Operative treatment
1. Introduction
Before proceeding with definitive repairs, the patient must be fully resuscitated, fully evaluated, and fit for anesthesia and surgery by a prepared team.
Most lateral compression injuries are only slightly displaced and are mechanically stable and treated nonoperatively. However, a broad spectrum of injuries is included in this fracture type. It includes injuries with deformity that will remain symptomatic, and others with occult instability that may progressively deform, in spite of benign appearing initial x-rays.
The main challenge when treating lateral compression fractures is to identify the few which requires operative treatment.
2. Instability of lateral compression injuries
Pitfalls when treating these injuries:
- Accepting excessive deformity
- Failing to recognize and reduce risk of progressive deformity
Recognizing the risks of progressive displacement and malunion helps prevent the need for complex late surgical corrections.
Our understanding of these injuries is still evolving. At present it is not clear how much pelvic deformity can be accepted, nor how best to identify those patients who may benefit from fixation.
Identification of instability
Unless obviously displaced, posterior arch fractures in lateral compression injuries may be hard to identify, particularly if only an AP x-ray is examined.
CT scans are required to clarify the character of these fractures.
The following features indicates increased risk of mechanical instability with progressive deformity:
- Complete posterior fractures
- Comminuted posterior fractures
- Displaced posterior fractures (determined by CT scan)
- Associated bilateral or comminuted anterior fractures
The amount of fracture instability is not always predictable from static x-rays or CT scans.
Treatment of instability
Posterior pelvic arch fixation may be indicated to prevent progressive deformity, or to provide stability after reduction.
Pelvic fractures usually consolidate within 4-6 weeks. If treated nonoperatively, reassessment after 3-4 weeks preserves the opportunity to correct an “incipient malunion”.
3. Lateral compression fracture anatomy
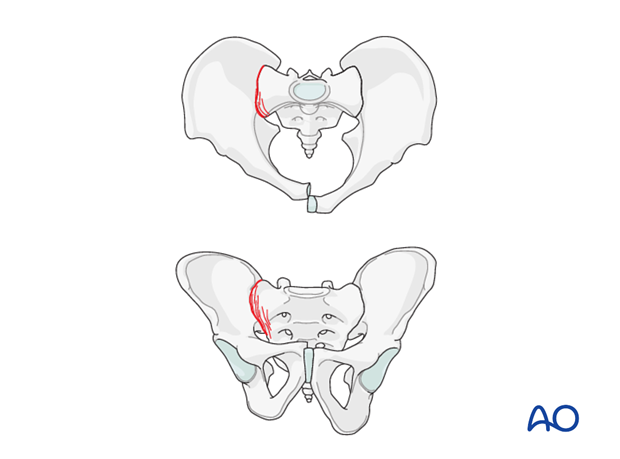
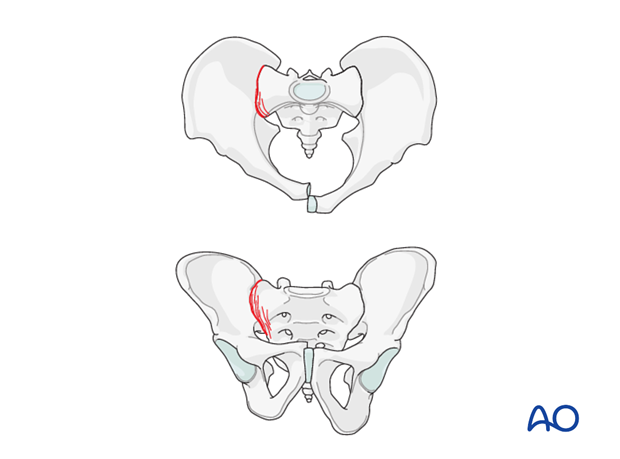
B2.1 Sacral fractures (LC-I)
These injuries are defined as having sacral compression fractures, with internal rotation deformity and transversely oriented pubic ramus fractures.
The classic lateral compression injury is described as unstable only in rotation.
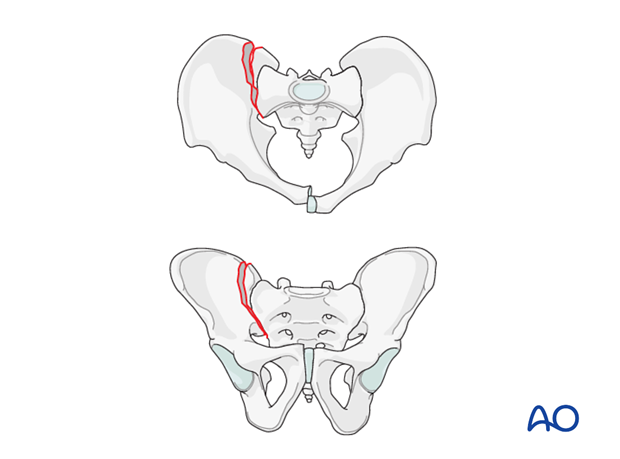
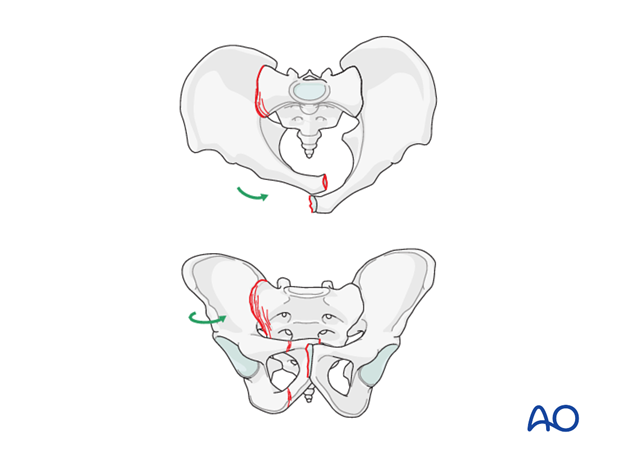
SI (crescent) fracture subluxation (LC-II)
These fracture subluxations have been considered unstable enough to need fixation. However, if undisplaced, without instability on stress x-rays non-operative management may be considered.
A very small crescent fragment can be ignored. Repair of the SI joint is essential unless it is completely stable.
Some crescent fractures do not have enough articular surface to support an iliosacral screw, nor to provide sufficient joint stability. In such cases the anterior ilium must be reattached to the crescent fragment.
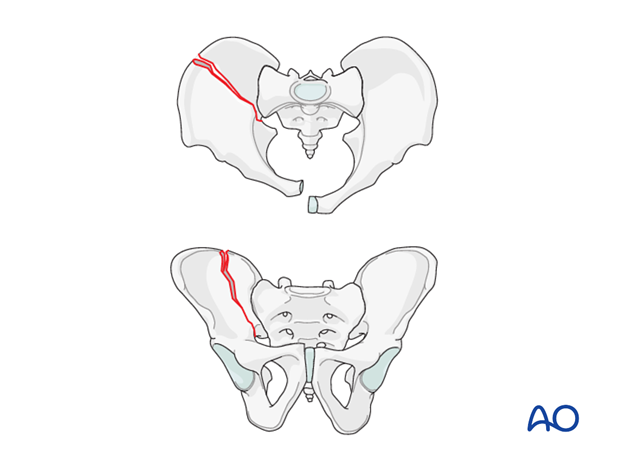
Posterior Iliac fracture (LCII)
These fractures begin anterior to the joint and usually require surgical repair. This is most easily repaired through an anterolateral approach to the iliac fossa.
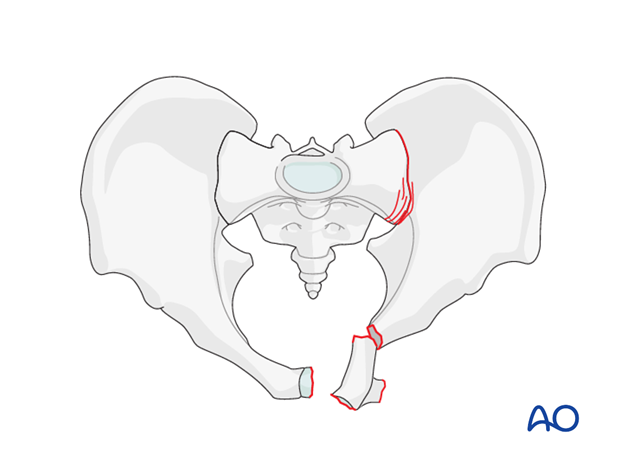
Anterior injury
The anterior component in a lateral compression injury almost always involves pubic ramus fractures, typically in a transverse orientation.
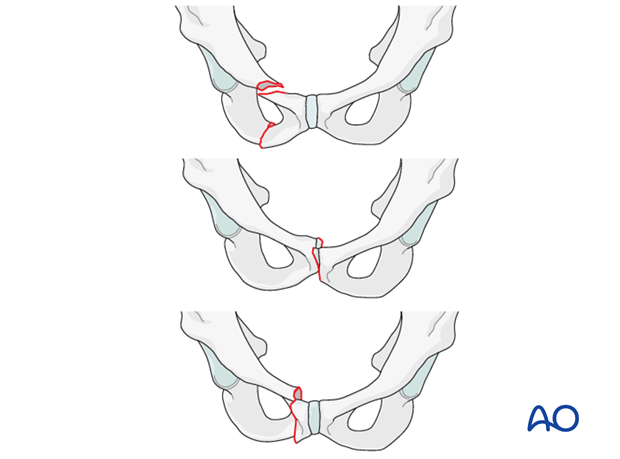
Occasionally, the anterior arch injury is a "locked symphysis", with overlapping pubic bodies,...
… and the "tilt fracture". The latter displaces a portion of one pubic body antero-inferiorly, disrupting the symphysis and ramus. The resulting deformity causes dyspareunia.
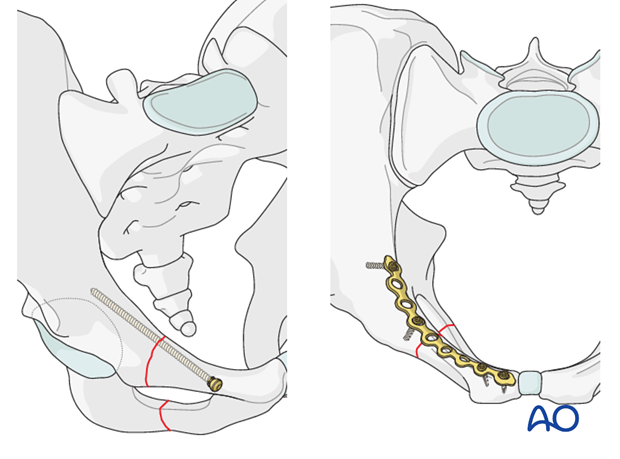
Both the "locked symphysis" and "tilt fractures" are indications for ORIF.
4. Lateral compression deformity
Significant deformity of lateral compression injuries may require reduction and fixation, even if little instability is evident.
Internal rotation of the hemipelvis can produce deformity which may obstruct the pelvic outlet, limit external rotation of the hip joint, or be unsightly.
Because of SI joint obliquity, internal rotation, if significant, also produces cephalad displacement of the acetabulum with apparent shortening of the lower extremity.
This apparent leg length discrepancy should not be confused with total pelvic ring instability.
5. Principles of treatment
Reduction
Anterior and/or posterior arch injuries may need to be disimpacted to achieve reduction of deformity. If performed in the first few days after injury this may be possible with closed manual reduction, perhaps aided by “joy stick” handles, or properly applied distraction external fixation.
Occasionally open reduction is required.
This is especially likely for locked symphysis and tilt fractures.
Fixation
After reduction of a lateral compression injury, fixation is advisable to prevent recurrence of deformity. The techniques chosen will depend upon the surgeon’s preference and the location of the injuries.
If the posterior arch has signs of instability its fixation may be advisable in addition to that of the anterior arch.
6. Sequence of reduction and fixation
Fixation sequence will depend upon the injury combination and the selected techniques.
Whichever option is selected, care should be taken not to fix one arch without confirming that alignment of the other is acceptable or achievable without removing the initial fixation.
Posterior fixation first
If the posterior ring is satisfactorily reduced and then fixed, there is usually still sufficient anterior arch mobility to allow CRIF of the superior ramus or external fixation.
Anterior fixation first
If significant anterior deformity is present, and it does not correct with closed manipulation or oblique external fixation, anterior open reduction and internal fixation should be carried out first, with optional posterior fixation if indicated.
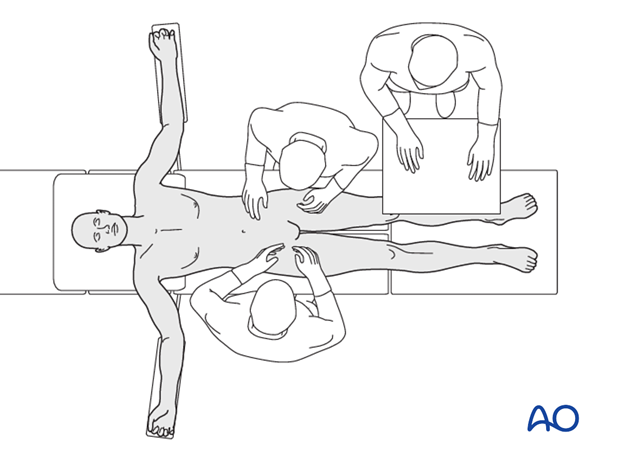
7. Patient preparation
This procedure is performed with the patient in a supine position.
8. Approaches
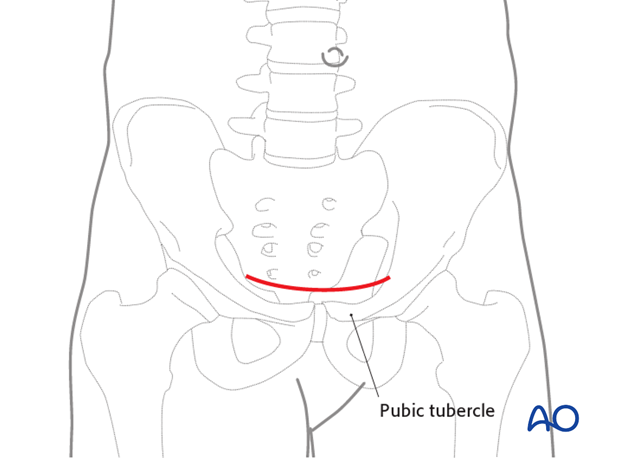
The standard horizontal (Pfannenstiel) approach to the symphysis is used for reduction and fixation of the pubis and medial ramus fractures.
For more lateral exposure of the pubic ramus, a lateral extension of the standard approach or a modified Stoppa incision may be necessary.
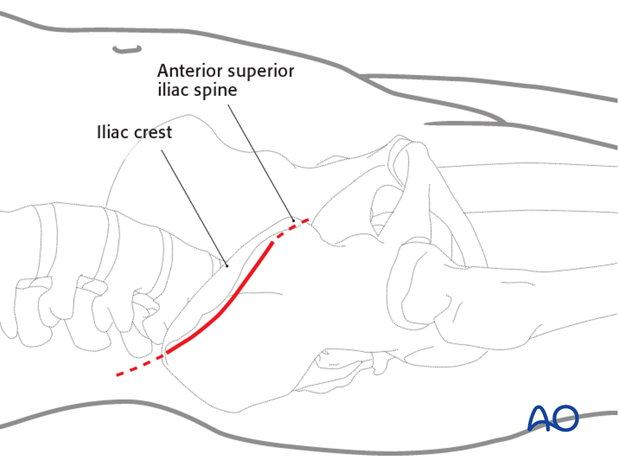
For access to an unstable iliac wing fracture, or the anterior part of the SI joint, including suitable crescent fractures, the anterior approach to the iliac wing is necessary.
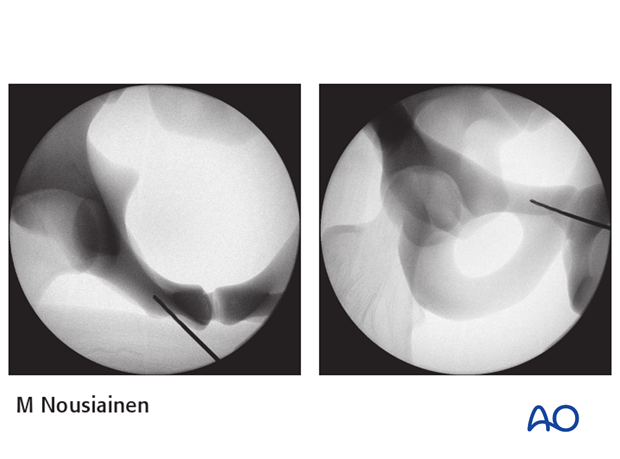
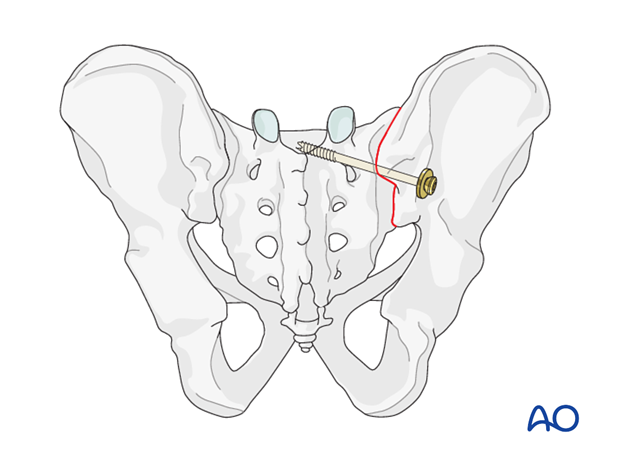
Pubic ramus intramedullary screws are inserted through stab wounds, either over the pubic tubercle (for retrograde insertion) or laterally over the acetabulum (for antegrade insertion).
The location of the stab wound is found using a C-arm and a K-wire.
For retrograde screw insertion, the surgeon stands on the opposite side of the table from the ramus being fixed.
9. Reduction and fixation
Reduction
If the initial alignment is satisfactory, and fixation is being performed primarily to prevent displacement, fixation proceeds without further reduction.
However, if significant deformity is present, reduction should start with closed manipulation of the ipsilateral lower extremity (flexion and/or external rotation, possibly with traction).
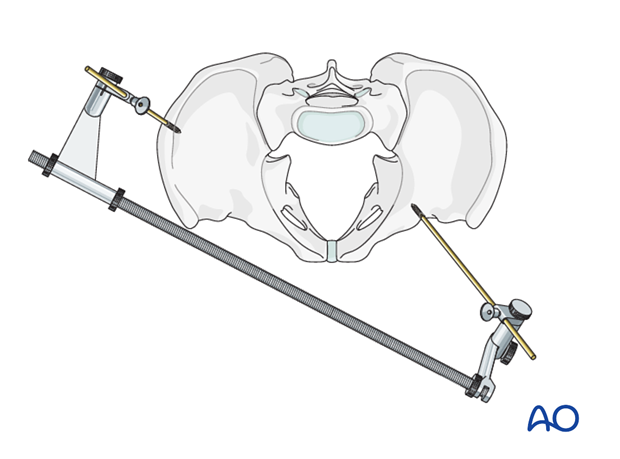
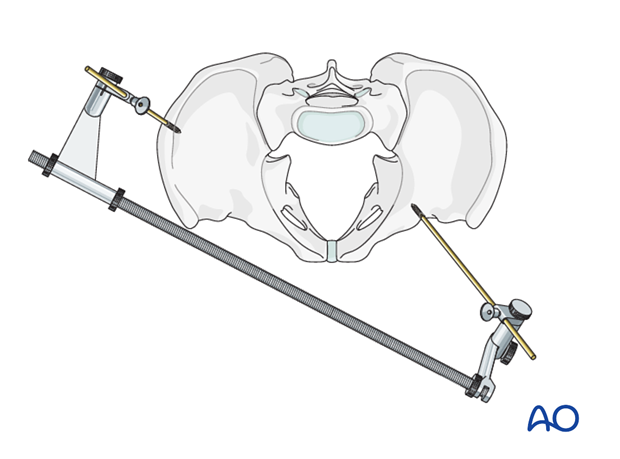
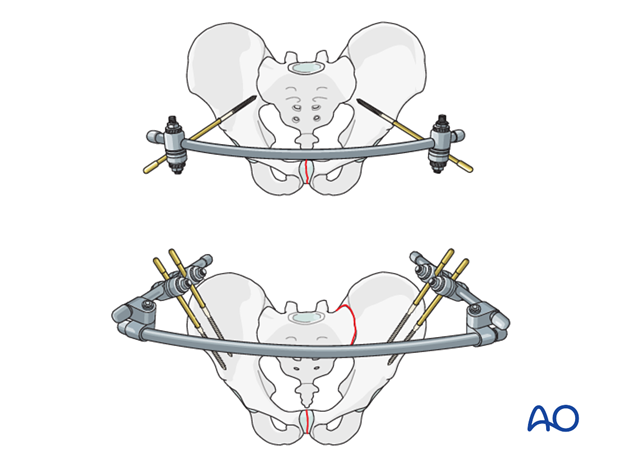
If manipulation with the leg is unsuccessful, percutaneous Schanz screws may permit direct manipulation of the deformed hemipelvis. This can be performed manually, or with a large distractor or external fixator.
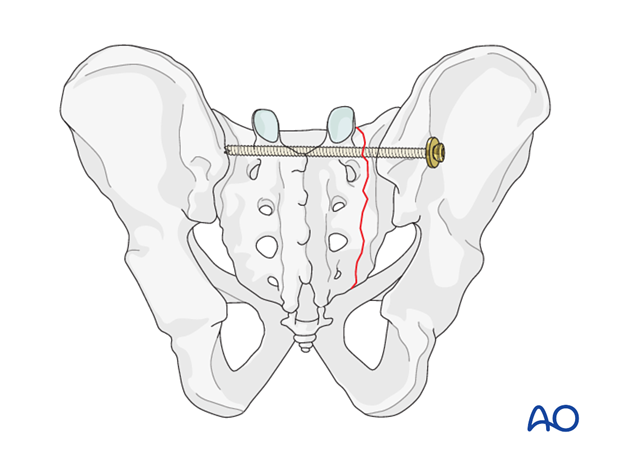
An oblique external fixator through which distraction is applied has been successful for reducing and maintaining alignment until the anterior arch heals.
Anterior fixation
Several different techniques of anterior arch fixation are available. While stable anterior arch fixation is desirable, strong evidence for selecting one technique instead of another does not yet exist.
Closed reduction and percutaneous superior ramus screws may avoid the encumbrance and pin site problems of external fixation. In intramedullary screw fixation failure rate may approach 15%. It is more common with retrograde screws, osteoporotic patients and more laterally ramus fractures. Supplementary posterior fixation (eg. ISS) may help prevent superior ramus screw loosening, and is worth considering for osteoporotic patients.
If a satisfactory reduction of the pubic ramus cannot be obtained closed, open reduction is indicated, in which case fixation can be performed with either a pubic ramus screw or plate.
If an external fixator is used for reduction, it is often sufficient for stabilization while a well aligned ramus fracture heals. This avoids an extensive exposure when a complex comminuted ramus fracture is present, yet satisfactory aligned.
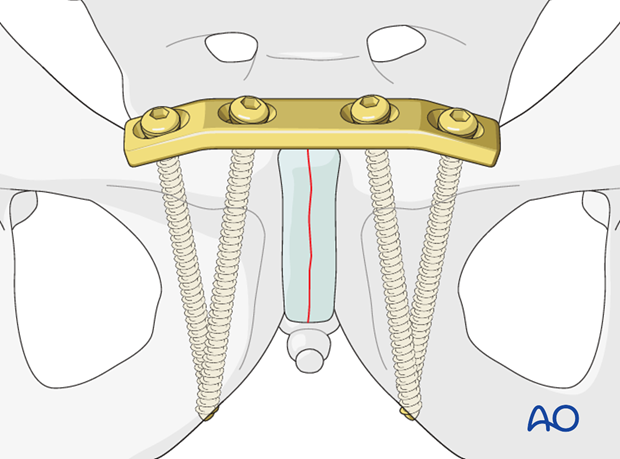
Pubic symphysis plating is indicated after reduction of a locked pubic symphysis.
Similarly, a pubic symphysis plate can be used, with a ramus screw or lateral plate extension, to fix a tilt fracture after open reduction.
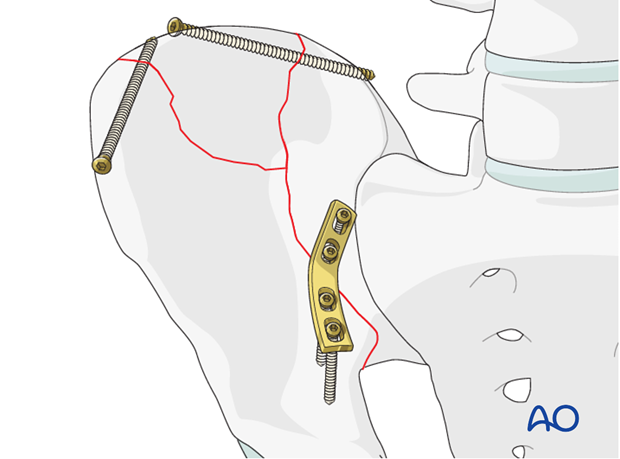
Posterior fixation
Posterior fixation may be indicated for potentially unstable sacral fractures (those that are complete from the anterior through the posterior sacral cortex, are comminuted, widely displaced, or associated with bilateral pubic ramus fractures). If instability is suspected, and definitely if it has resulted in progressive deformity, posterior fixation is advisable. This can usually be performed with iliosacral screw fixation.
If available, the use of intraoperative navigation may be beneficial.
ISS fixation of the SI joint is also suitable for smaller crescent fractures.
Larger crescent fractures can be repaired through an anterior (preferred) or posterior approach.
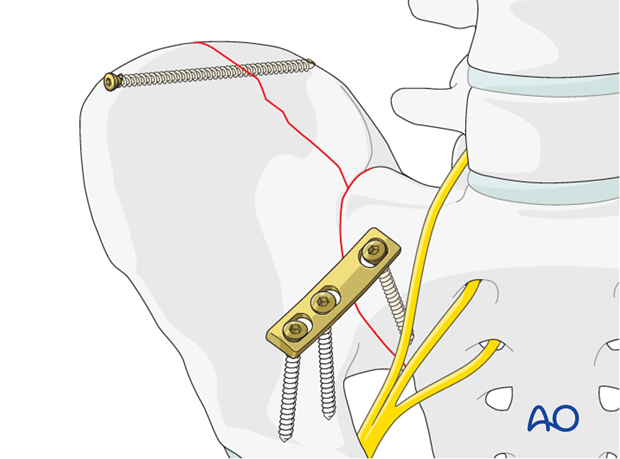
In the rare case of an incomplete iliac wing fracture, this should be repaired through the anterior approach to the iliac wing.
10. Check of osteosynthesis
Check the completed osteosynthesis with Imaging, and physical exam if there is any question about pelvic stability.
Using inlet and outlet views, with the C-arm, confirm that pelvic deformity has been corrected and that involved sacroiliac joints and pubic symphysis are anatomically reduced.
Unless a C-arm with a large field of view is available, it may be wise to obtain similarly oriented portable x-rays of the entire pelvis, to be certain about overall alignment.
Confirm that reduction of each fracture or joint injury is satisfactory, Make sure that all fixation devices are properly placed, and that each screw is of appropriate length. Multiple views are typically needed, including both axial and perpendicular views for questionable screws. If screws protrude from bone, consider risks to nerves, vessels, and adjacent viscera, especially urethra and bladder after pubic symphysis repair.

11. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













