Lateral approach to the femur shaft
1. Principles
This approach is useful for a periprosthetic femur fracture with a stable prosthesis or a fracture distal to the prosthesis.
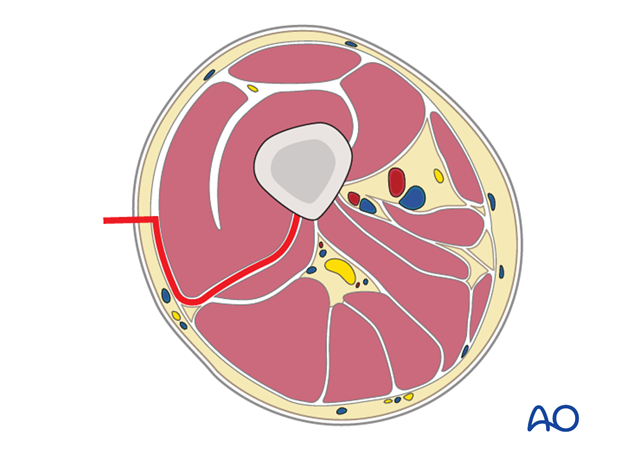
The major vessels and nerves are located medially/posteromedially to the femoral shaft and are not exposed using this approach.
This approach can be performed with the patient supine or in lateral decubitus.
Scar tissue due to previous exposure might obscure typical landmarks.
2. Skin incision
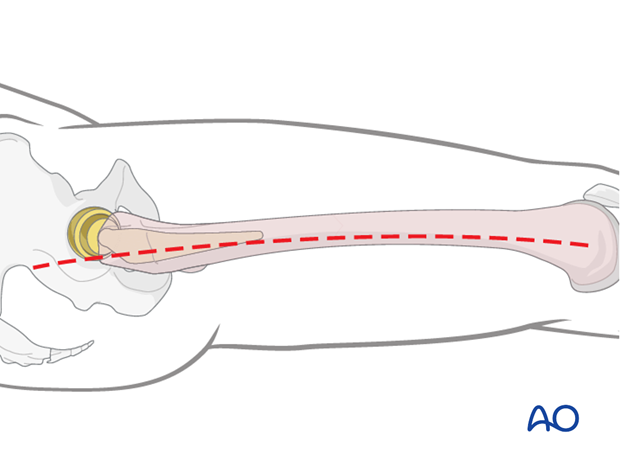
An incision is made along an imaginary line between the lateral femoral epicondyle and the greater trochanter, along the length of the femur required by the specific fracture pattern.
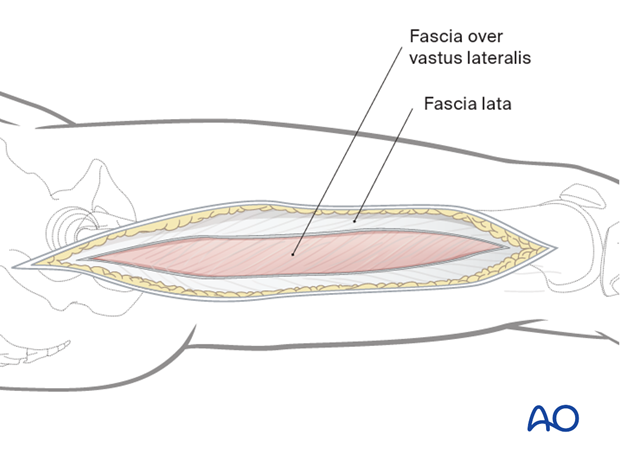
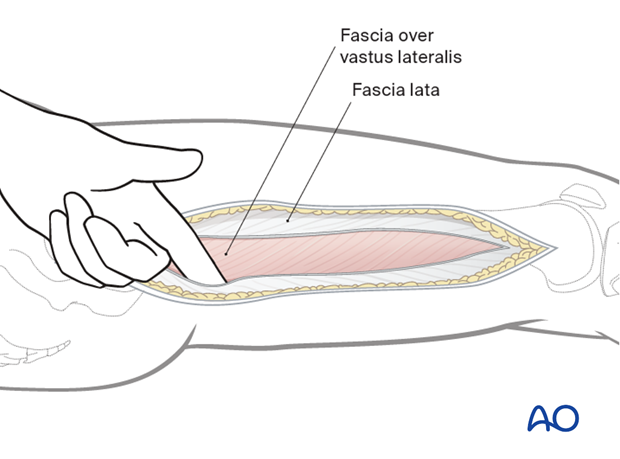
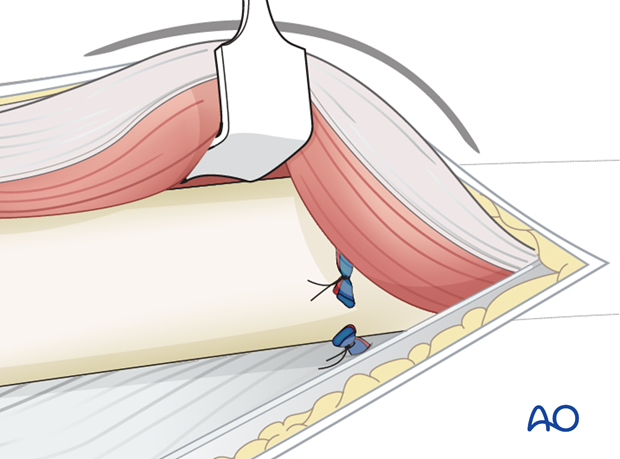
3. Opening the fascia lata
The fascia lata is incised with a scalpel and split with scissors parallel to the skin incision, along its fibers.
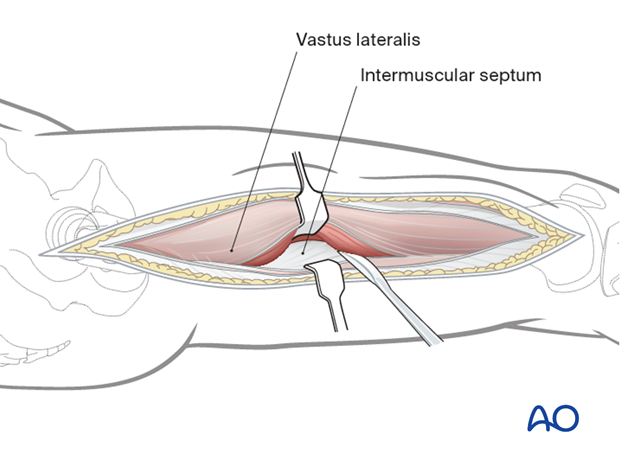
4. Principles of a safe approach
As the fibers of origin of the vastus lateralis are elevated from the intermuscular septum, take care, as the femur is approached, to try to pick up the perforating vessels and ligate them before they are inadvertently torn. If they are torn close to the septum, the posterior ends can retract into the posterior compartment of the thigh, with the occasional risk of troublesome occult bleeding.
The major vessels and nerves are located medially/posteromedially to the femoral shaft and are not exposed using this approach.
5. Separation of vastus lateralis from the fascia lata
The vastus lateralis is separated by blunt dissection from the fascia lata using manual palpation or a blunt instrument, such as a Cobb elevator.
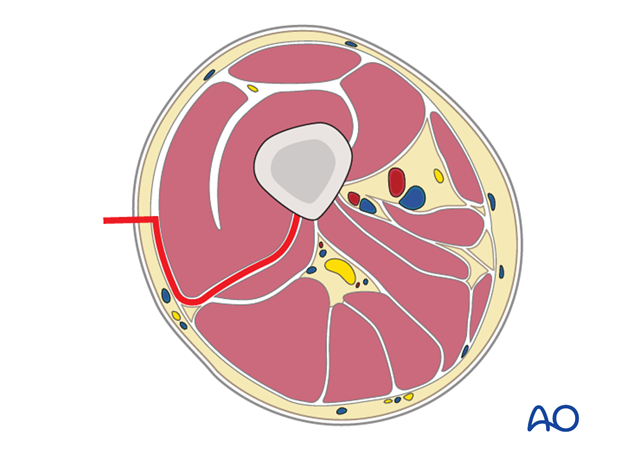
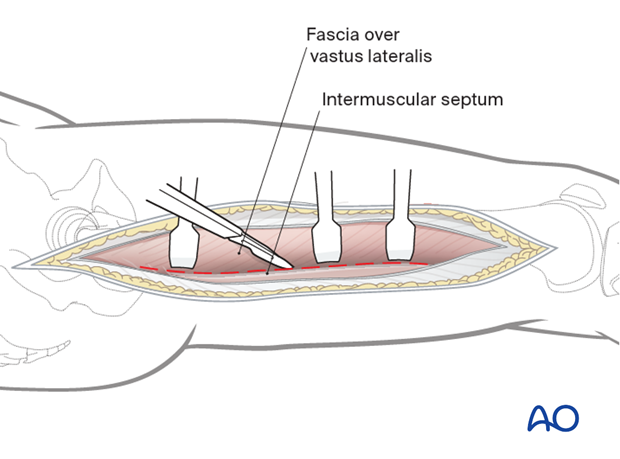
6. Incision of the fascia vastus lateralis
The vastus lateralis is now retracted anteromedially.
The muscle fascia investing the vastus lateralis is incised about 1 cm anterior to the intermuscular septum.
7. Mobilization of vastus lateralis from intermuscular septum
The muscle is detached from the lateral intermuscular septum and the linea aspera with a periosteal elevator.
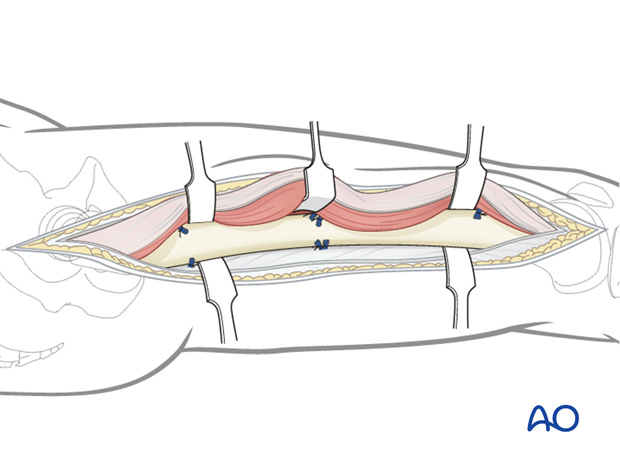
8. Ligation of perforating vessels
The perforating vessel bundles must be identified.
These vessels perforate the lateral intermuscular septum from the posterior side and run anteriorly, remaining closely applied to the femoral shaft.
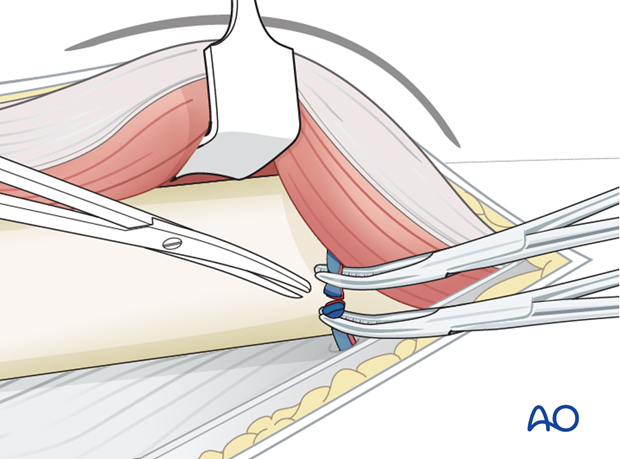
Larger vessel bundles must be ligated, smaller ones can be alternatively cauterized with the diathermy.
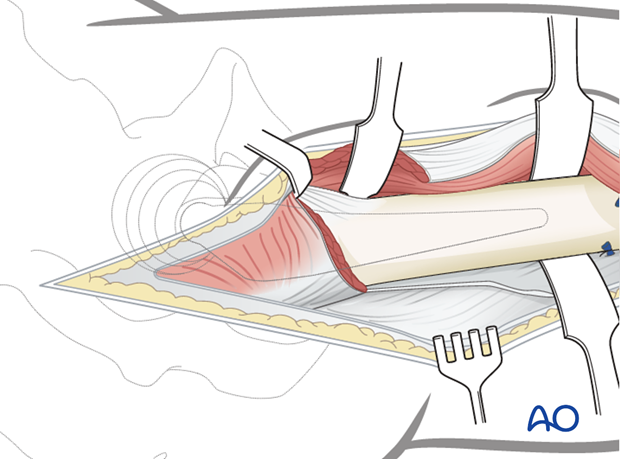
9. Exposure of the bone
After further detachment of the vastus lateralis, using the elevator, the femoral shaft is exposed extraperiosteally.
10. Exposure of the proximal femoral shaft
If exposure of the proximal femoral shaft is necessary, mostly only for subtrochanteric fractures, the origin of the vastus lateralis must be identified.
The muscle is retracted anteriorly, and an L-shaped incision is made down to the bone. The muscle origin is then dissected off with the periosteal elevator.
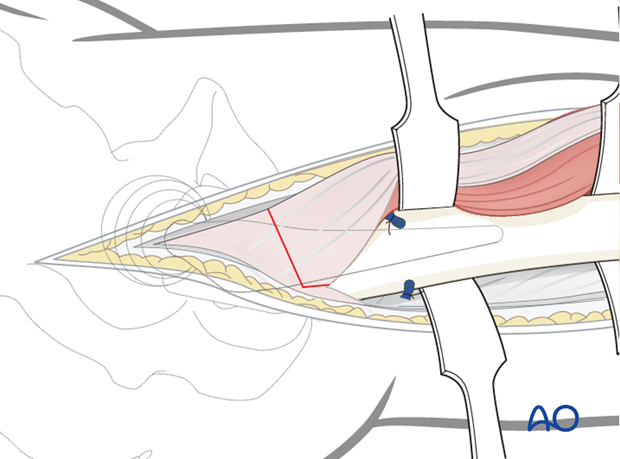
The proximal femoral shaft is exposed as necessary after the L-shaped detachment of the vastus lateralis has been performed. The vertical part of the incision lies in the interval between gluteus medius and vastus lateralis.
11. Closure
The vastus lateralis is allowed to fall back over the top of the lateral femur and repaired to its anterior and lateral origin if possible. The tensor fascia lata is closed with heavy stitches.
Considerations for periprosthetic fracture patients
A layered closure is preferred for periprosthetic fractures. A subfascial drain should be considered as blood loss can be significant and periprosthetic fracture patients are at high risk of requiring anticoagulation immediately postoperatively. A hematoma requiring evacuation must be avoided. The wound is closed in layered fashion according to the surgeon's preference.
Sterile dressing should be applied, and negative pressure incisional wound care can be considered.

12. Possible extensions
This approach can be extended proximally into a posterolateral approach to the hip joint if needed.














