Kocher-Langenbeck approach
1. Introduction
The Kocher-Langenbeck approach is an approach to the posterior structures of the acetabulum. It allows direct visualization of the posterior column and the retroacetabular surface. This approach can be useful for ORIF of periprosthetic acetabular, femoral fractures and revision arthroplasty.
The Kocher-Langenbeck approach can be performed either in the prone or lateral position. (The lateral position is preferred for periprosthetic fracture and revision arthroplasty).
The maintenance of knee flexion (at 90°) and hip extension throughout the procedure reduces tension on the sciatic nerve.
Scar tissue due to previous exposure might obscure typical landmarks.
Exposure
This approach allows direct access to the area indicated in dark brown, limited cranially by the neurovascular bundle.
Additional exposure to the cranial anterior portion of the acetabulum (blue) can be obtained with trochanteric osteotomy, which is not commonly performed in the setting of a previous arthroplasty.
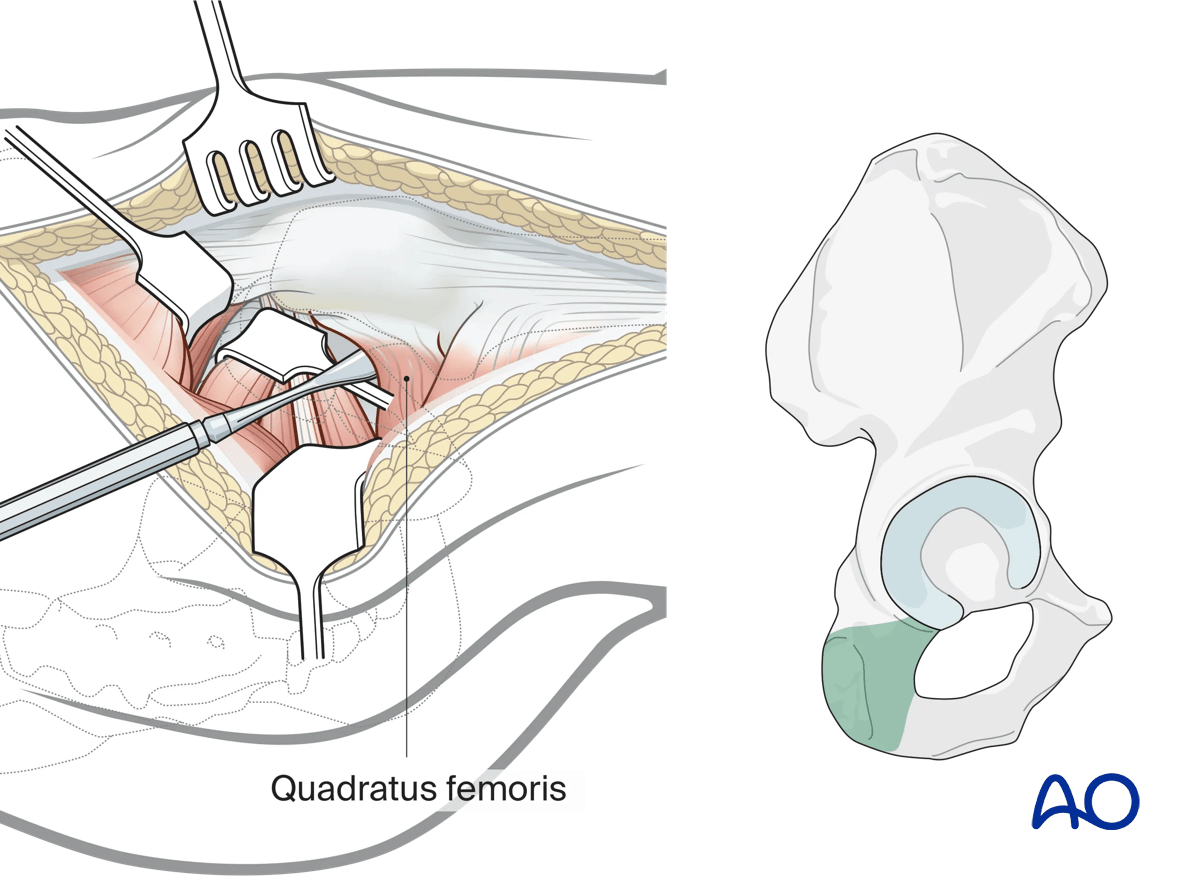
Caudal exposure (green) can be obtained with reflection of the quadratus femoris muscle.
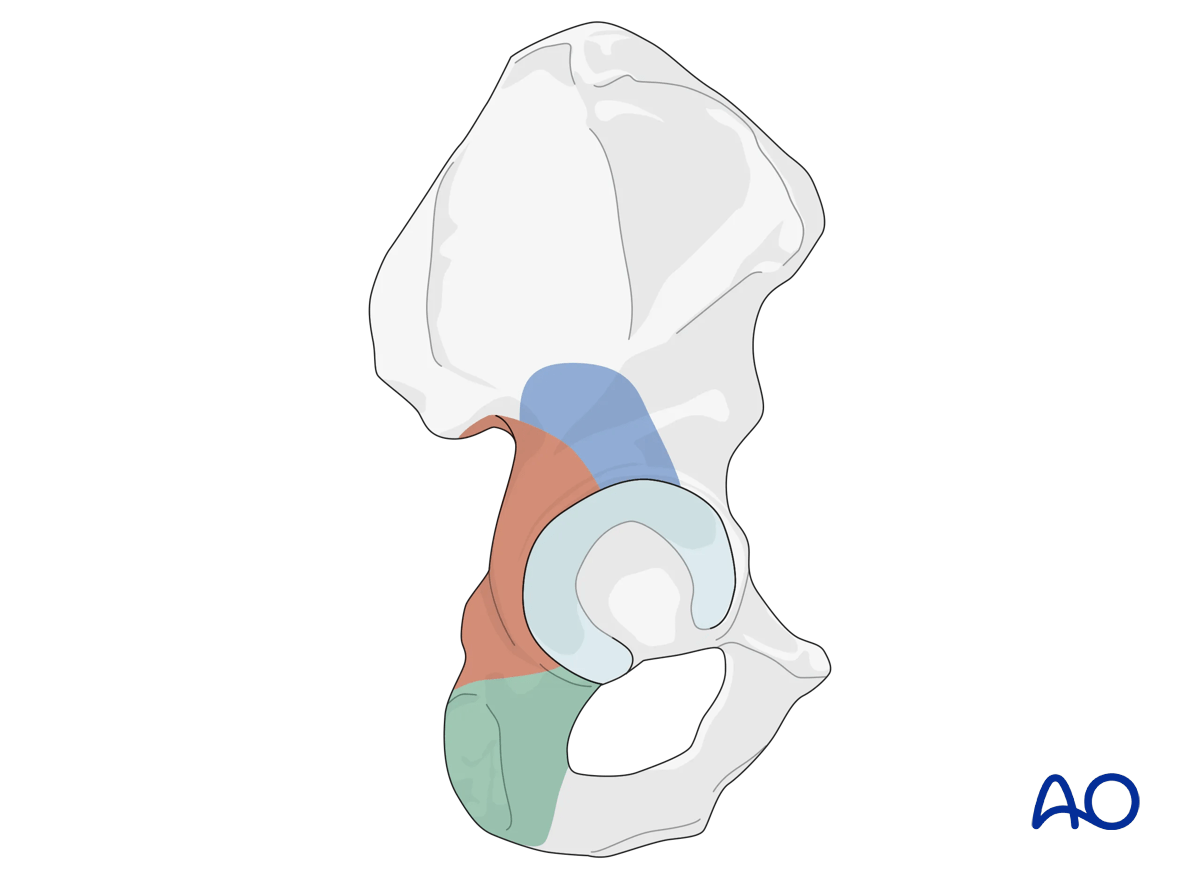
The area in light brown can be accessed by palpation and allows clamp placement.
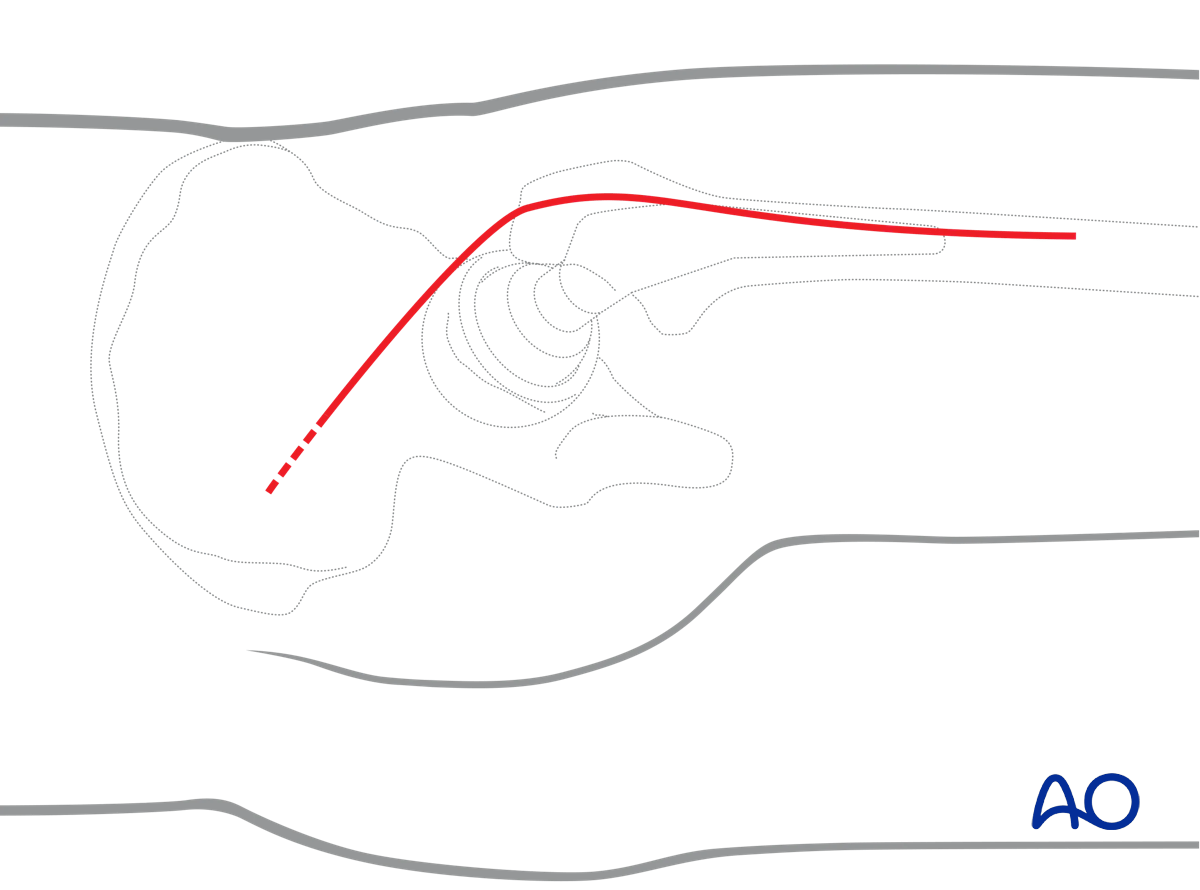
2. Skin incision
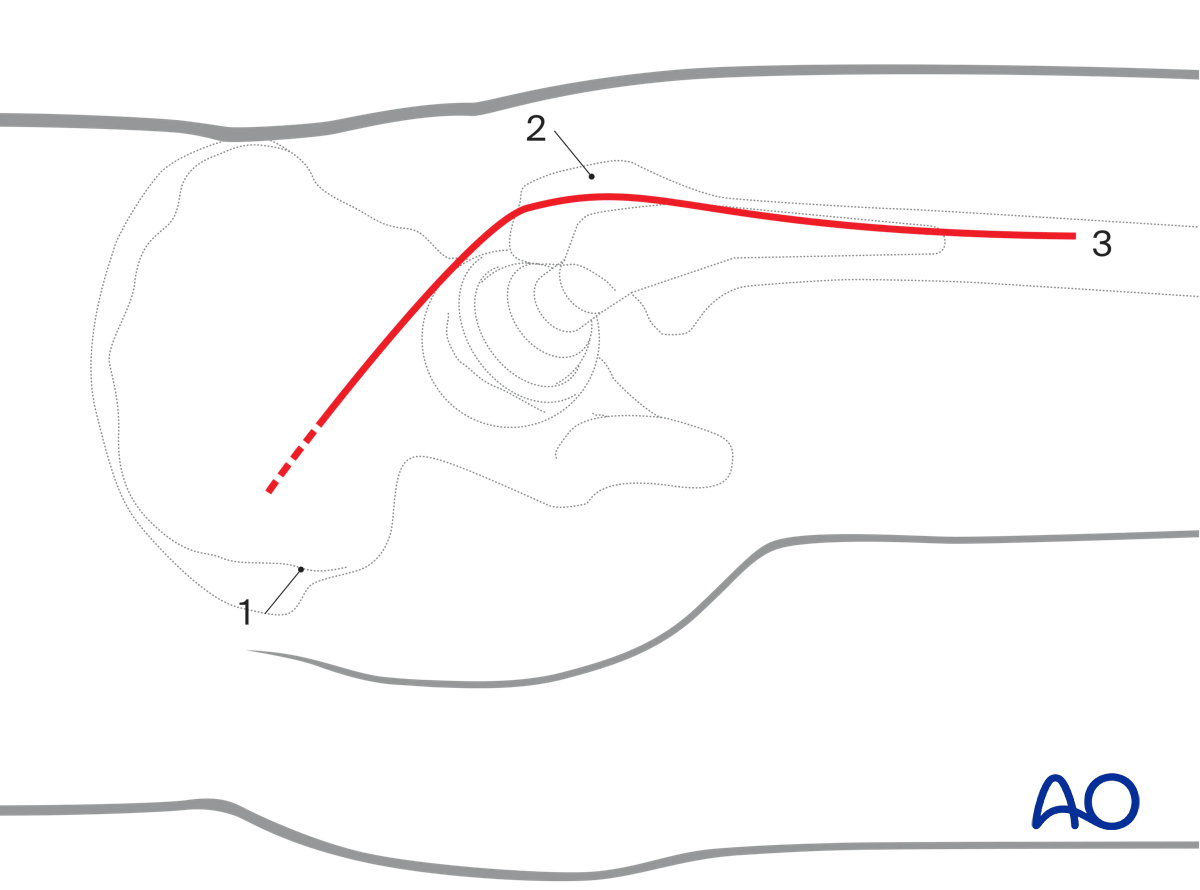
Outline the following bony landmarks with a sterile marking pen:
- Posterior superior iliac spine
- Greater trochanter
- Shaft of femur
Start the skin incision a few centimeters distal and lateral to the posterior superior iliac spine. A more proximal extension (indicated by dashed line) may improve exposure in obese or muscular patients.
Continue the incision anteriorly over the greater trochanter. Curve it distally along the tip of the greater trochanter towards the lateral aspect of the femoral shaft.
End the incision at the mid third of the thigh (just distal to the insertion of the gluteus maximus tendon).
3. Superficial surgical dissection
Fascial incision
After dividing the subcutaneous tissues, sharply incise the subcutaneous tissues along:
- The gluteus maximus muscle (using scissors)
- The iliotibial tract (using a scalpel)
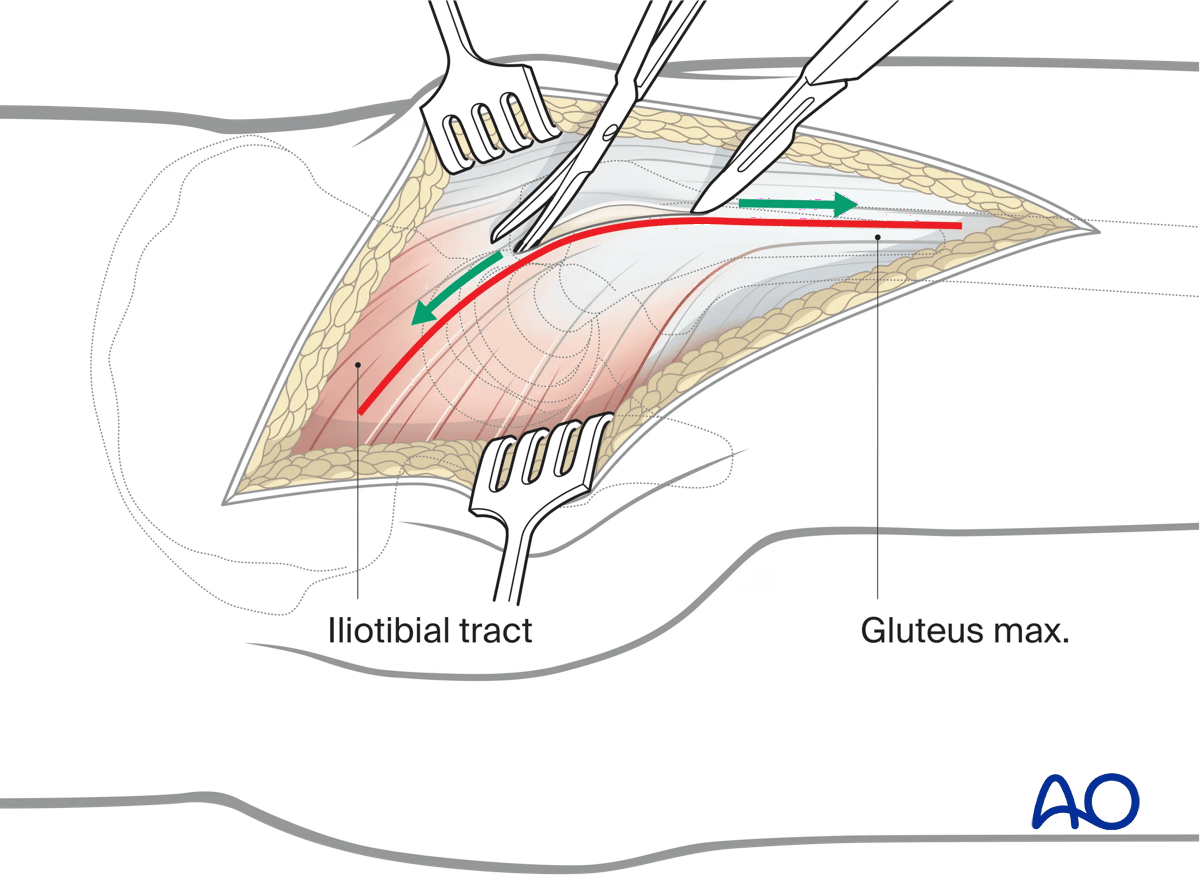
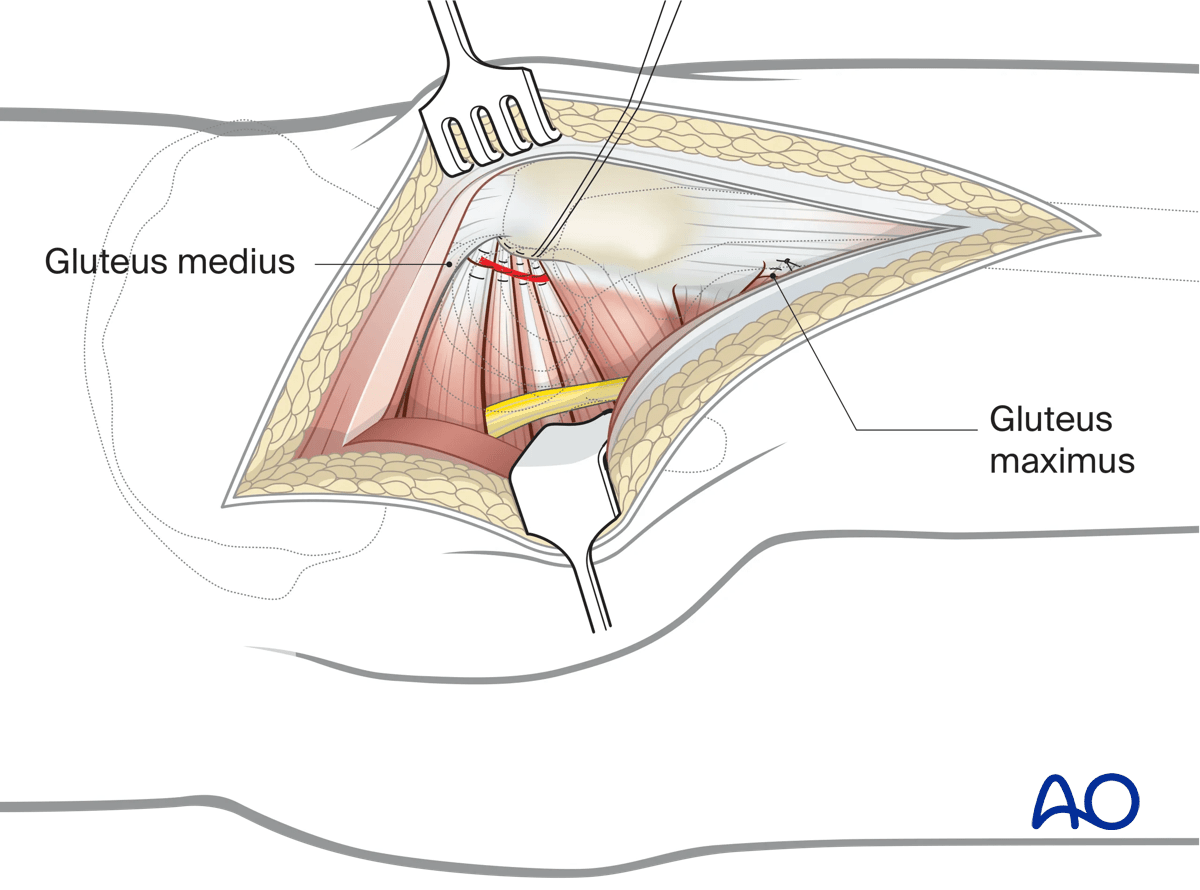
Split the gluteus maximus and incise the iliotibial tract
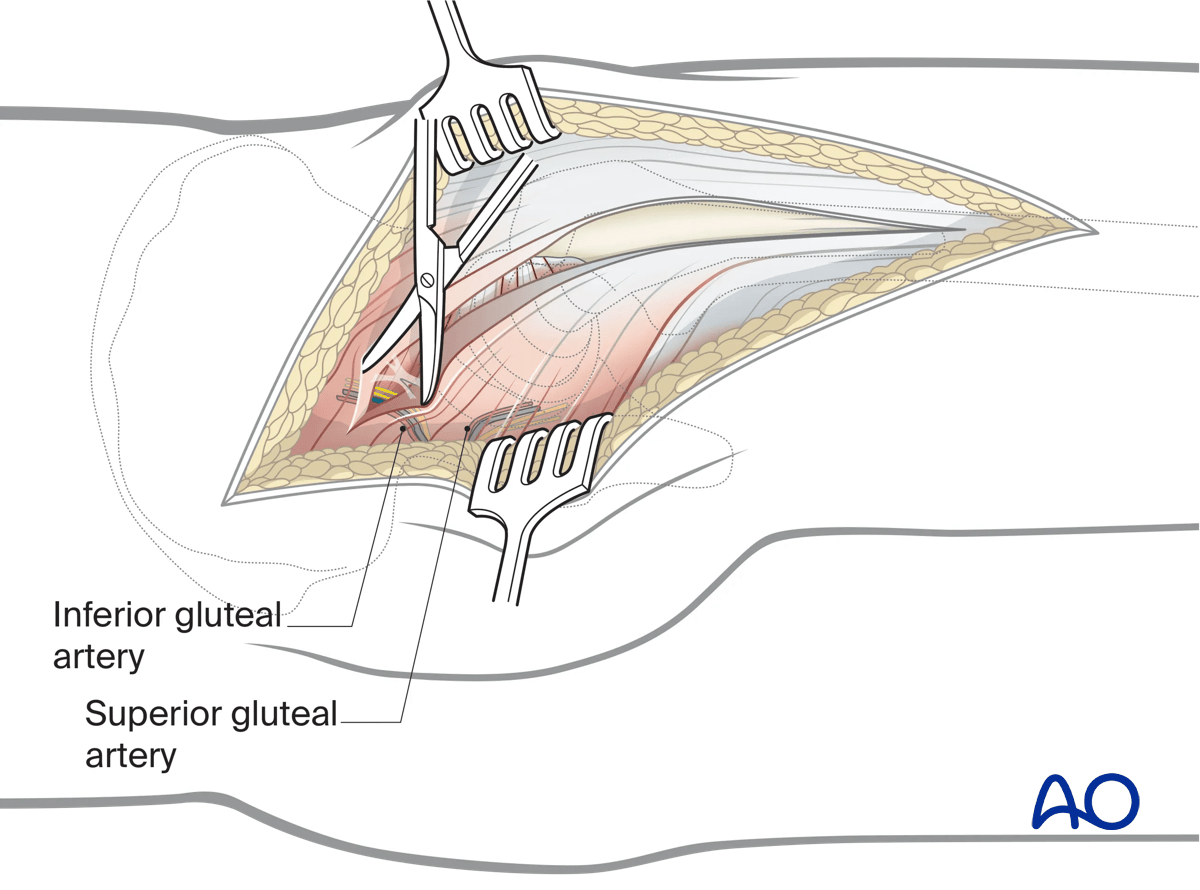
Split the gluteus maximus in line with its fibers, starting at the greater trochanter in a proximal direction up to the crossing of the first neurovascular bundle.
This creates a posterior muscle belly (inferior gluteal artery), and an anterior belly (superior gluteal artery) that includes one third of the gluteus maximus and the muscle of the tensor fascia latae.
In the distal half, incise the iliotibial tract in line with its fibers up to the mid third of the thigh.
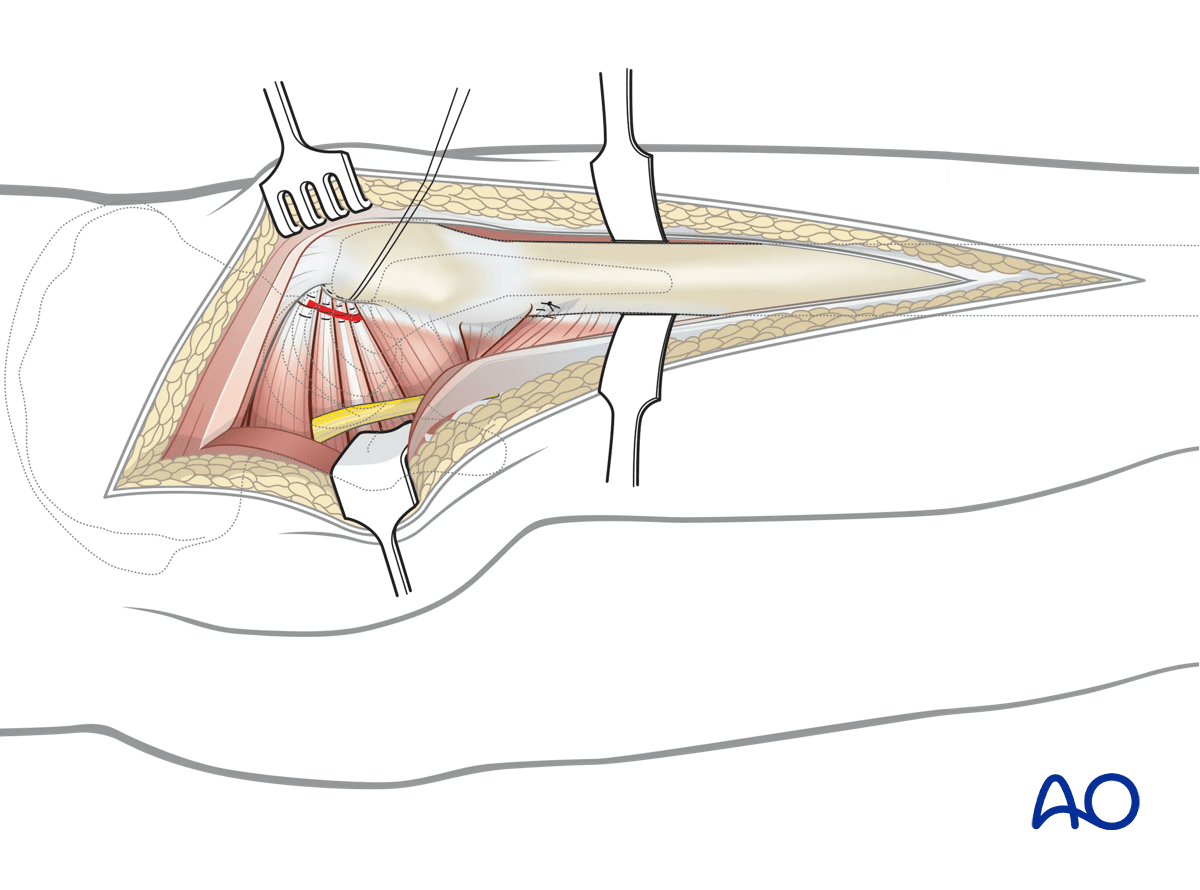
4. Deep dissection
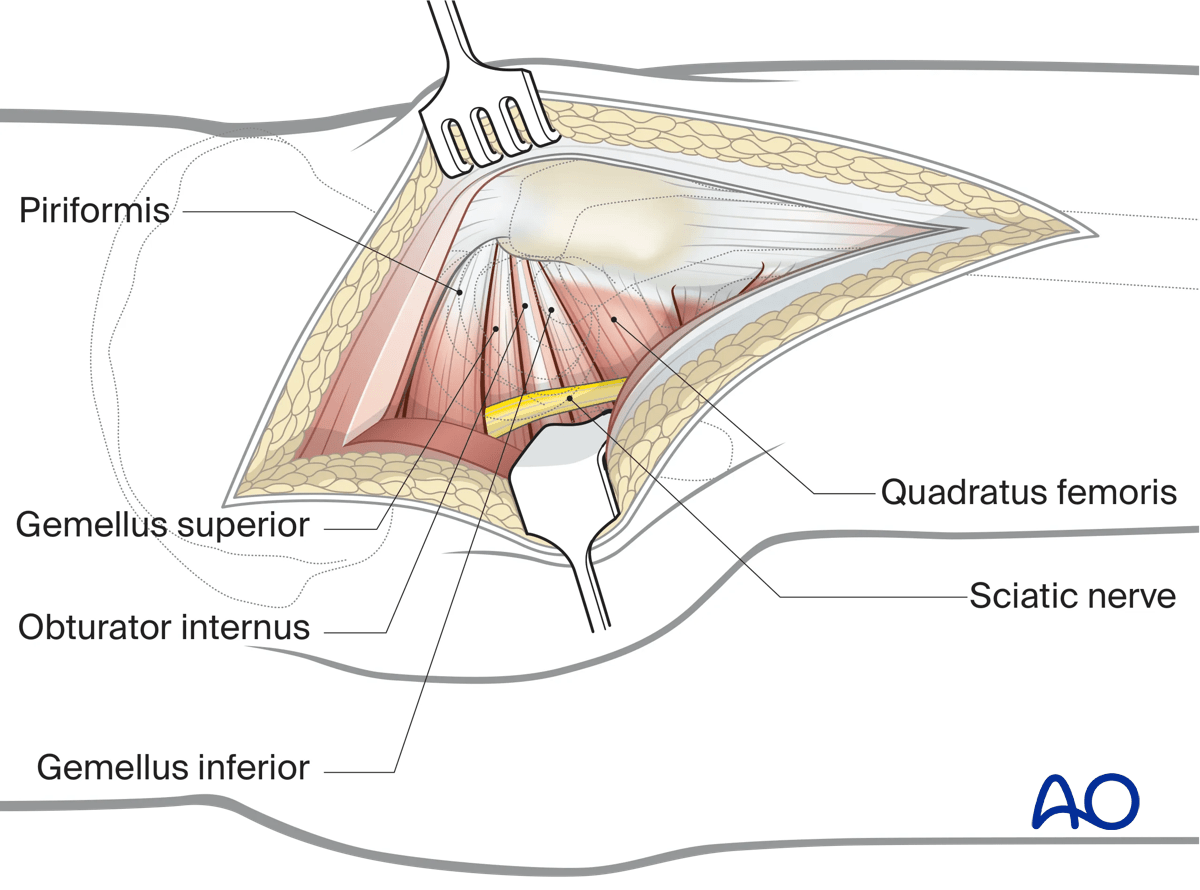
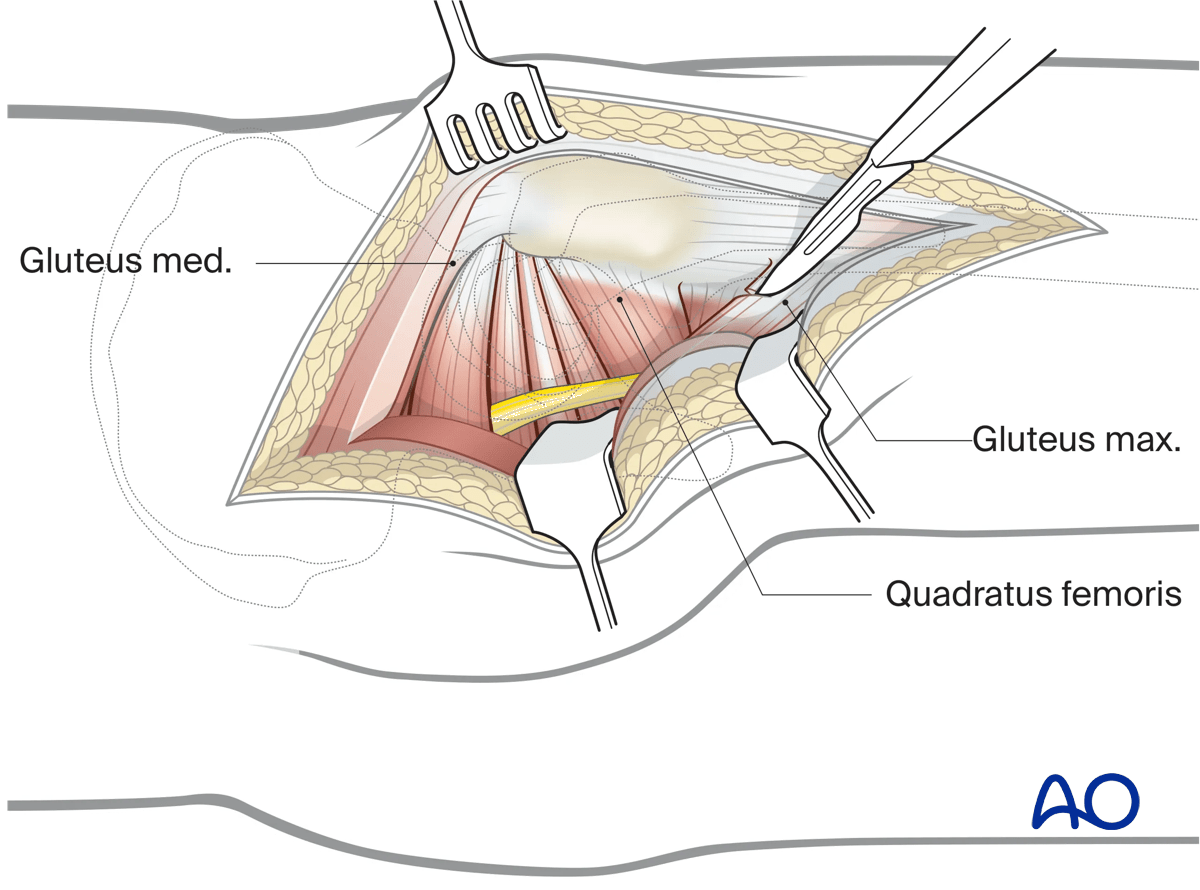
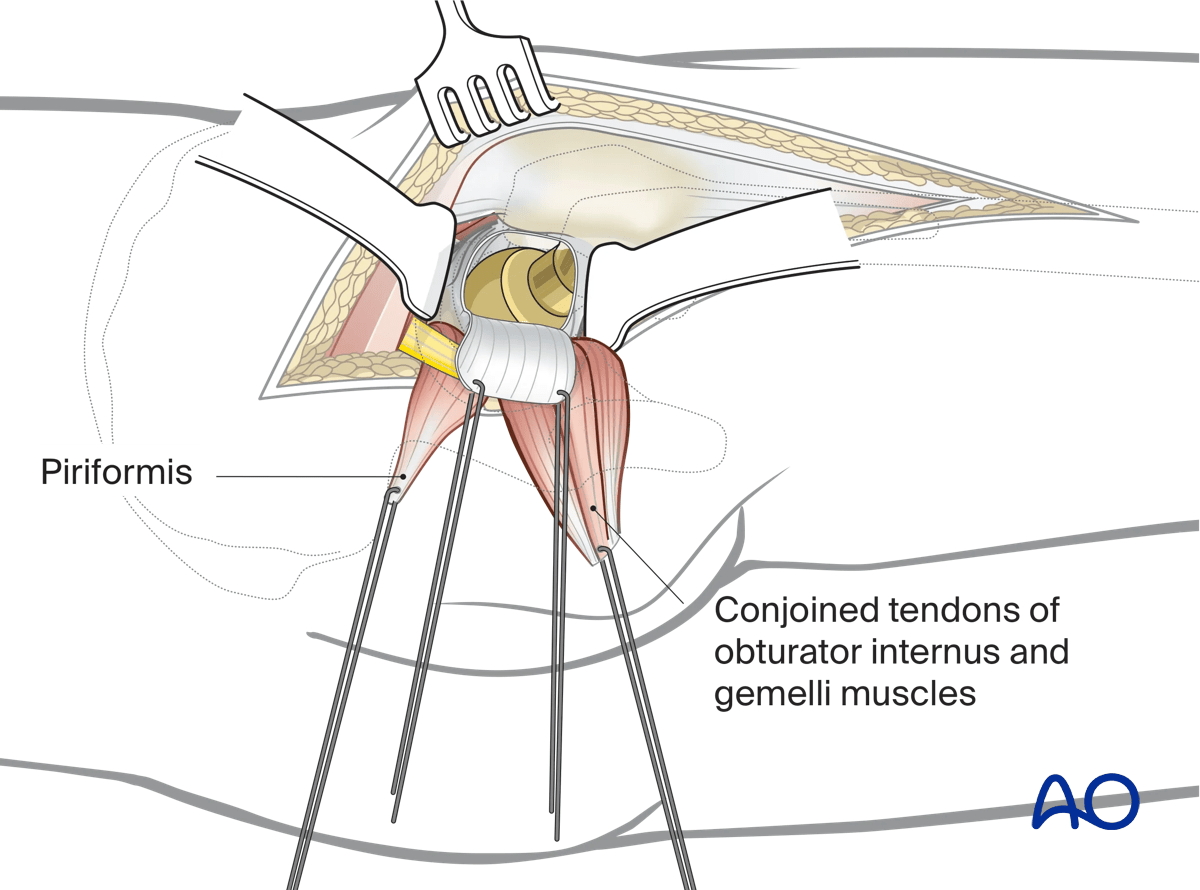
Free the layer of fat covering the short external rotators, exposing the insertion of the piriformis tendon, the gemelli, and the internal obturator muscle.
The sciatic nerve (see illustration) lies posterior to the gemelli and internal obturator muscles, and anterior to the piriformis muscle, between the greater trochanter and the ischial tuberosity.
Carefully visualize the sciatic nerve.
Ensure at all times that no direct pressure or stretching is exerted on the nerve.
Option: detach the gluteus maximus muscle
Detach the gluteus maximus 1 cm from its insertion into the gluteal tuberosity of the femur.
Detachment can be done partially or completely.
This allows less tension and easier mobilization of the gluteus maximus muscle.
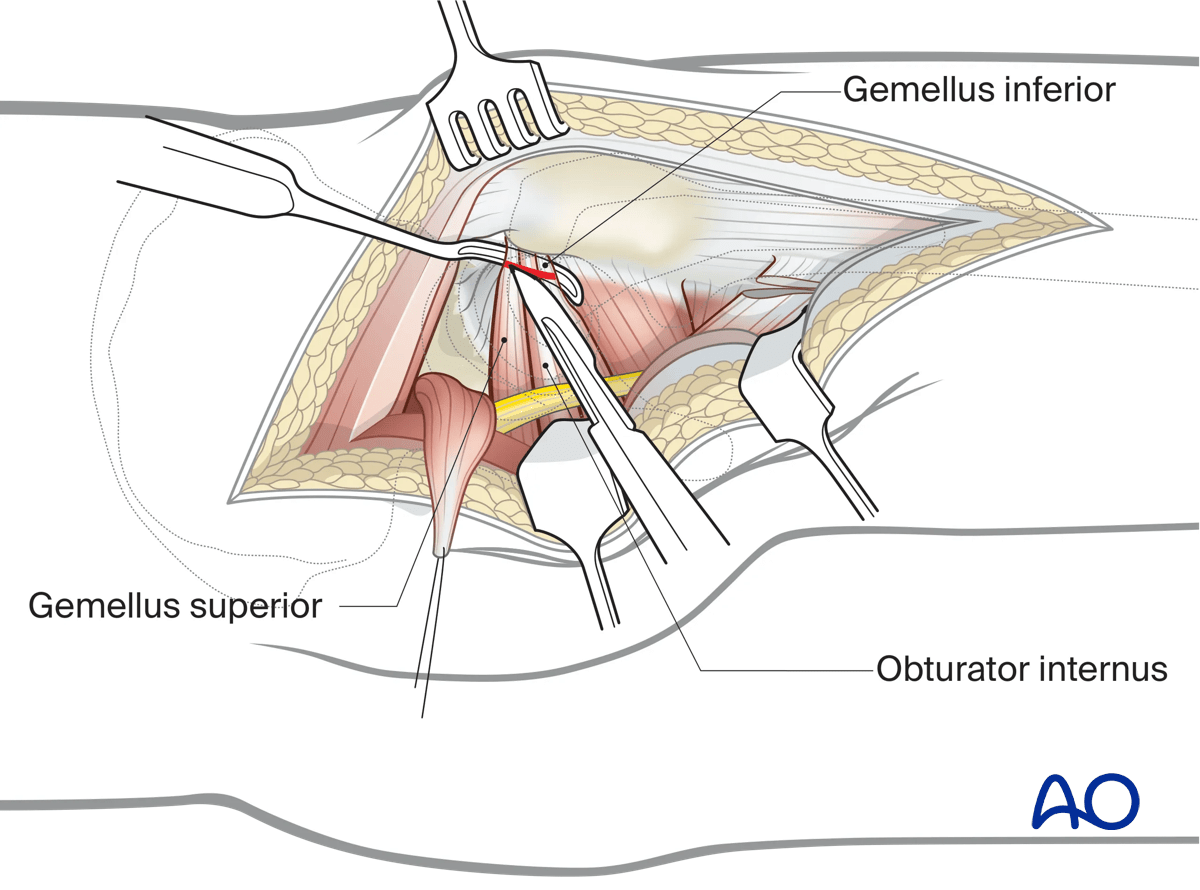
Detach the external rotator muscles
Before dividing the tendons, place heavy, nonabsorbable stay sutures for retraction and subsequent repair. One suture can be placed in the piriformis tendon, and the other in the conjoined tendons of obturator internus and gemelli. Reflection of the short rotator muscles exposes the hip capsule.
Reflect the piriformis belly laterally to expose the retroacetabular surface to the greater sciatic notch.
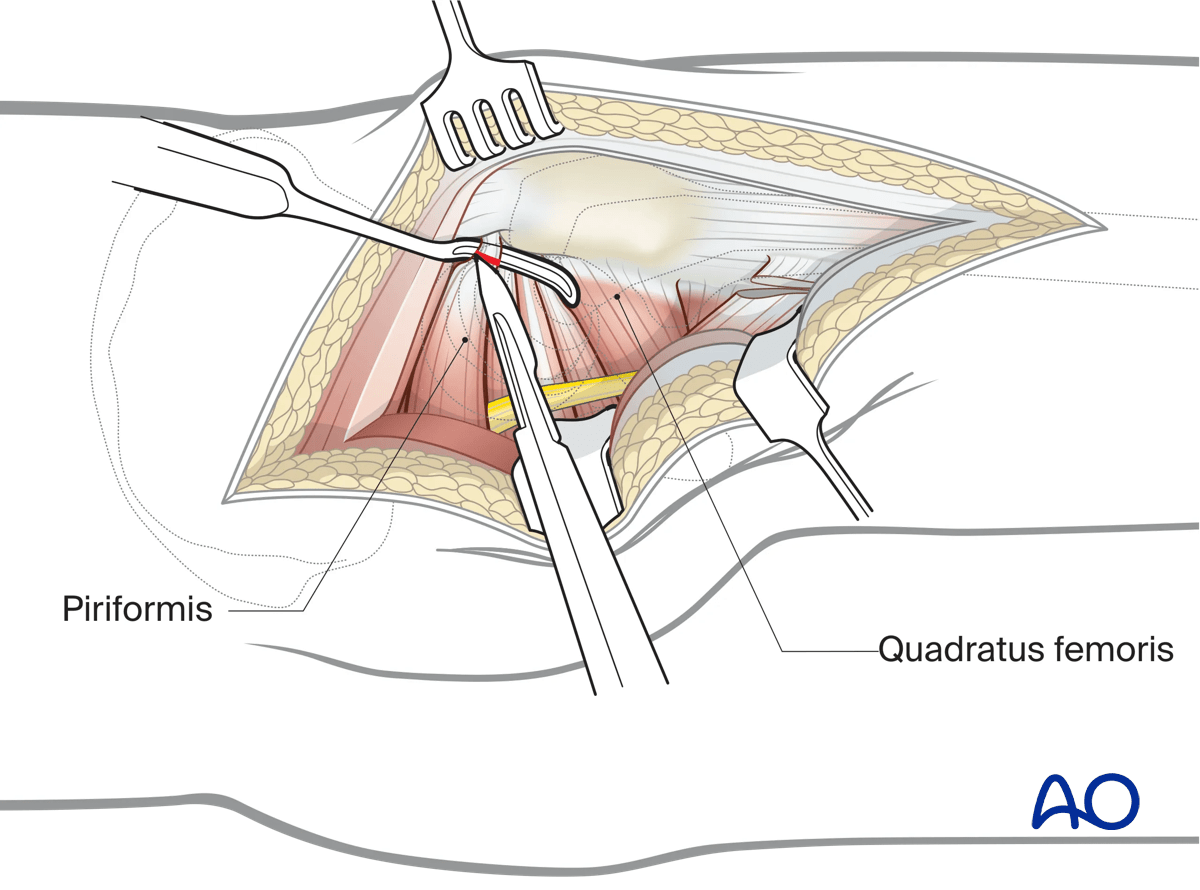
Reflect the muscle bellies of the three conjoined muscles laterally to access the lesser sciatic notch.
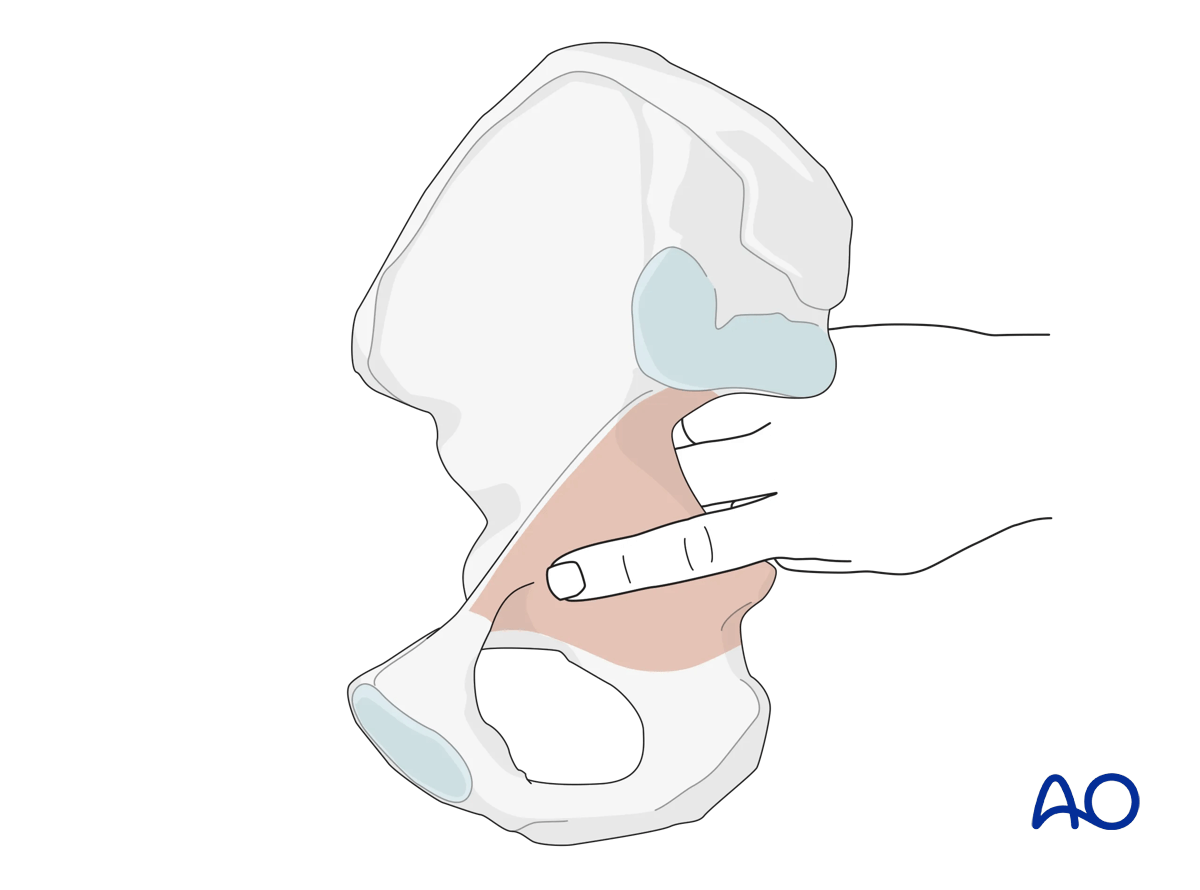
5. Exposure of the posterior wall and column
Expose the greater sciatic notch, the ischial spine, and the lesser sciatic notch.
Insert a retractor in the lesser sciatic notch and one anterosuperiorly in the direction of the anterior inferior spine. Now the posterior column is visible in its whole extent.
Protect the sciatic nerve, which lies behind the retractor, with abdominal sponges. Use the short external rotator muscles as a cushion.
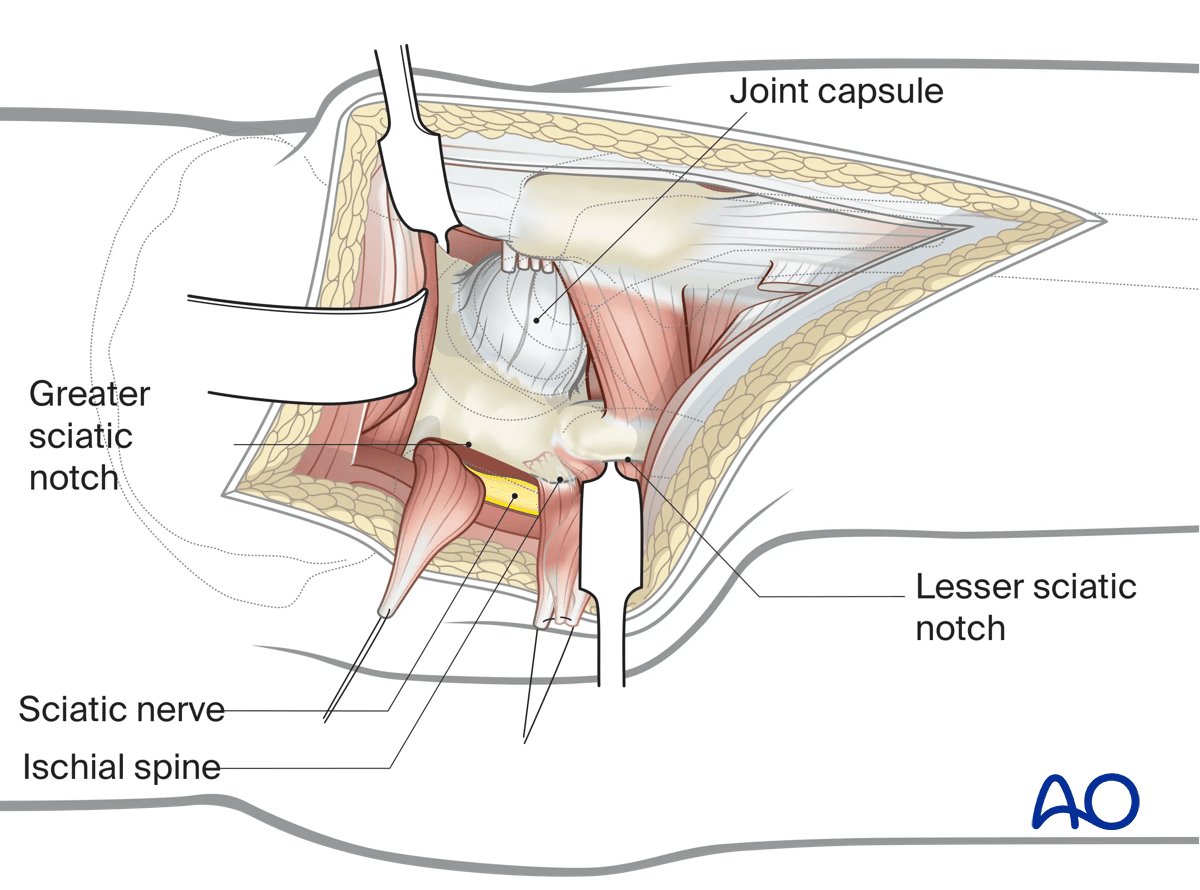
6. Quadratus femoris elevation for additional caudal exposure
The quadratus femoris can be elevated from its origin to expose the distal extent of the posterior column as demonstrated in green.
7. Hip exposure
Expose the hip joint by creating and reflecting a full thickness, broad-based flap through the posterior hip capsule. Heavy (e.g. #2) non-absorbable sutures can be used to tag the capsule to aid in retraction and subsequent repair.
8. Wound closure
Perform a meticulous debridement of all soft tissues before starting wound closure.
Remove necrotic tissue and irrigate the entire wound to decrease the risk of periarticular ossification.
At the completion of the procedure, the posterior capsular flap sutures, and then the tendon sutures, are tied to each other after being passed through drill holes in the posterior greater trochanter. Quadratus femoris, if divided, is repaired separately.
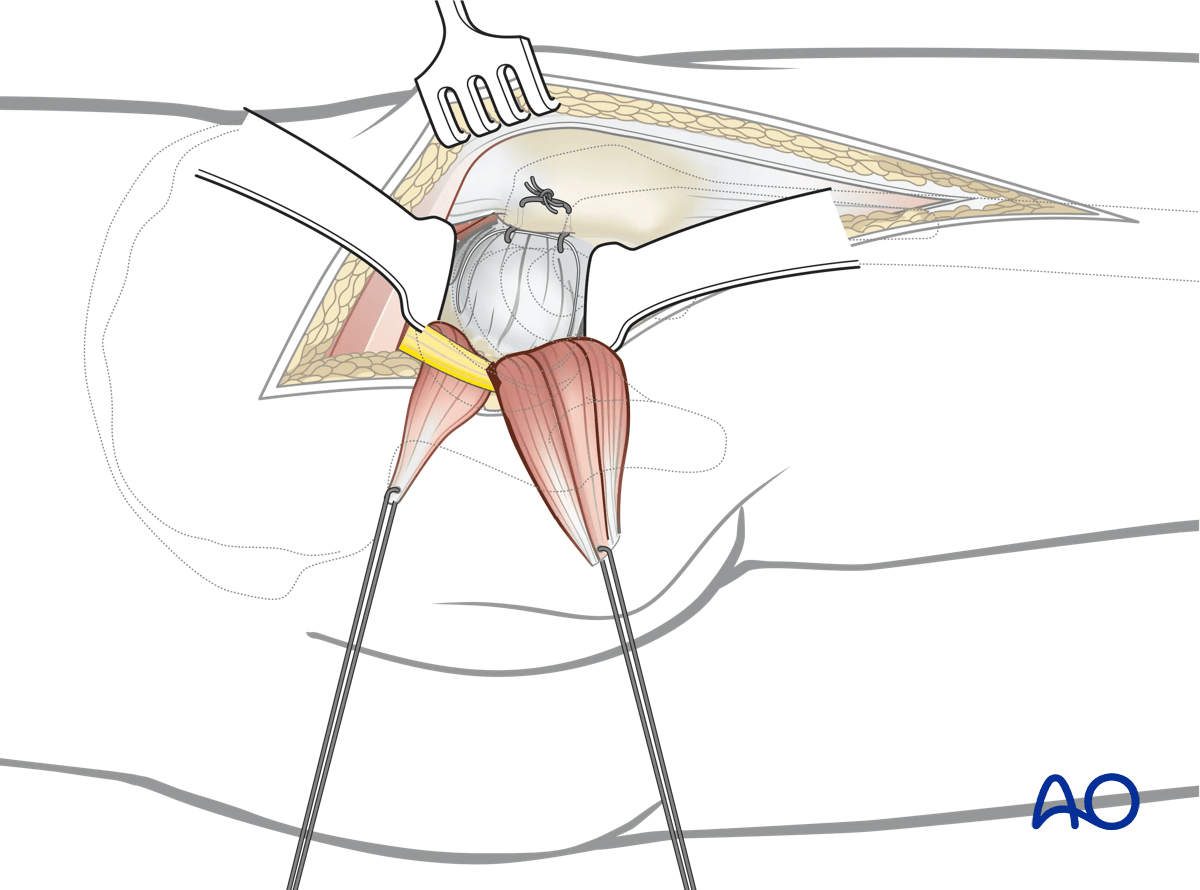
A secure repair of the tendons and capsule decreases the risk of hip prosthesis dislocation after a posterior approach.
(See also:Pellicci PM et al.(2009) MRI shows biologic restoration of posterior soft tissue repairs after THA Clin Orthop Relat Res.April; 467(4): 940–945.)
Approximate the split parts of the gluteus maximus with adaptation sutures. Perform the closure of the iliotibial tract, the subcutis, and the skin.
9. Possible extensions
This approach can be extended distally into a lateral approach to the femur if needed.