Lag screws
1. Principles
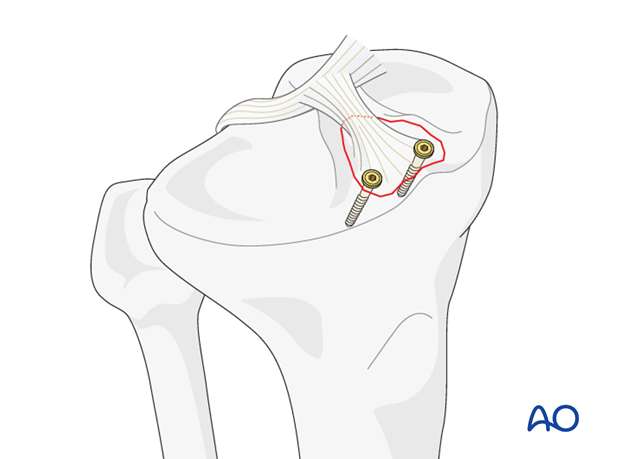
Avulsion of anterior cruciate ligament
This injury represents an avulsion of the anterior cruciate ligament.
This intraarticular avulsion fracture is most often seen in the younger patient.
Number of screws
Depending on the size of the fragment one or two antegrade lag screws are used.
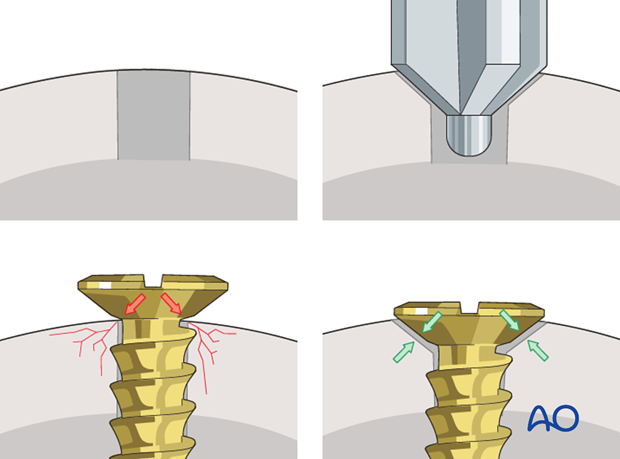
Countersinking
There are two important reasons for countersinking:
- To produce a lower profile of the screw head and thus avoiding soft-tissue irritation.
- Countersinking also ensures that the screw head has a maximum contact area with the bone, which leads to an even distribution of forces between the screw head and bone.
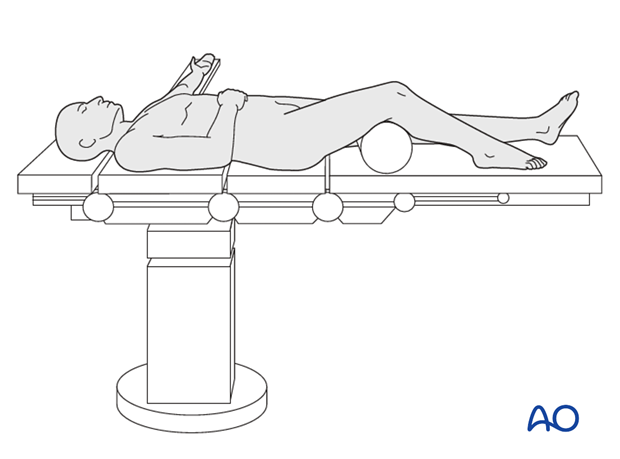
2. Patient preparation
This procedure is normally performed with the patient in a supine position.
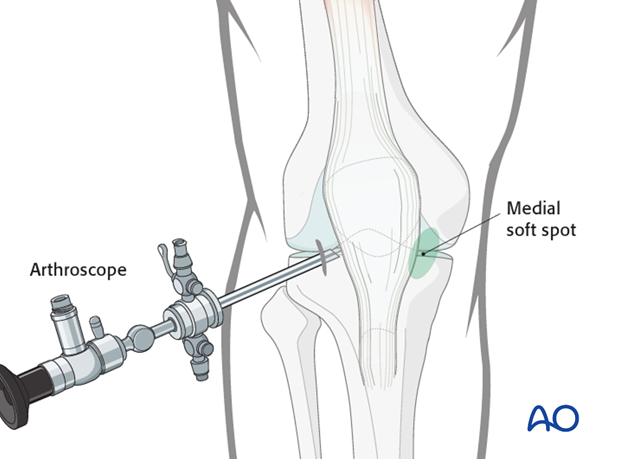
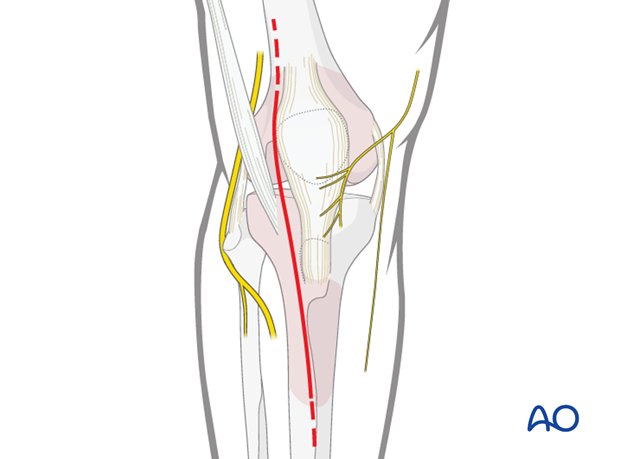
3. Approaches
Arthroscopic approach to the knee
The arthroscopic approach may be used but advanced experience in arthroscopic surgery is essential.
Anterolateral approach
For open reduction an anterolateral approach is used.
4. Reduction
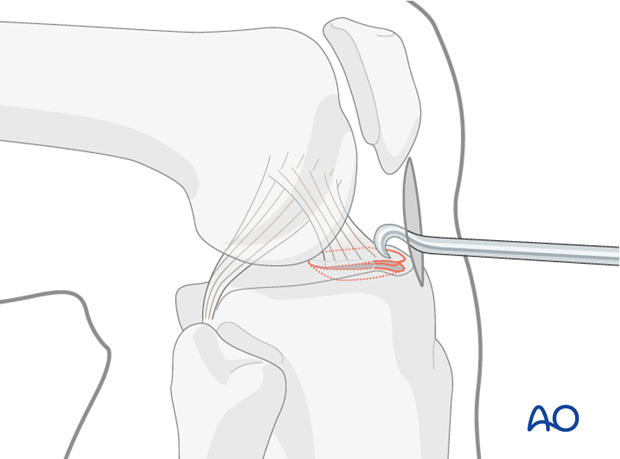
Arthroscopy
The fracture is visualized with the arthroscope and reduction is attempted with a hook or another instrument inserted through another portal.
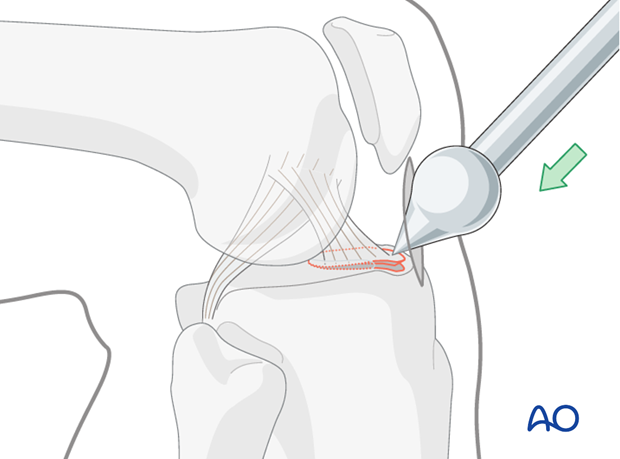
Alternative: ball-spiked pusher
Alternatively, a ball-spiked pusher may be used.
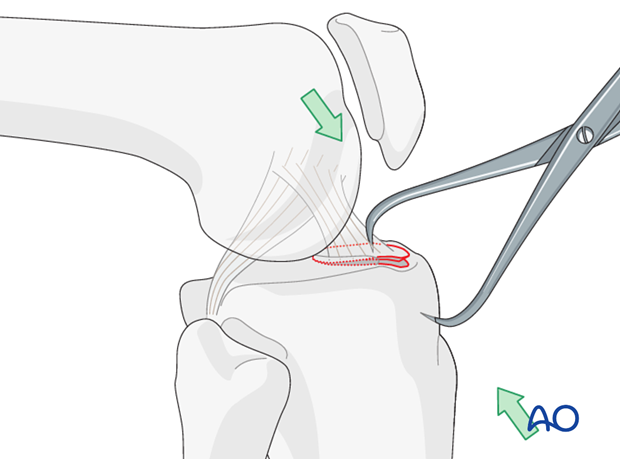
Clamps
In open procedures, the avulsed bony fragment of the intercondylar eminence is visualized directly and may be reduced with the help of a clamp or a ball-spiked pusher.
5. Fixation
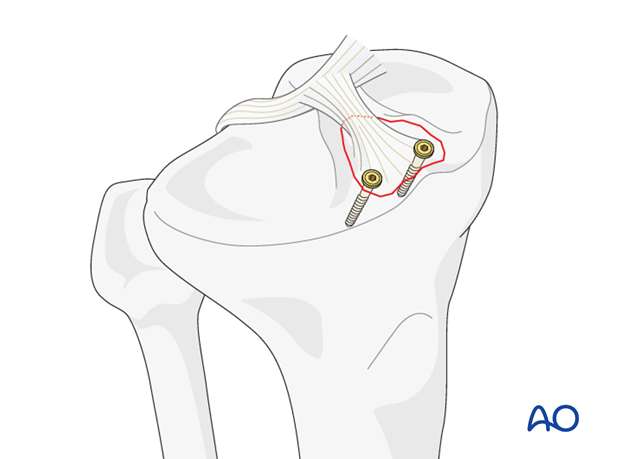
Lag screw application
Fixation should be performed with the screws not compromising the articular cartilage or ligament insertion sites. Cannulated small fragment screws are preferred.
Click here for a detailed description of the lag screw technique.
The lag screw fixation as a primary fixation will ensure anatomic reduction. Unless one is dealing with a very young individual with very dense cancellous bone, one should supplement the screw fixation with wiring as illustrated below.
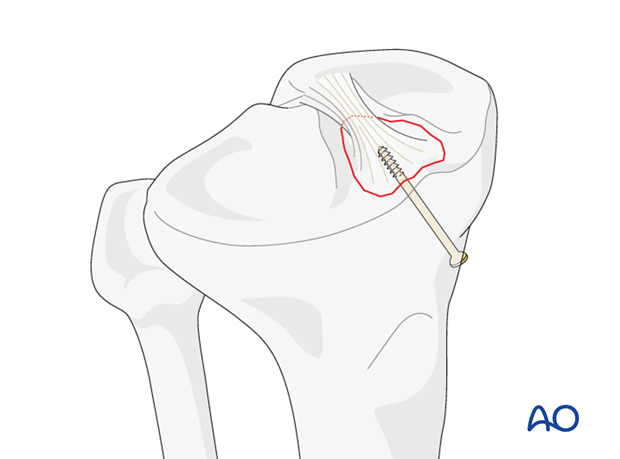
Alternative: retrograde lag screw application
In case of a solid avulsion fragment retrograde fixation with a small cancellous screw can be performed. Antegrade lag screws are usually left in place whereas these retrograde lag screws can be easily removed after fracture healing.
The lag screw fixation as a primary fixation will ensure anatomic reduction. Unless one is dealing with a very young individual with very dense cancellous bone, one should supplement the screw fixation with wiring as illustrated below.
6. Aftercare
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Unless there are other injuries or complications, mobilization may be performed on post OP day 1. Static quadriceps exercises with passive range of motion of the knee should be encouraged. Early active range of motion of knee and ankle is encouraged.
The goal of early active and passive range of motion is to achieve a full range of motion within the first 4 – 6 weeks. Maximum stability is achieved at the time of surgery. A delay beyond a few days to allow swelling to subside is illogical and harmful.
Weight bearing
A hinged brace is used with non-weight bearing for 6 weeks.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 8 week follow-up is usually performed.
Implant removal
Implant removal is optional after retrograde lag screw fixation and suturing.
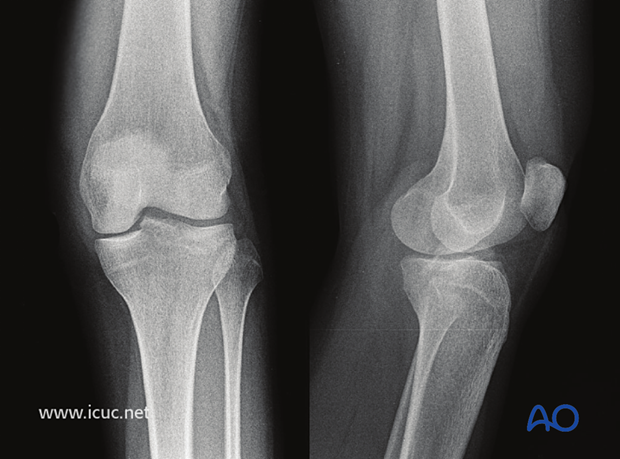
7. Case
AP and lateral X-rays demonstrating avulsion of the tibial spine with slight displacement.
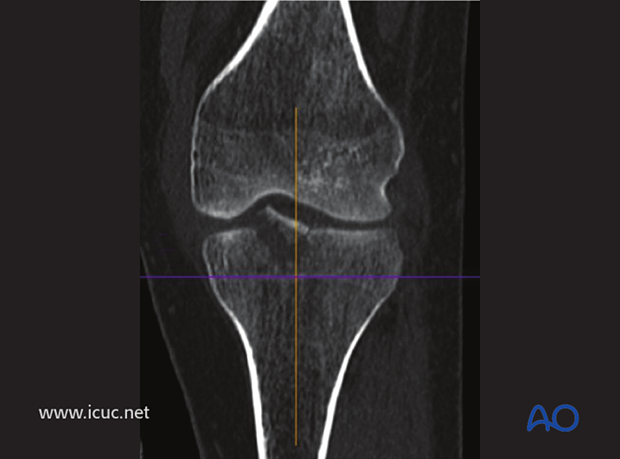
CT scan in coronal image showing the displacement.
Medial parapatellar incision is used.

The medial parapatellar retinaculum is opened and the joint capsule is incised, revealing a hemarthrosis.
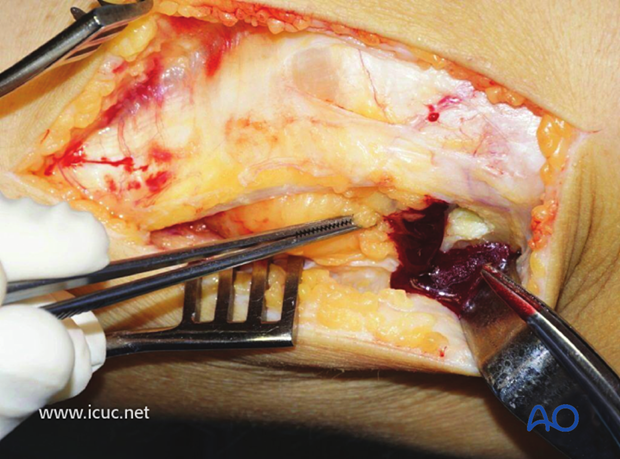
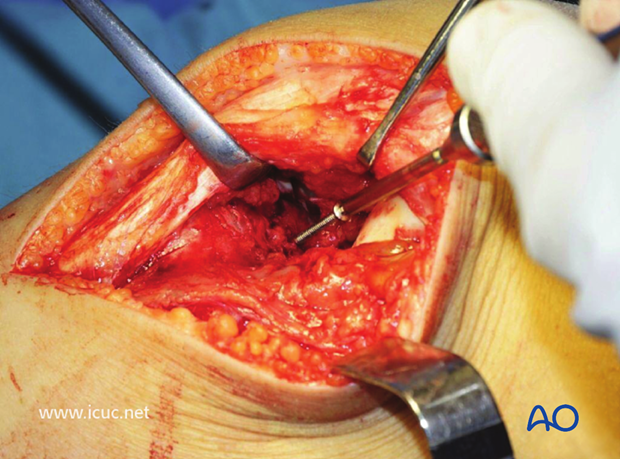
By elevating the patella with the knee extended, the avulsed tibial spine can be seen. This image shows a pair of forceps in the fracture gap below the tibial spine.
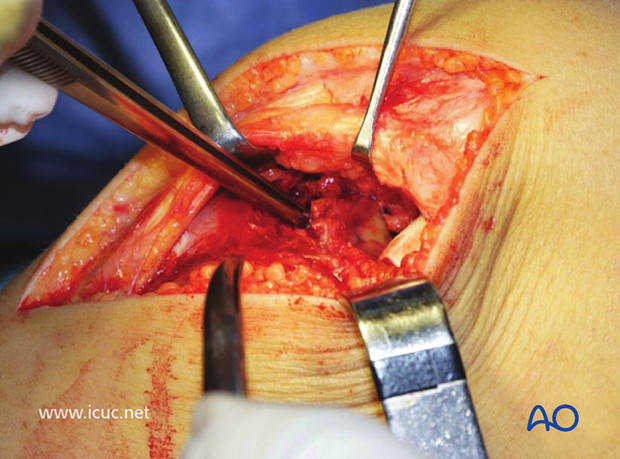
The hematoma has been removed from beneath the avulsed tibial spine and it has been reduced and held with a K-wire.
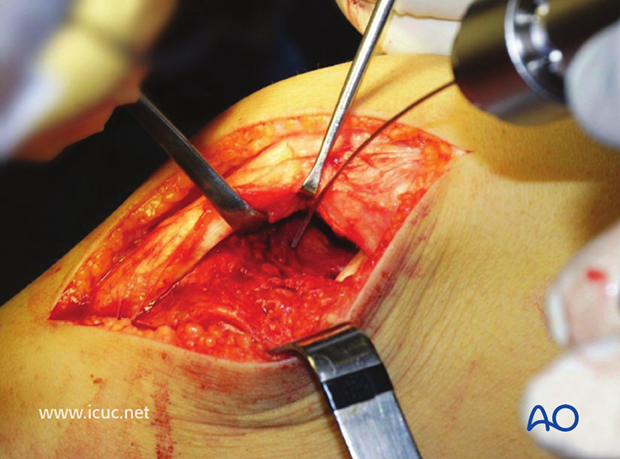
A small fragment cancellous lag screw is inserted.
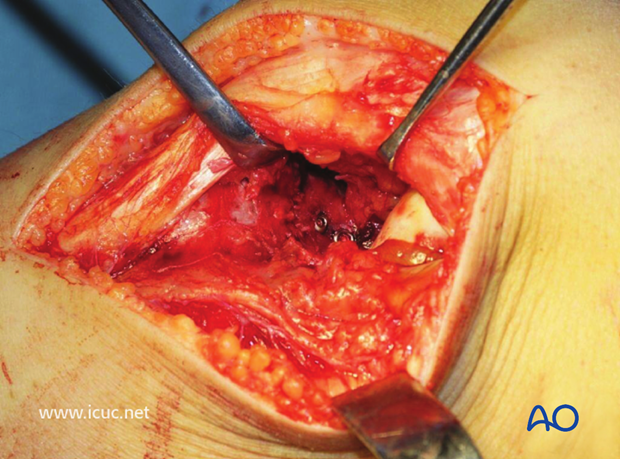
A second lag screw is inserted.
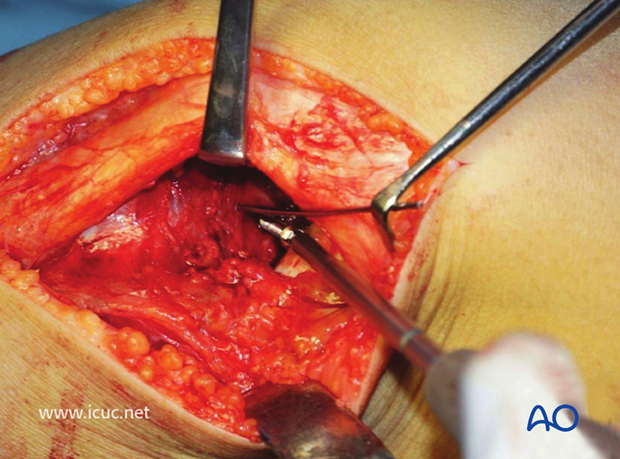
Final intraoperative view of the tibial plateau.
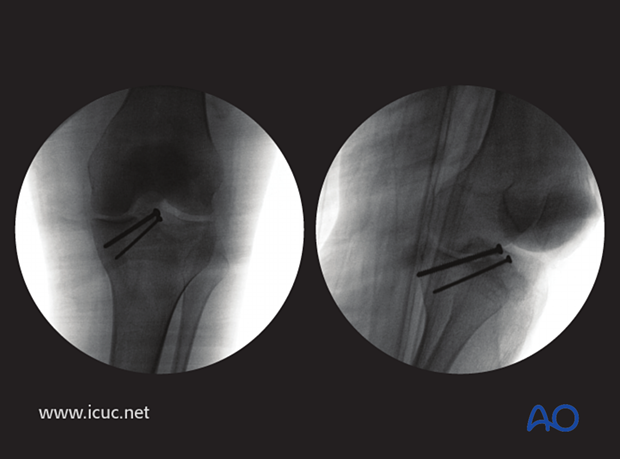
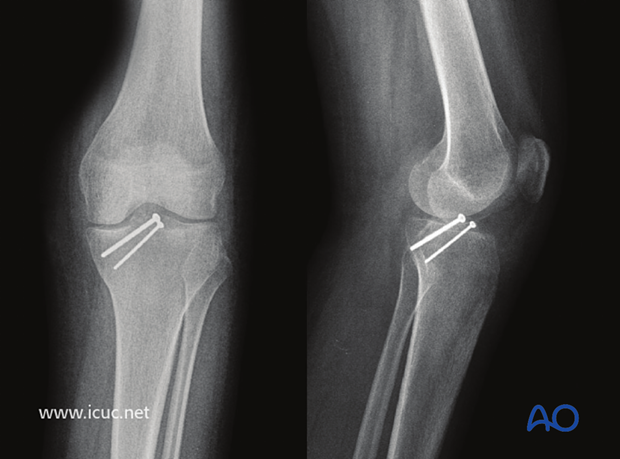
Intraoperative check X-rays in two views.
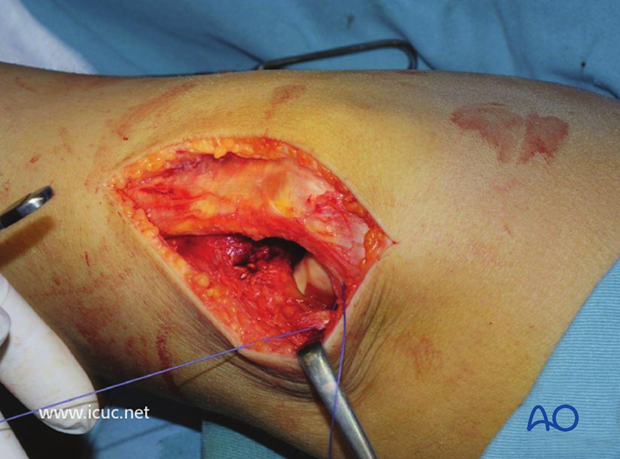
The medial parapatellar retinaculum and capsule are carefully repaired.
Four-week X-ray showing nice reduction of the spine.
One-year images showing maintenance of flexion and full extension of the knee.














