Isolated cerclage
1. Principles
In the setting of a stable femoral prosthesis, the goals include pain control, fracture healing, and maintaining a stable hip prosthesis.
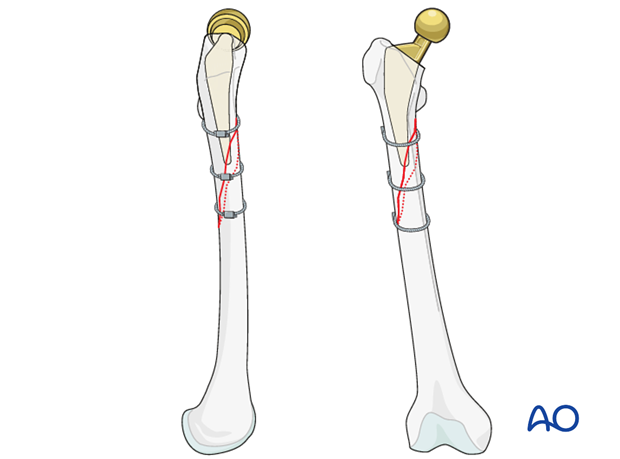
This is typical of proximal fit prostheses that present spiral and/or short oblique minimally displaced fracture patterns, that can undergo direct reduction and compressive fixation with isolated cerclage.
2. Approach
Direct lateral approach
Direct lateral approach to the femoral diaphysis is typically utilized. This can be performed in a minimally invasive fashion for some fracture patterns and proximal and/or distal extension of deep surgical approach can be utilized in a fracture specific manner.

Other approaches
Other approaches that can be used to perform this procedure are:
- Anterolateral approach
- Direct anterior approach
- Iliofemoral (Smith-Petersen) approach
- Posterolateral approach
- Trochanteric osteotomy
These approaches can be performed with the patient in a lateral or supine position.
3. Reduction
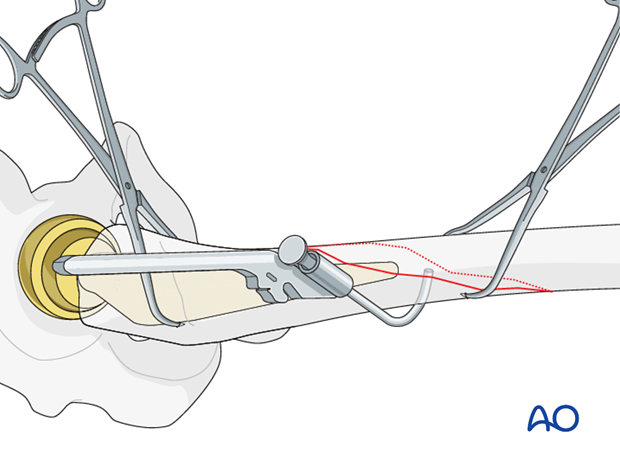
Direct reduction
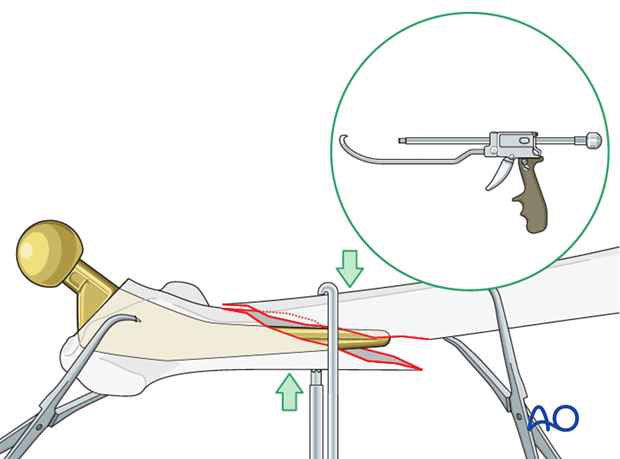
Reduction is typically carried out in a direct manner with clearance of fracture hematoma and stabilization with pointed bone reduction clamps.
The Collinear reduction clamp can be extremely helpful in facilitating reduction. It is easily applied from the direct lateral incision.
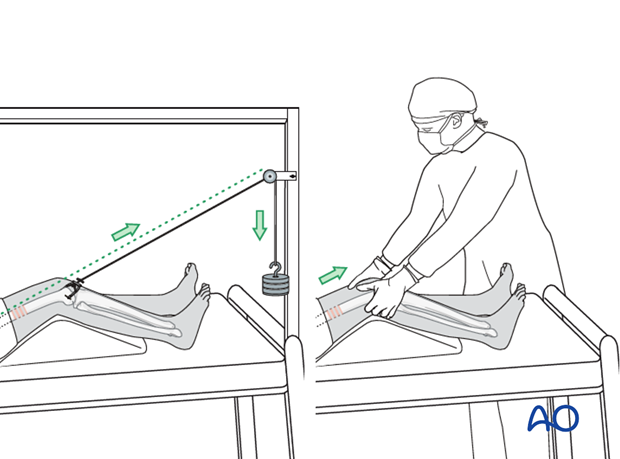
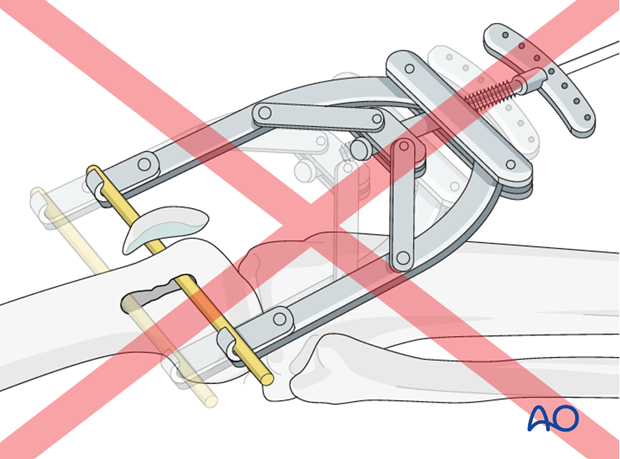
Traction aids
The reduction can be facilitated with manual traction and/or distal femoral skeleton traction.
Skeletal traction may be placed in the distal femur or the proximal tibia, depending on surgeon's preference.
However, the distal femur is much more effective in facilitating reduction of periprosthetic femur fractures.
4. Fixation
Implant selection
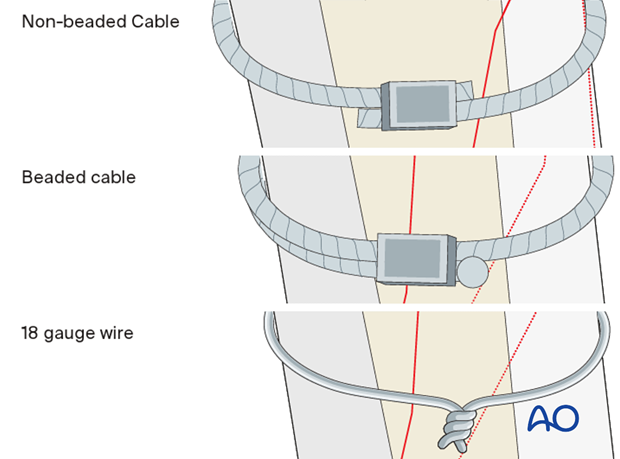
Compression can be achieved for these fractures with:
- Non-beaded cerclage type cables
- Beaded cerclage type cables: this type of system enables a more minimally invasive approach
- Large gauge wires (no less than an 18 gauge)
This can be performed in a minimal invasive or open technique, depending on available equipment and the amount of displacement of the fracture.
Instrument selection
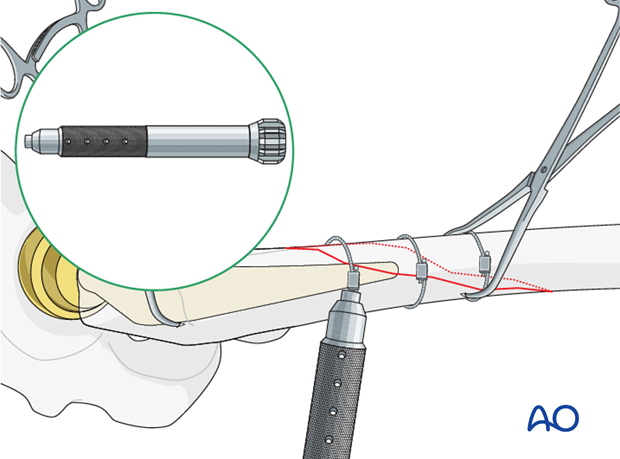
Care should be taken in passage of either construct. If available, a closed loop passage system is both safe and effective. However, a more traditional cerclage cable passer can be safely utilized also.
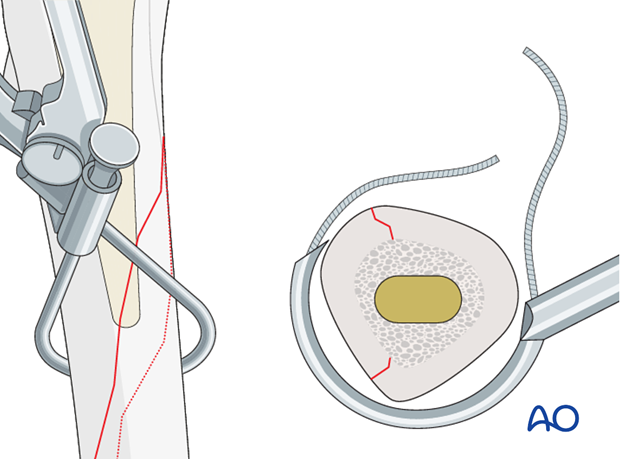
Cable/wire positioning
The first wire or non-beaded cable should be placed in the middle of the fracture.
The female component of the closed loop passage system is inserted from the posterior side.
The male component is inserted from the anterior side.
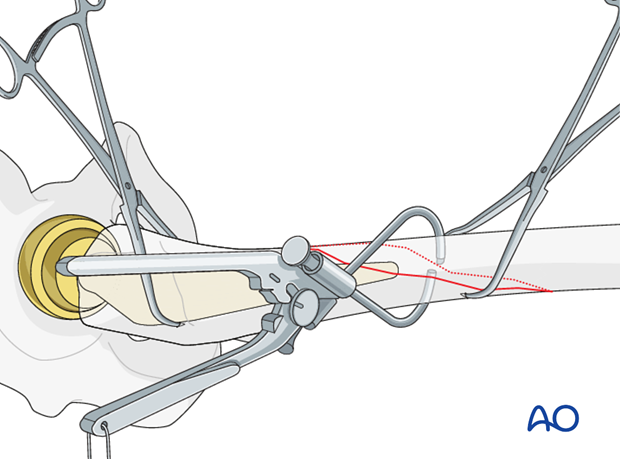
The handle components are aligned together, creating a closed loop system.
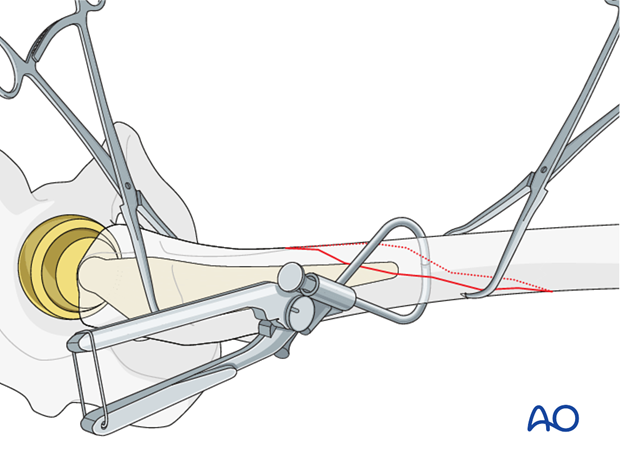
The wire is passed inside the closed loop system.
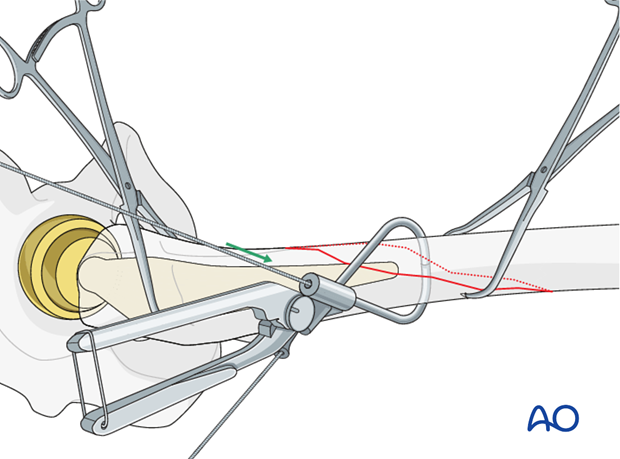
The closed loop system is removed, and the wire is left in place.
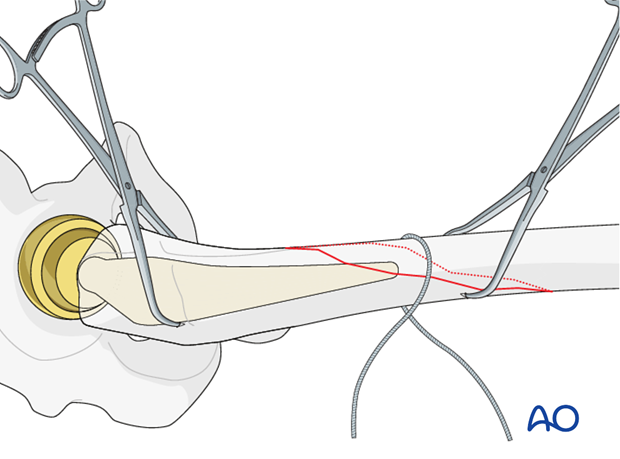
The same procedure is repeated for the insertion of each wire.
At least one proximal and one distal cable are placed to stabilize the fracture.
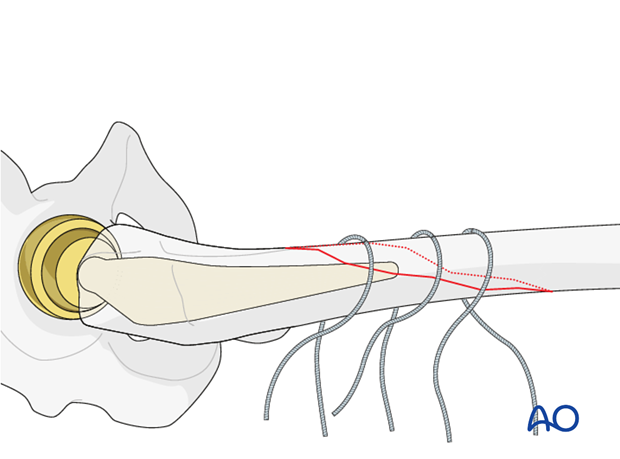
Wires should be tensioned in a sequential manner to avoid fracture displacement.
All provisional reduction aids should be maintained until all cables are crimped.
Alternatively, cable tension is performed.
Radiographic verification
Antero-posterior and medio-lateral radiographs of both the fracture sites and the arthroplasty are obtained at the end of the procedure, to ensure that:
- There is no displacement
- The joint articulation is preserved
- There is no dislocation, that may be caused by excessive distraction of the limb or a malreduction of the femur
5. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
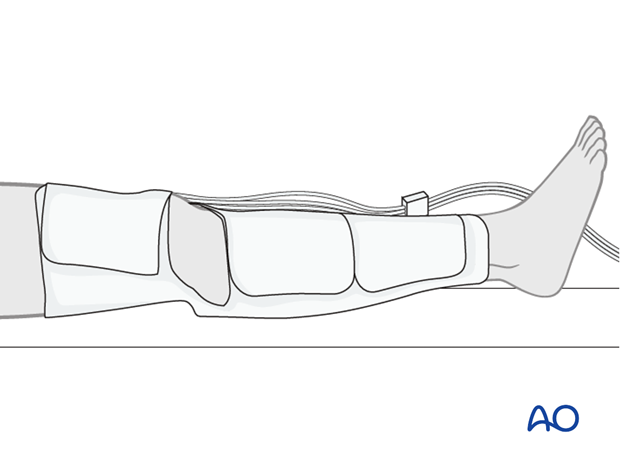
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.