ORIF - Plates without angular stability
1. Principles
General consideration
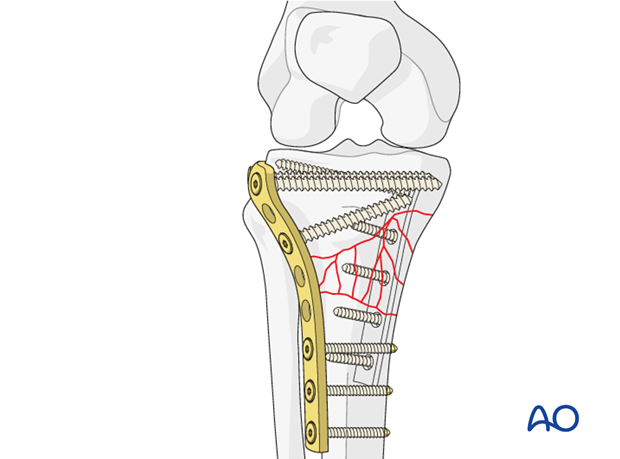
In unstable fractures it is helpful to consider the tibia as having a medial and lateral column. A lateral plate on its own is often not sufficient, and the medial side may be supported by a posteromedial small fragment plate.
High degree of medial comminution
If there is a high degree of medial comminution combined with a bad soft-tissue injury do not use conventional plates. This is an indication for the use of the LISS locking plate.
If the LISS plate is unavailable to you then consider a lateral bridge plate plus a medial external fixator (temporary 6 weeks). The disadvantage of the external fixator is the risk of sepsis with the use of periarticular Schanz screws.
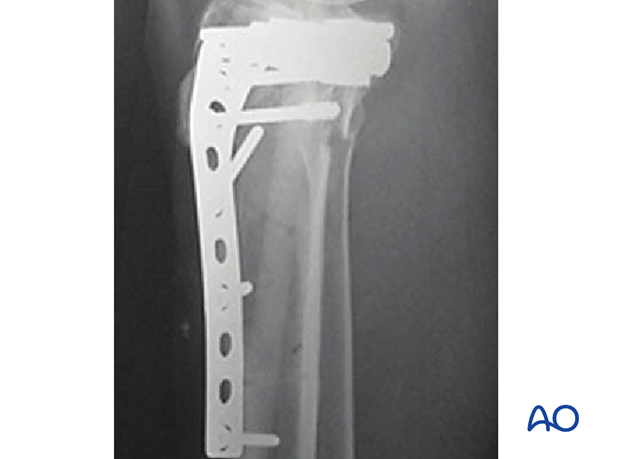
In these x-rays the position of the proximal Schanz screw is dangerously close to the joint. The preferred position for this screw is at least 14 mm below the joint line.

This shows the lateral projection.
Compartment syndrome
Monitor the neurovascular status of the limb carefully not to miss a compartment syndrome.
2. Patient preparation
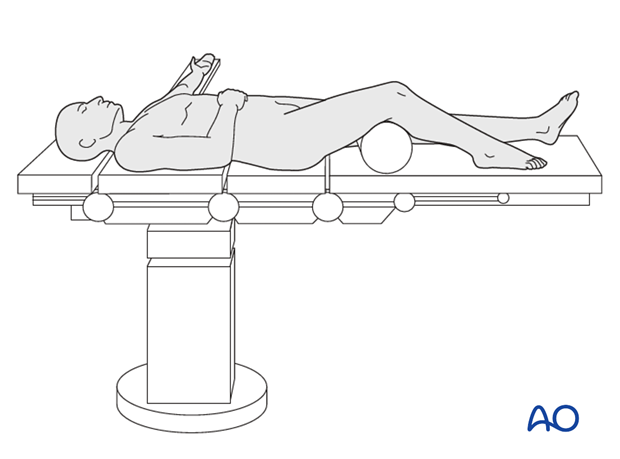
This procedure is normally performed with the patient in a supine position. By allowing the limb to lie in a externally rotated position, access may be gained through a posteromedial approach.
If a posterior approach is preferred the patient should be placed in a prone position.
3. Approaches
For this procedure the following approaches may be used:
4. Reduction
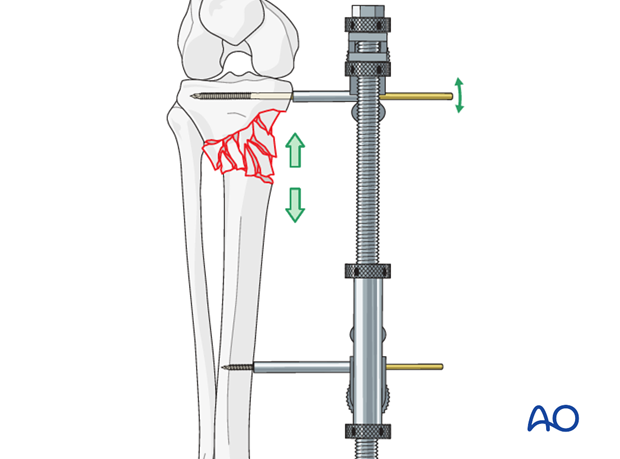
Place distractor opposite of planned fixation device
For extraarticular tibial fractures (metaphyseal wedge or multifragmentary) the large or femoral distractor may be used during the fixation of the medial or lateral side depending on where the fixation device will be placed. Eg, the distractor is placed on the medial side if the fixation device will be applied onto the lateral side.
5. Fixation
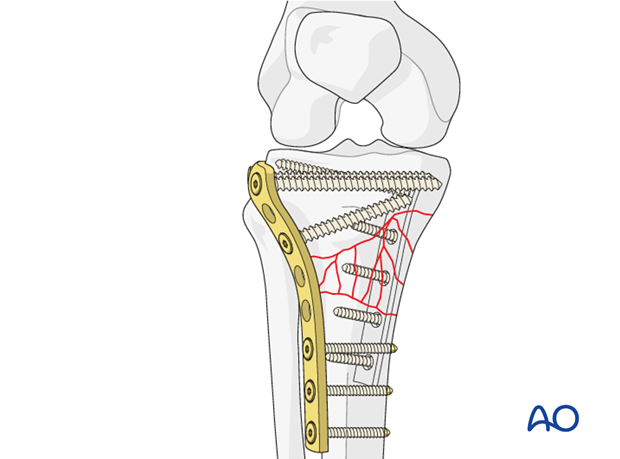
Medial Column Fixation
Reduction and fixation of the medial column is obtained by a one-third tubular plate through a separate posteromedial approach.
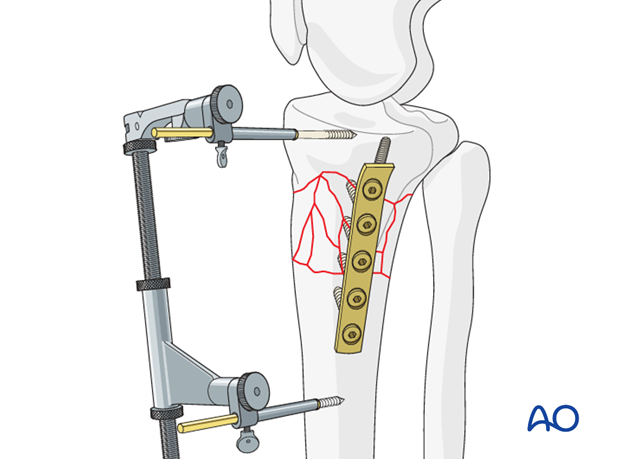
Lateral column fixation
The lateral side is reduced through a standard lateral approach. Reduction and fixation was obtained with a lateral L-plate 4.5 which functions here as a bridge plate.
The medially applied disctactor may interfere with screw insertion, but the distractor should be kept until both sides are stabilized to prevent loss of reduction.
Removal of medial distractor
The medial distractor should be kept as long as possible and be removed only after application of both plates.
6. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the tibial compartments should be carried out especially during the first 48 hours to rule out compartment syndrome.
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Unless there are other injuries or complications, mobilization may be performed on post OP day 1. Static quadriceps exercises with passive range of motion of the knee should be encouraged. Afterwards special emphasis should be given to active knee and ankle movement.
The goal of early active and passive range of motion is to achieve a full range of motion within the first 4 – 6 weeks. Maximum stability is achieved at the time of surgery. A delay beyond a few days to allow swelling to subside is illogical and harmful.
Weight bearing
Partial weight-bearing (touch down or of 10 to 15 kilograms) may be performed with crutches or a walker.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 6 and 12 week follow-up is usually performed. If delayed healing occurs additional bone grafting may be required.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.













