Posterior ORIF SI fracture
1. Introduction
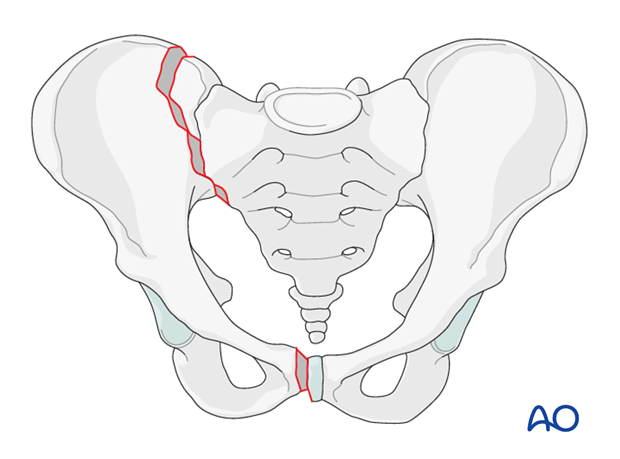
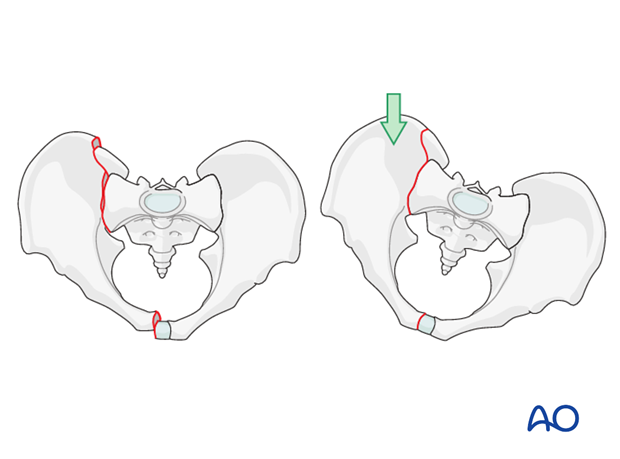
A crescent fracture is a fracture dislocation of the SI joint.
This injury involves a ligamentous disruption of the inferior part of the SI joint, and a vertical fracture of the posterior ilium that extends from the SI joint and exits the iliac crest.
The posterior superior iliac spine remains firmly attached to the sacrum via the superior portion of the posterior ligamentous complex.
The remaining anterior fragment is more mobile to internal rotation but remains relatively stable to external rotation and vertical forces.
This fracture is always combined with an injury to the anterior pelvis, most often fractures of the pubic rami.
These fractures are unstable.
When reducing and fixing the fracture of the iliac wing, the SI joint is indirectly reduced and the function of the posterior ligaments is restored.
Note to preparation and approach
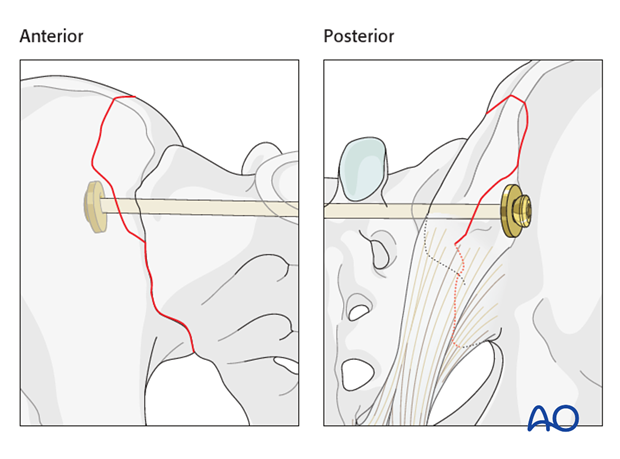
To allow a good reduction of the fracture, the posterior approach to the SI joint should be made slightly medial to the posterior iliac spine. One should not dissect through the gluteal muscles, but rather lift them from their attachment. This is to facilitate reduction and avoid invagination of the soft tissues.
Alternatively if the crescent fragment is large, fixation can be performed via an anterior approach.
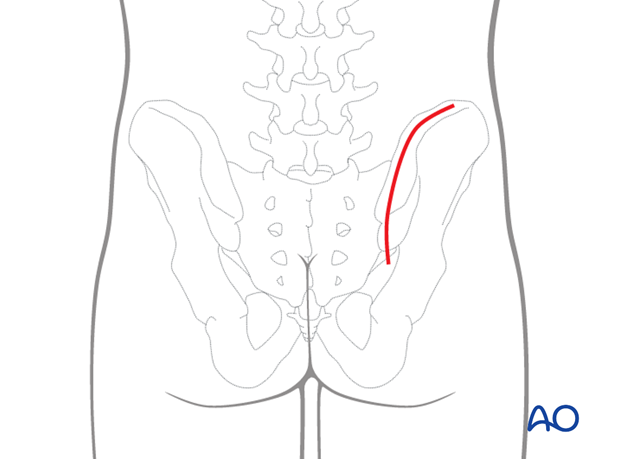
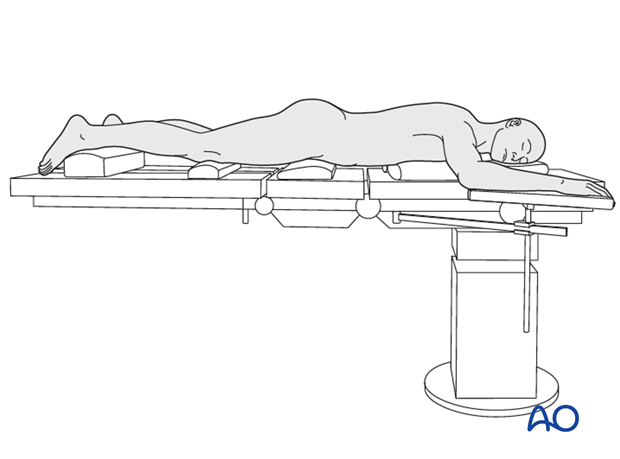
The patient is placed in a prone position. The thorax and abdomen should be placed on chest rolls without any pressure to the pelvis to facilitate manipulation of the pelvis as well as to facilitate ventilation of the patient during the operation.
Choice of fixation
Depending on the fracture line, the type of fixation may vary.
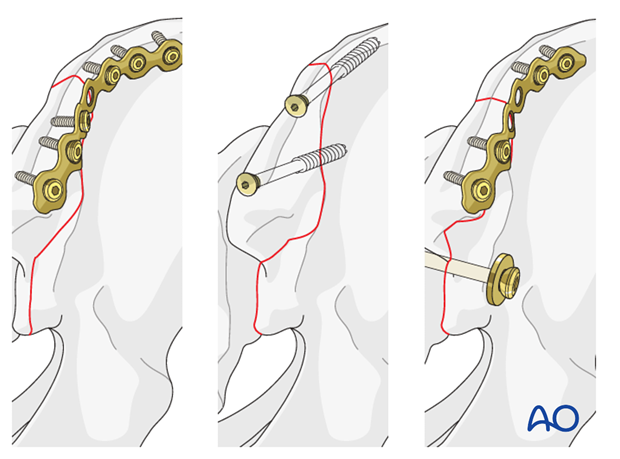
With small fragments, an additional SI screw may provide additional stability of the fixation.
2. Reduction
Preparation of fracture site
The fracture is exposed with a laminar spreader, cleaned of debris, interposed periosteum, and ligaments.
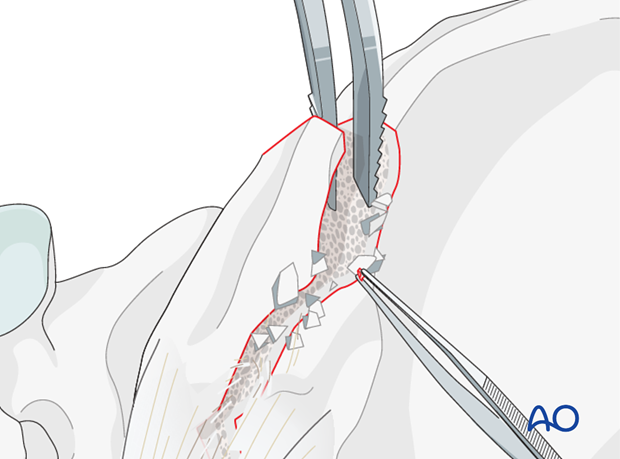
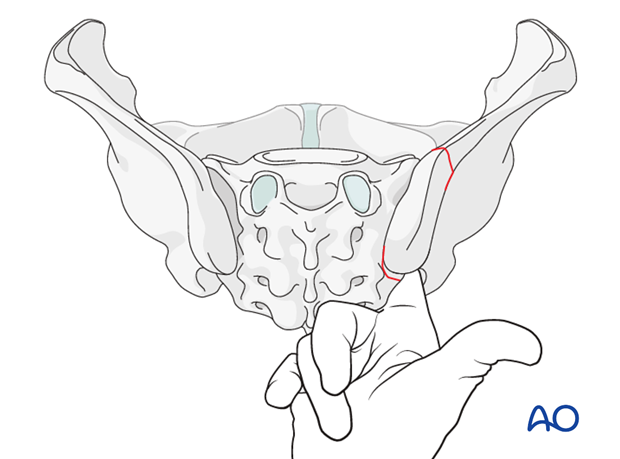
The fracture is reduced using pelvic clamps and reduction forceps. In some cases additional Schanz screws are inserted and used as joysticks.
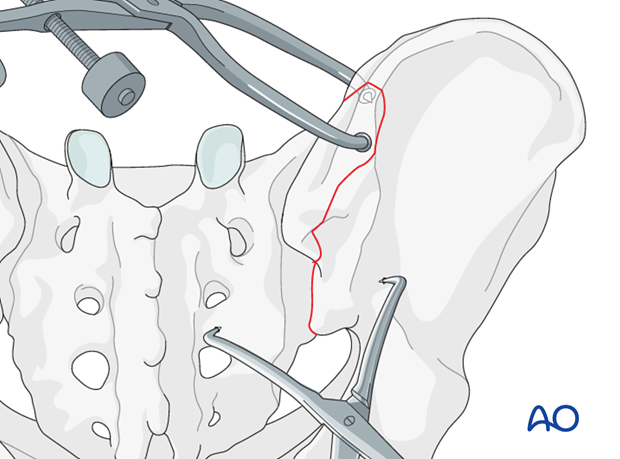
If the hemipelvis is displaced posteriorly, a slight rotation of the patient to the contralateral side may facilitate the reduction.
Reduction of the SI joint can be verified by palpating the anterior SI joint surface.
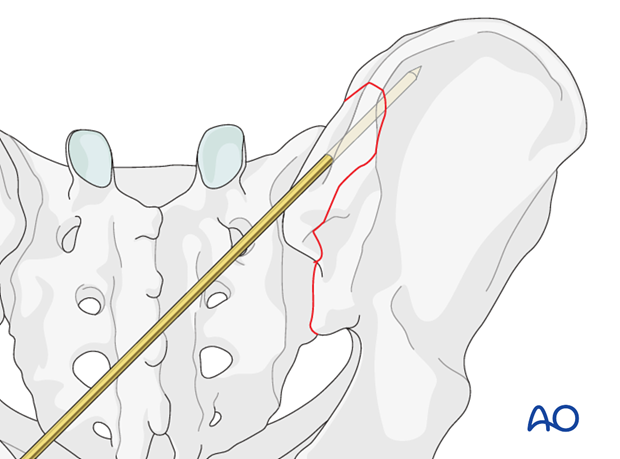
Temporary fixation
K-wires are inserted for temporary fixation.
3. Fixation
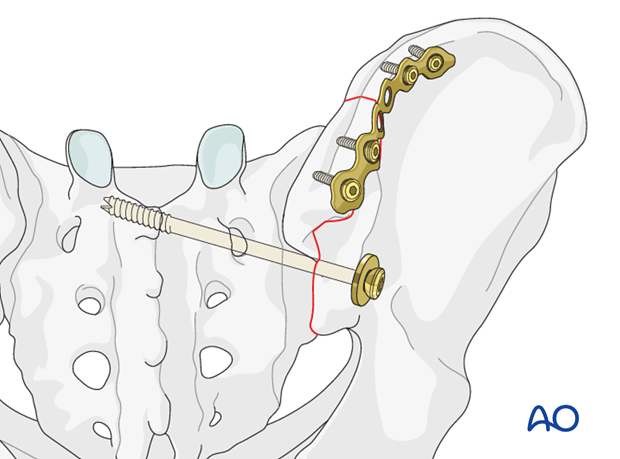
Plate selection
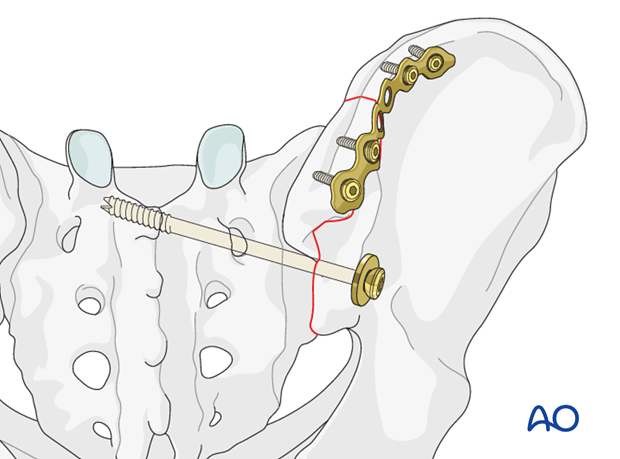
For large fragments, a 3.5 mm reconstruction plate is used. In osteoporotic bone, an angle stable plate is preferred.
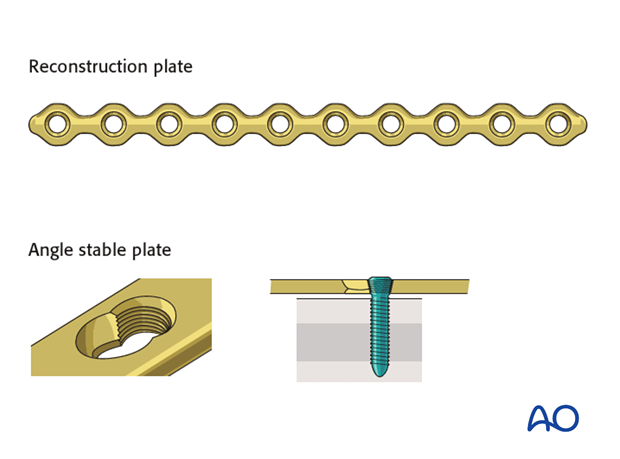
The plate is shaped to fit the contour of the bone and placed on the lateral rim.
Fixation is completed using bicortical screws.
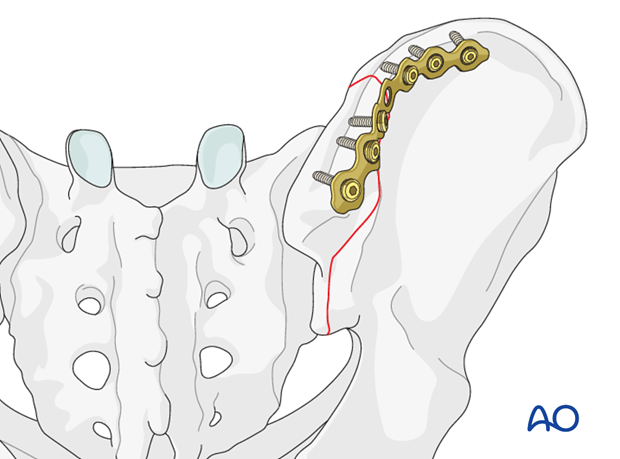
If the fracture plane is perpendicular to the iliac wing, stability may be increased using cancellous lag screws in addition to the plate.
Screws should not be used alone unless the bone quality is good.
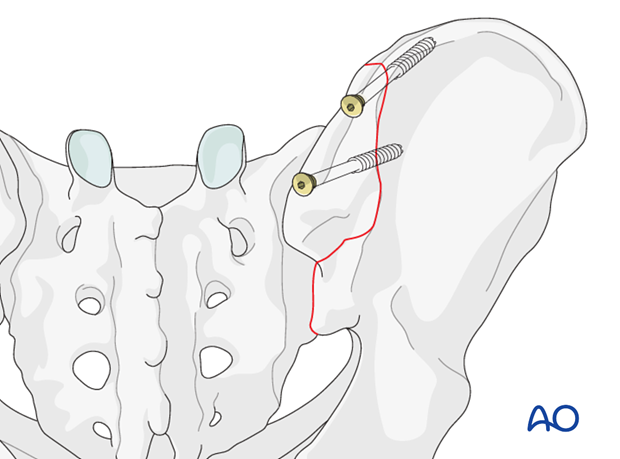
If the crescent fragment is small, a plate may not provide sufficient hold. Additional stability can be achieved by insertion of a SI screw.
The SI screw is inserted following the same principles as for the fixation of a SI dislocation.
4. X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.














