
New cup impaction
The appropriate cup is inserted using implant system specific instruments.
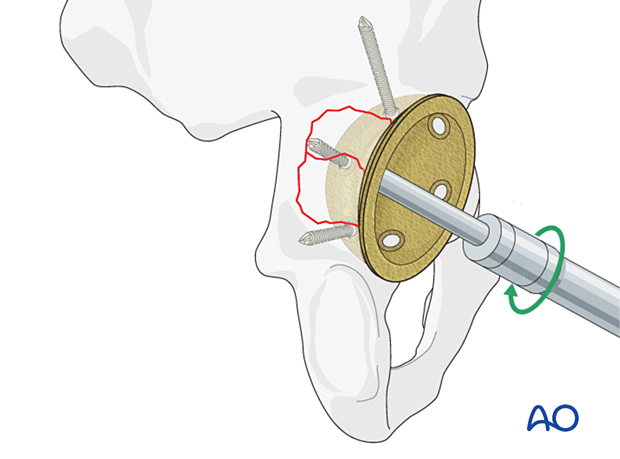
Cup screw fixation
The cup should achieve rim fit. Insert multiple screws in different planes to achieve stabilization to allow bony ingrowth.
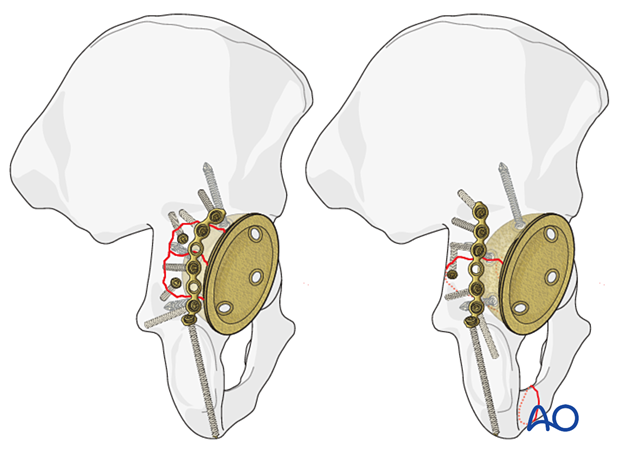
The screws, if possible, should span either side of the fracture. Any residual bony defects should undergo bone grafting with autograft or allograft, per surgeon's preference.
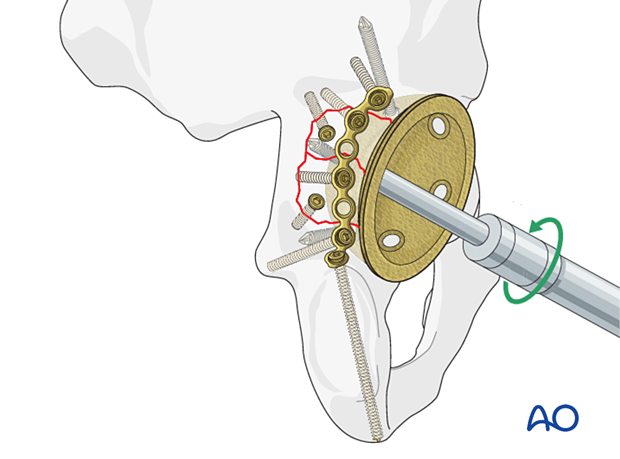
For further details about the multihole pressfit cup implantation please refer to the treatment: Revision of cup to multihole pressfit cup.
6. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
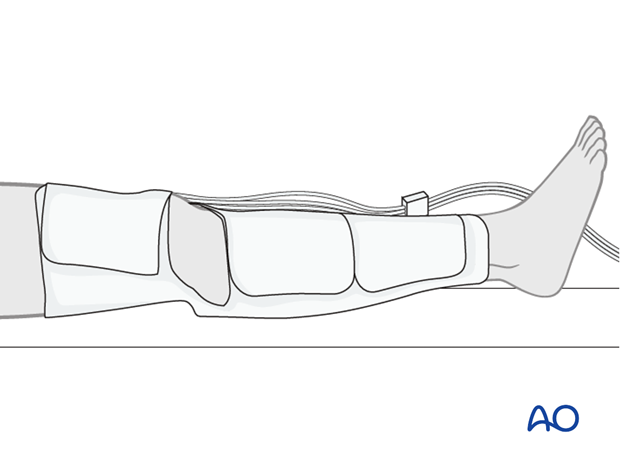
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
Precautions against hip dislocation
Hip precautions can be extremely important in patients who have suffered intraoperative acetabular fracture. Much work has been done to minimize the surgical exposure during hip arthroplasty to decrease the risk of dislocation. These advantages are typically removed when acetabular stabilization need to be performed. A dislocation in the postoperative course of such a patient can be disastrous.
Patients are instructed to follow standard hip precautions against dislocation based upon the surgical approaches for hip arthroplasty.
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.