Open reduction internal fixation
1. Introduction
Apex posterior fractures of the proximal ulna with posterior dislocation of the radial head behind the capitellum are posterior fracture-dislocations of the elbow.
The radial head is almost always fractured.
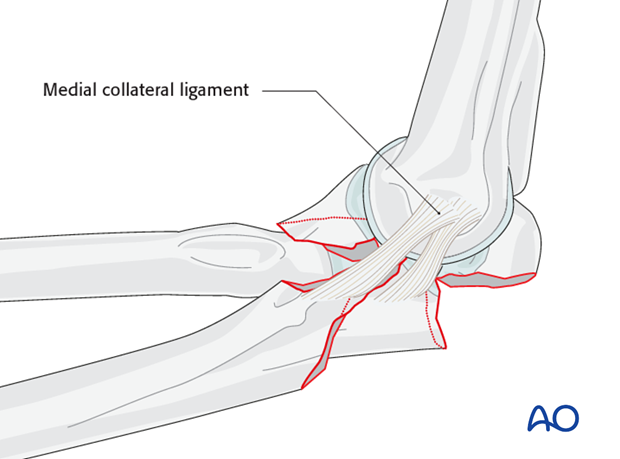
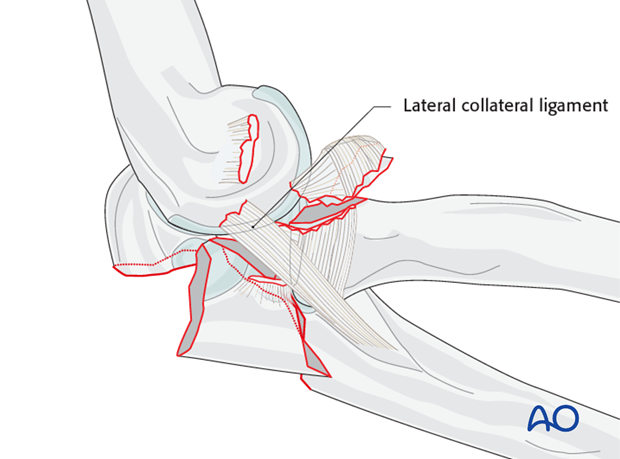
The lateral collateral ligament is avulsed from the lateral epicondyle in 50% of injuries.
The medial collateral ligament is intact unless the ulnohumeral joint is completely dislocated.
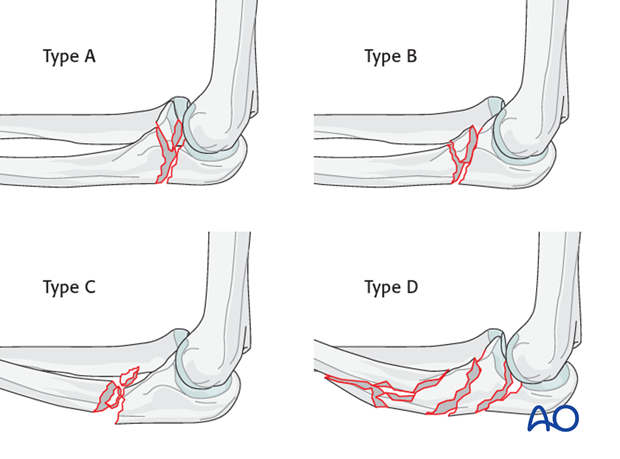
These can be considered part of the spectrum of posterior Monteggia lesions as described by Jupiter and colleagues:
- Type A - intraarticular (olecranon) fractures
- Type B - metaphyseal (extra-articular)
- Type C - diaphyseal
- Type D - multifragmented and multifocal
Principles
- The key is restoration of the trochlear notch of the ulna by correct alignment of the coronoid and olecranon processes.
- Metaphyseal and diaphyseal fragmentation can be bridged with a long plate.
- The fractures are often associated with osteoporosis.
- When the coronoid is fractured, it is often fragmented, and sometimes benefits from temporary immobilization of the elbow with external fixation or cross pinning.
2. Positioning
Both lateral decubitus and supine position can be used for these fractures. The advantages and disadvantages of both are discussed below.
Lateral decubitus
Advantages
- No one needs to hold the arm.
- The skin flaps tend to fall away reducing the need for assistance with retraction.
- There is direct access to the ulnar fracture.
Disadvantages
- It is more difficult to make a lateral approach to the radial head.
- The setup of the patient is more difficult.
- Positioning increases the risk of injury to the peroneal nerve.
Supine
Advantages
- The arm can be placed across the patient’s chest for the proximal ulnar approach and on the table for access to the radial head and neck.
- Intraoperative imaging is easier.
Disadvantage
- The arm will need to be held across the chest by an assistant.
If a medial approach is selected place the arm on an arm board with the shoulder abducted and the arm externally rotated.
3. Approaches
Use a straight posterior skin incision.
A lateral skin flap can be raised for a lateral exposure (Kaplan or Kocher) of the radius if needed.
A medial skin flap (Taylor and Scham, or “Over the top”) can be raised for medial exposure of the coronoid fracture if needed.
Exposure of a coronoid fracture is improved by elevating the fractured olecranon on the triceps as with an osteotomy.
If a second medial plate will be used to secure the coronoid, one can - after taking care to protect the ulnar nerve - either elevate the entire flexor pronator mass (Taylor and Sham) or use the interval where the ulnar nerve lies in the split of the FCU (“Over the top” or Hotchkiss).
During the exposure it should be verified whether the lateral collateral ligament origin is avulsed from the lateral epicondyle or not.
The radial head can be accessed either by recreating the apex posterior fracture of the proximal ulna - thereby subluxation or dislocating the radial head posterior to the capitellum as typically occurs in this injury - or one can use a separate lateral muscle interval (Kocher or Kaplan).
For most fractures of the radial head that are replaced with a prosthesis or have a repairable partial articular fracture, recreating the deformity and using and perhaps slightly enlarging the rent in the anconeus muscle usually provides sufficient exposure of the radius.
4. Fixation
Sequence of repair
- Address radial head fracture.
- Address coronoid fracture.
- Address lateral collateral ligament avulsion.
- Realign and secure the olecranon fragment.
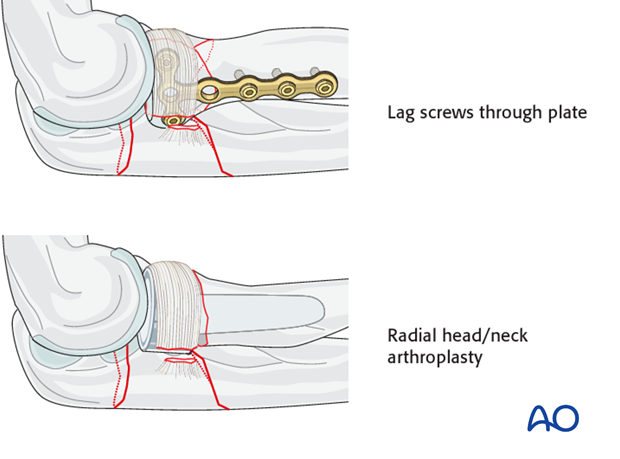
Partial radial head fractures
If there is partial articular fracture consisting of 1-2 fragments, screw fixation is used.
For greater fragmentation (> 3 fragments including the intact head) the radial head is excised and replaced by a prosthesis.
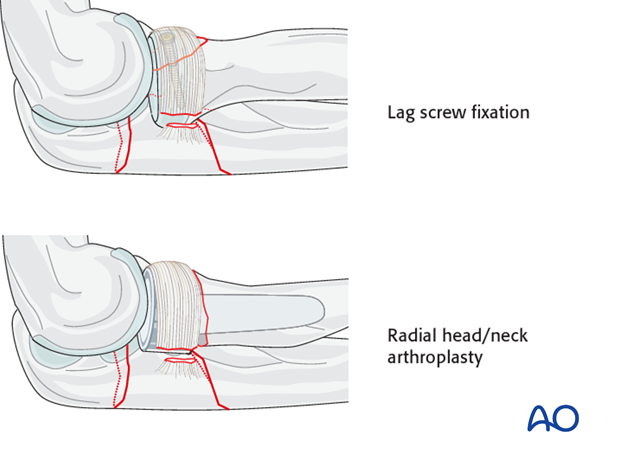
Complete radial head fractures
A complete articular fracture consisting of 3 or less fragments, large enough to warrant repair, plate fixation is performed.
If comminution exceeds 3 fragments, the head is not salvageable and should be replaced.
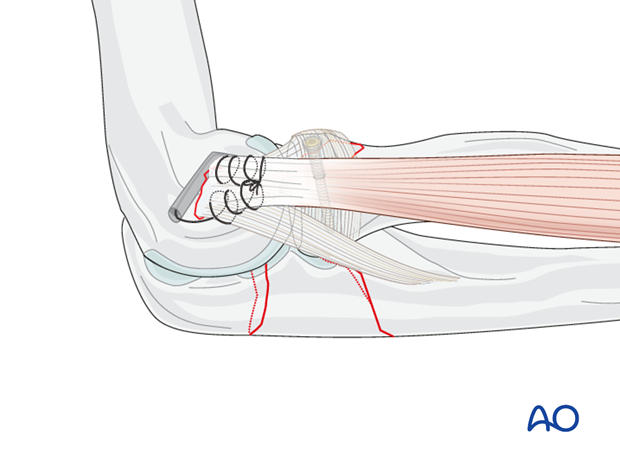
Coronoid repair
After mobilizing the olecranon process with the triceps, address the basilar coronoid fracture.
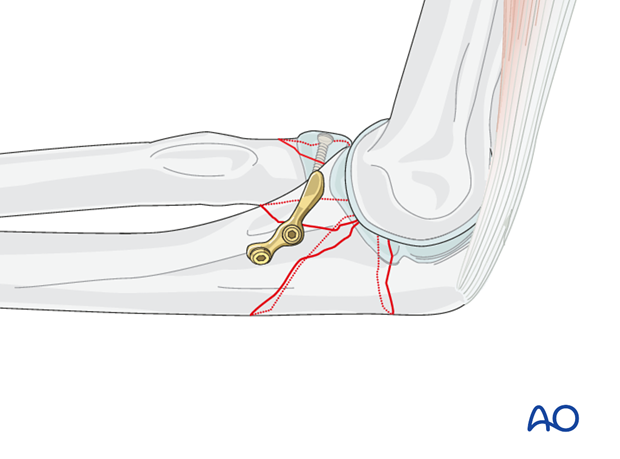
Ligament injury
For posterior olecranon-fracture dislocations the origin of the LCL can be accessed and reattached through the olecranon fracture once the olecranon fragment has been mobilized.
If avulsed from the lateral epicondyle, reattach the lateral soft tissue sleeve including the origin of the LCL to the lateral epicondyle in the appropriate sequence.
The LCL origin is always avulsed if there is a complete dislocation of the ulnohumeral joint and should be repaired.
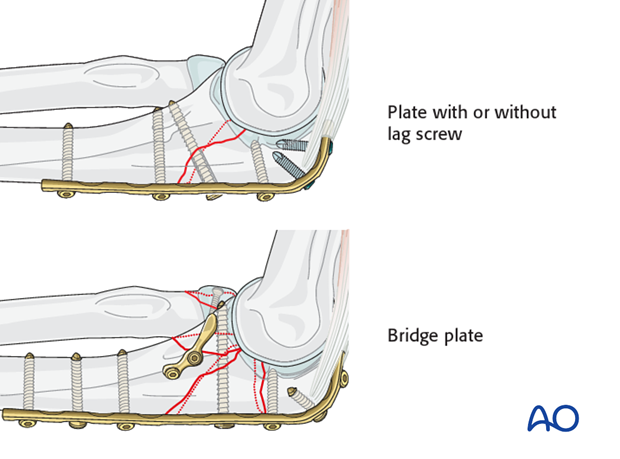
Repair the olecranon with a posterior plate
- Simple: Plate with or without lag screw
- Multifragmentary: Bridge plate
5. Final assessment
Check for dislocation or subluxation of the ulnohumeral joint in full gravity extension under a lateral image. Check for crepitation with forearm or elbow motion.
6. Postoperative treatment following ORIF
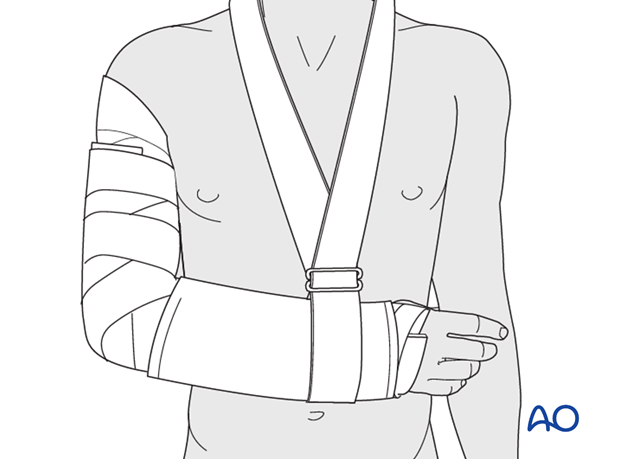
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
Mobilization
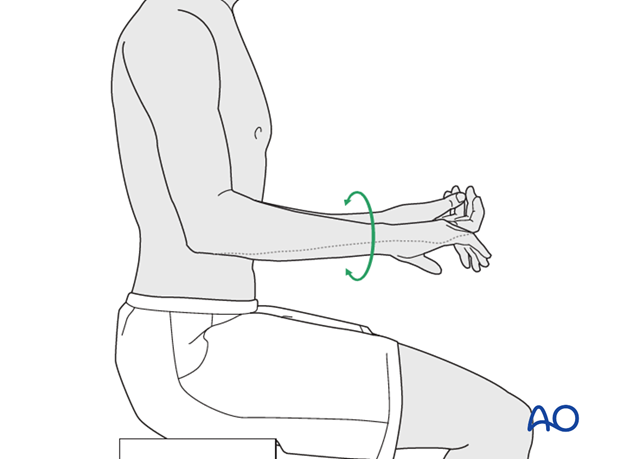
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
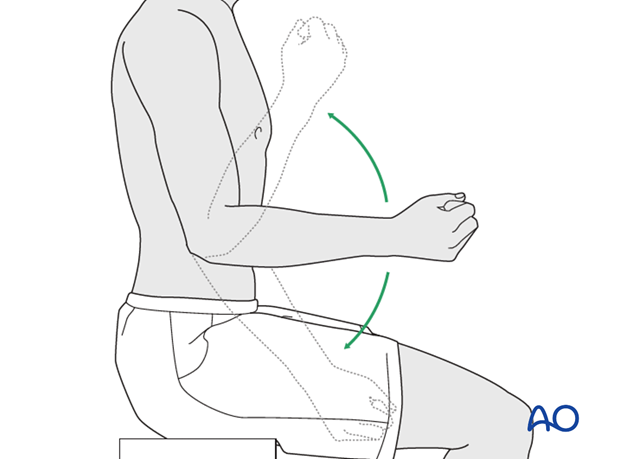
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













