ORIF - Compression plating
1. Principles
Compression plate
The objective of compression plating is to produce absolute fracture stability, abolishing all interfragmentary motion.
Compression plating is useful in two-part fracture patterns, where the bone fragments can be compressed.
Dynamic compression principle
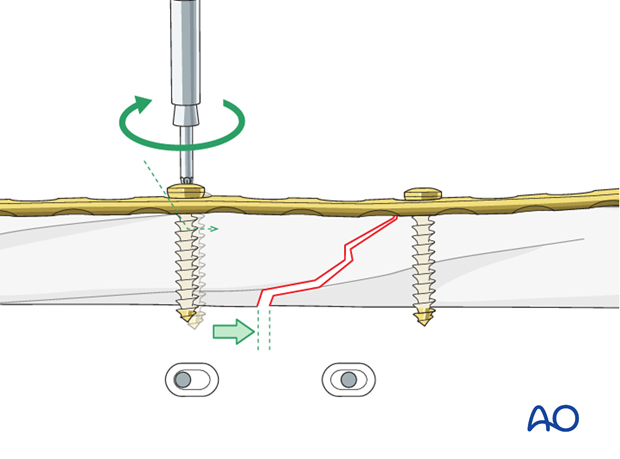
Compression of the fracture is usually produced by eccentric screw placement at one or more of the dynamic compression plate holes. These holes are shaped like an inclined and transverse cylinder. The screw head slides down the inclined cylinder as it is tightened, the head forcing the plate to move along the bone, thereby compressing the fracture.
Open fractures in the humeral shaft
Adequate surgical debridement is the crucial first step in the care of any open fracture.
Read more about the treatment of open fractures in the humeral shaft.
2. Choice of implant
Plate length
It is crucial to use a plate that is long enough on each side of the fracture. Plate length is more important than the number of screws for ensuring stability.
3. Plate position
Introduction
The choice of plate position depends on the fracture morphology and location, the radial nerve pathology and the surgeon’s preference. The anterolateral, anterior, and posterior surfaces of the humeral shaft are all possible choices.
The medial surface is generally only used for complex reconstructive procedures, ie vascular repair in complex fractures. Since the use of this plate position is rare it is not further shown.
The location should allow sufficient plate length on both proximal and distal segments, with a minimum of three holes for each.
For optimal compression, the plate should be positioned so that an “axilla” with one of the two fragments can be formed.
If the fracture location and orientation is suitable for lag screw fixation, consider applying a lag screw through the plate.
Be aware, that due to the soft-tissue attachments the optimal plate position for compression plating cannot always be obtained. In this case, it may be preferable to use lag screw(s) and a neutralization plate or bridge plating with locking plates to reduce soft-tissue dissection.
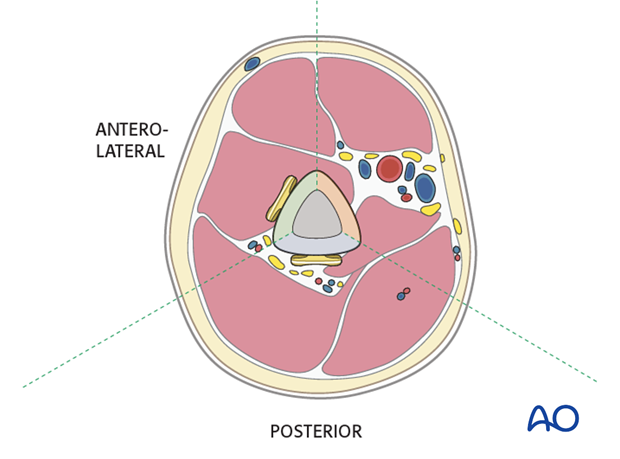
Anterolateral or anterior plate
An anterolateral plate fits well from very proximally to the distal fifth of the humerus and is selected if proximal and middle third fractures are present.
A plate in this position should provide stable fixation of the fracture and minimal soft-tissue damage.
Proximally, the plate may interfere with the deltoid insertion if it is placed laterally, or with the long head of the biceps tendon if the plate is positioned anteriorly. To overcome these problems the proximal end of the plate can be tunneled through the deltoid insertion.
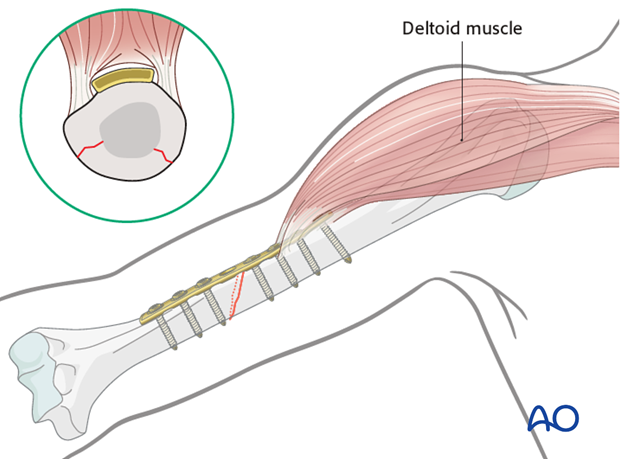
Distally the plate may be applied to the anterior or lateral surfaces.
Depending on the chosen positions for the proximal and distal plate ends, the plate may need to be contoured.
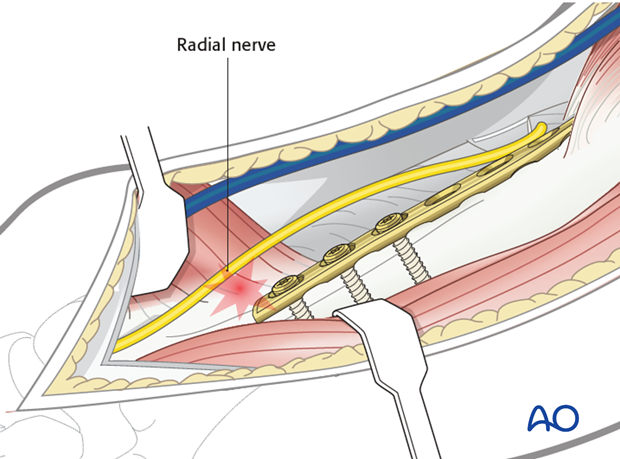
Neurological considerations should be taken into account. The radial nerve is at risk if the plate is applied to the lateral surface in the distal third. The plate should be twisted to ensure that the distal end avoids damaging the radial nerve.
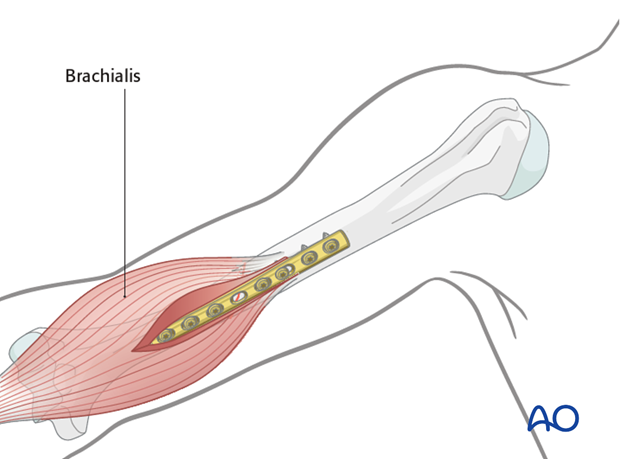
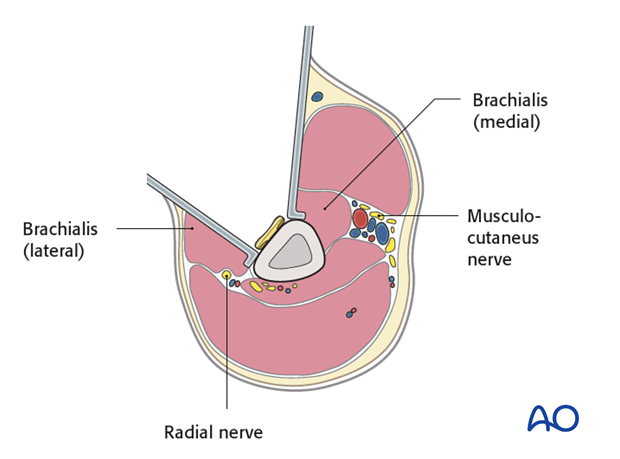
The innervation of the brachialis muscle is derived from both the radial and musculocutaneus nerves. The radial branch is at risk if the plate is applied to the anterior and anterolateral surfaces in the distal third while retracting the entire brachialis muscle medially. To avoid this it is safer to split the brachialis muscle.
If a small open fracture wound is present, the approach is made separately. Only if there is a large wound, after debridement, consider using the wound itself, with its necessary extensions, for plate insertion.
Posterior plate
The posterior surface is difficult to access proximally and limited by the axillary nerve. Therefore, posterior plating is best suited for middle and distal third fractures.
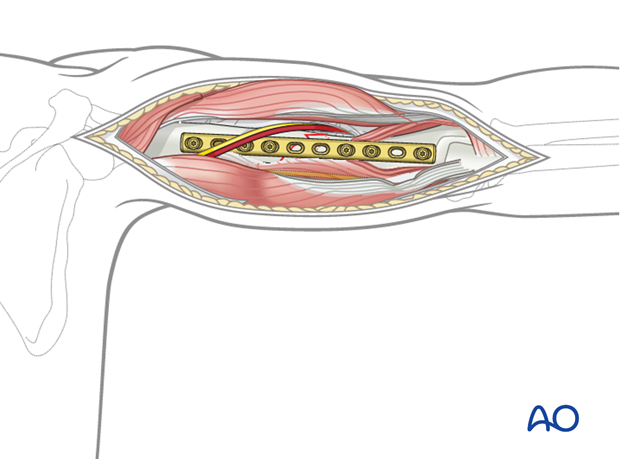
It is important to protect the radial nerve and its accompanying vessels in the spiral groove. If the plate interferes with the radial nerve, the plate must be placed underneath it. The course of the radial nerve in relation to the plate holes should be mentioned in the operation note. This will reduce the risk of accidental nerve damage if the plate should ever need to be removed.
4. Patient preparation and approaches
Patient positioning
Place the patient in a supine position or, alternatively, a beach chair position for placement of an anterolateral or anterior plate.
For placement of a posterior plate, a prone or lateral decubitus position is normally used.Approaches
The approach is selected depending on the chosen plate position.
For an anterolateral plate the anterolateral or extended deltopectoral approach may be used. For a more distal anterior or lateral plate, an anterolateral or lateral approach may be used.
The posterior surface can be accessed with a posterior approach (triceps-split or triceps-on approach).5. Reduction
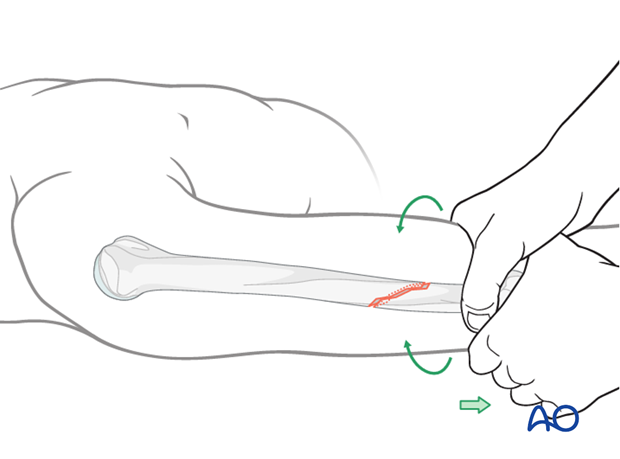
Manual reduction - limb realignment
Begin the reduction with traction on the distal humerus restoring bone length, tension in the soft tissues, realignment of the axis, and rotation.
Clear any interposed soft tissue by direct exposure. Preserve as much soft-tissue attachment as possible.
Pointed reduction forceps
Definitive reduction and fracture apposition is best performed with bone forceps, preferably with a pointed reduction forceps.
Align the fracture anatomically before tightening the forceps. It may be necessary to readjust to achieve this. If soft tissues have been preserved, the reduction may be difficult to assess.
Apply the clamp perpendicular to the fracture plane. Its position will mimic that of an appropriately placed lag screw.
Note: Care should be taken in poor bone quality. The reduction forces need to be applied gently to prevent further, iatrogenic fractures.
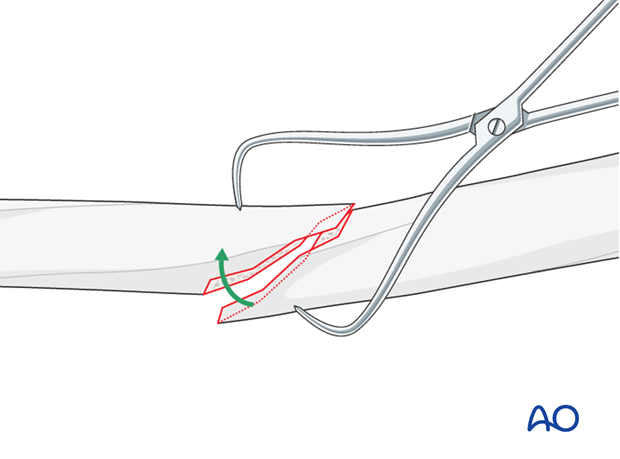
Reduction forceps can interfere with plate application for simple oblique fractures. If so, they may be placed through the plate hole of the intended lag screw position while the fracture is reduced and held. The plate is then applied, compressing the fracture and finally the lag screw is inserted.
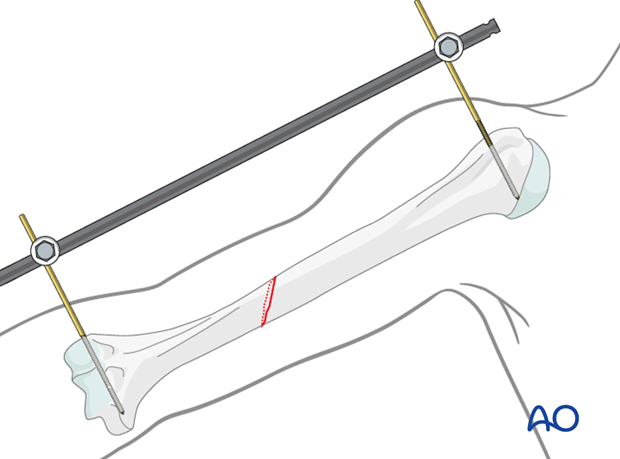
Reduction by external fixator or distractor
In nonunion with chronic shortening of the humerus it may become necessary to distract the fracture with an external fixator.
Oblique fractures are inherently unstable, so that an external fixator or a distractor may be necessary to maintain length. Such devices minimize soft-tissue injury if manual reduction is relied upon while the plate is being attached.
Insert proximal and distal pins outside the planned plate location. Take care not to injure the radial nerve. If in any doubt use incisions wide enough to allow palpation or direct visualization of the radial nerve.
Complete reduction may require additional correction of angulation or rotation. Folded linen bolsters under the fracture often help.
6. Plate contouring
Fitting the plate to the bone
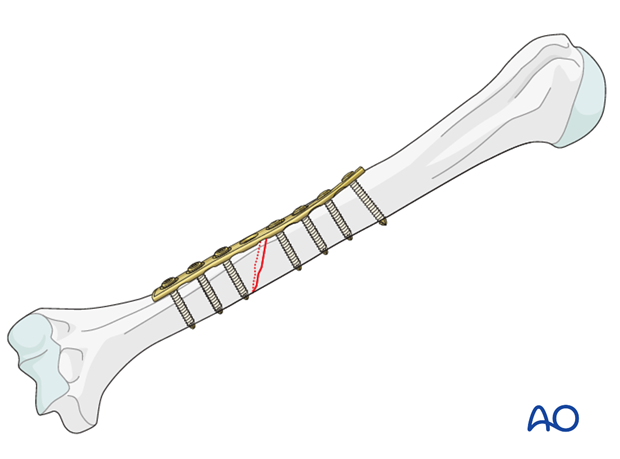
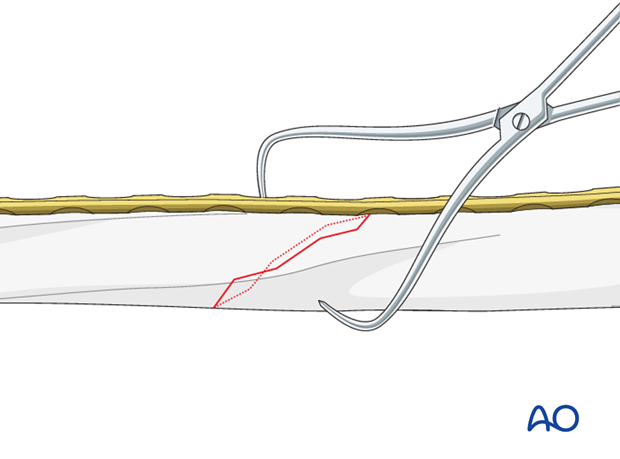
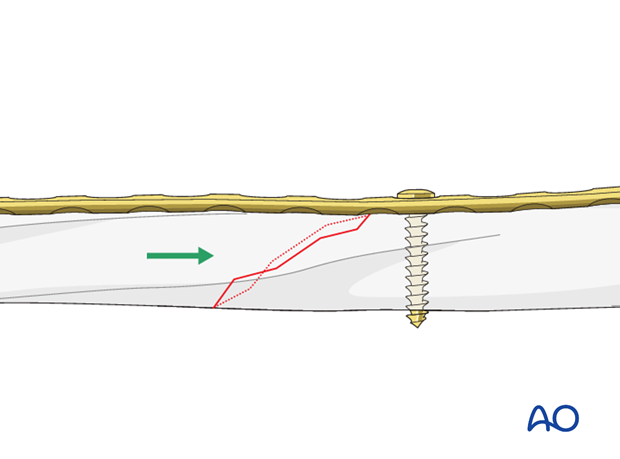
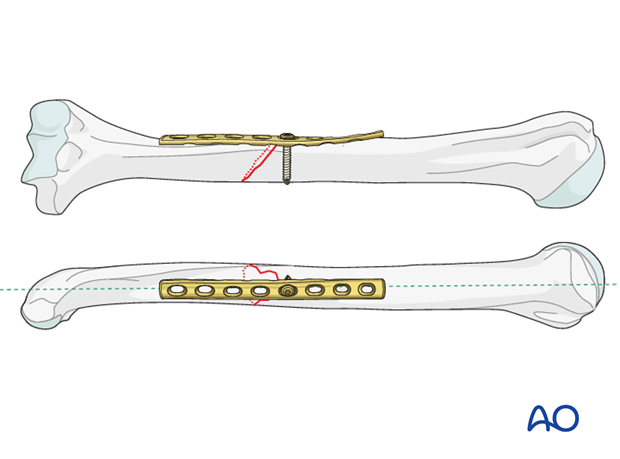
If possible, the plate should be positioned so that it lies directly over the distal end (as shown here) or the proximal end of an oblique or short spiral fracture plane. This position is best if the surgeon wishes to place a lag screw through the plate perpendicular to the fracture. Furthermore, when attached first to the fragment with which the plate makes an acute angle, the sharp end of the opposite bone fragment can be compressed securely into the "axilla" formed by the plate and the bone, to gain stable preloaded fixation.
If this optimal plate position requires an excessive soft-tissue detachment, alternative fixation principles should be considered.
Depending on the planned plate location, some contouring of the plate is likely to be necessary to fit the plate to the bone perfectly so that tightening its screws does not displace the fracture. This is true distally, posteriorly, and also on the anterolateral surface centrally. Sometimes twisting the plate around the shaft of the humerus provides a better fit and allows a longer plate.
Shape a malleable template to the bone surface. Use this template as a guide to shape the plate to fit the bone.
Use care to avoid fracture displacement while contouring the plate.

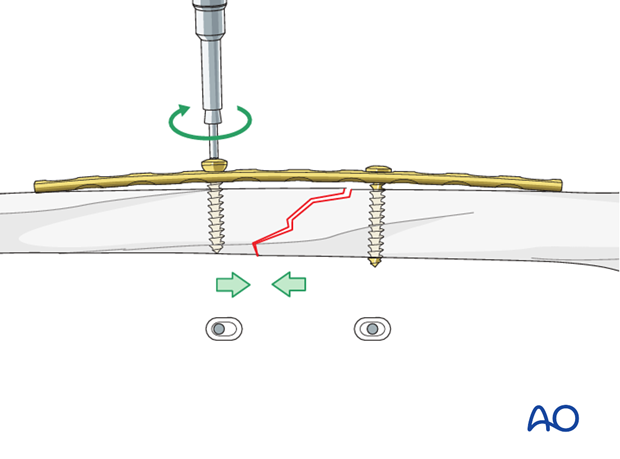
Overbending the plate
Even with oblique fractures, the plate should be slightly overbent (more convex) so that it does not fit perfectly on the bone. As the eccentrically placed screws are tightened in an overbent plate, the far (trans) cortex is compressed first. With further tightening, the near cortex also becomes compressed.
Such short, convex “overbend” can be made with the handheld bending pliers or bending irons.
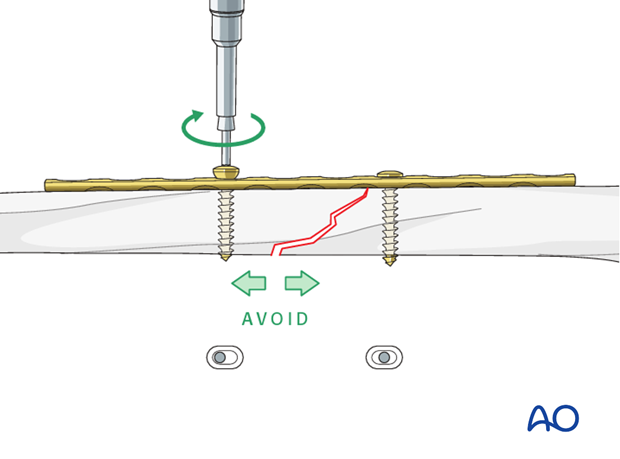
Pitfall: fracture opening opposite plate
When a transverse or short oblique fracture is compressed with a plate that is not overbent, compression will first be exerted at the cortex under the plate (cis cortex) and will cause gapping of the cortex opposite the plate (trans cortex).
An alternative to overbending can be lag screw insertion through the plate, across the fracture plane. This technique will also prevent gapping and micromotion.
In single plane fractures, such as this example, micromotion results in excessive strain of the healing tissues at the fracture site and also risks plate fatigue failure if union is slow.
7. Plate fixation
Application of the plate
Expose the bone sufficiently for plate application but do not strip the periosteum.
Center the plate over the fracture and hold it with a clamp in position.
Alternatively, and to confirm correct contouring, use a well-placed screw to hold the plate.
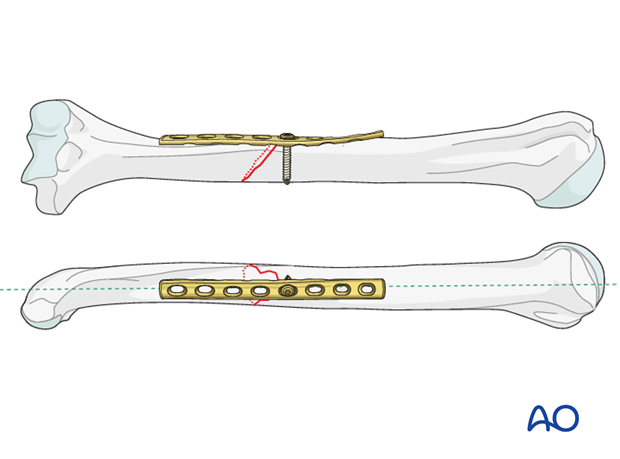
Creating an “axilla”
Attach the plate first to the fragment that will allow an “axilla” to be created between fracture surface and the plate.
Planning for a lag screw
When the obliquity is sufficient, a lag screw may be used to add additional stability to the fracture. This can be inserted through the plate after primary axial compression has been achieved. When planning a lag screw through the plate, it is important to assure that the plate is applied with a hole in a suitable position for the subsequent lag screw. If the lag screw cannot be placed perpendicular through the fracture plane, it does not add any further positive effect. Sometimes, the plate position on the humerus does not allow application of the lag screw through the plate without major soft-tissue dissection. In this case, either make sure the compression is adequate without a lag screw or use an alternative technique such as lag screw and neutralization plate.
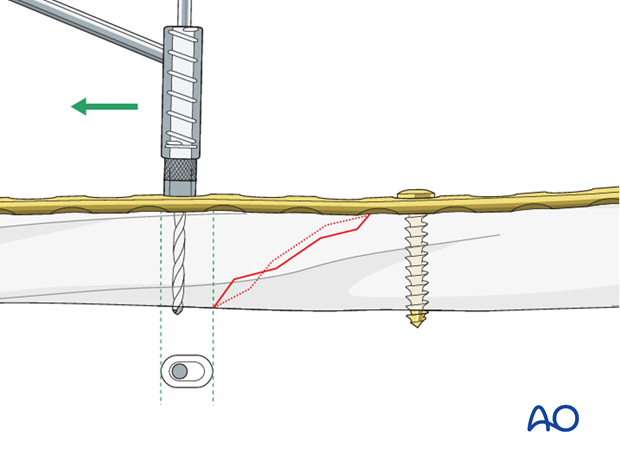
Drilling for first screw
Hold the plate in the desired position and drill through a hole close to the fracture.
Measure the depth.
Tap the cortices if non-self-tapping screws will be used.
Fixation of the plate with a first screw
Attach the plate with one screw to the pre-drilled fragment. Do not tighten the screw completely at this stage. Check plate fit and alignment and proceed with fracture reduction.
Bring the other fragment into position in the “axilla” between the plate and the fracture surface and check the reduction and plate alignment.
If there is concern of the strength of the screw hold in the bone add further screws to the same fragment.
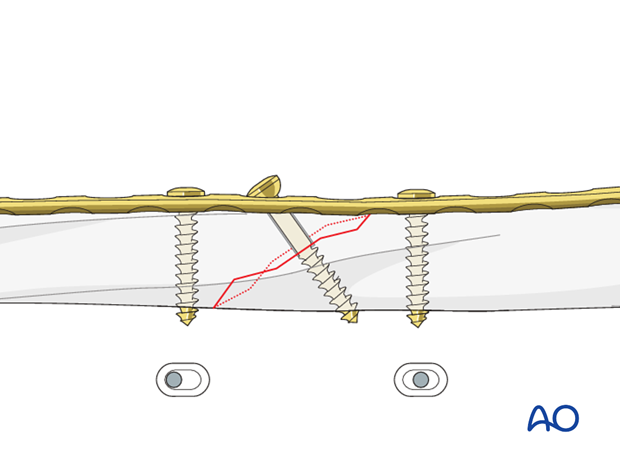
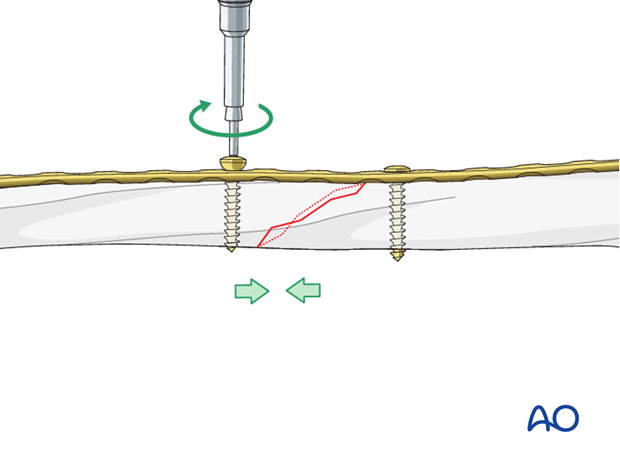
Eccentrical insertion of second screw
Insert a screw eccentrically into the other fragment, far enough away from the fracture to ensure the far cortex is on the same fragment, ie the screw does not cross the fracture. Make sure the hole for the planned lag screw is still available and in the correct position.
Confirm that the fracture surfaces are reduced, and that both ends of the plate fit satisfactorily.
Tightening of screws for fracture compression
Tighten both screws alternately, watching carefully to see that the reduction is maintained and compressed satisfactorily.
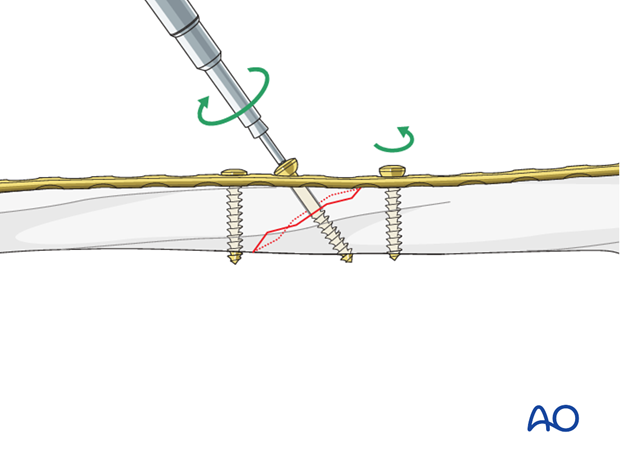
8. Lag screw addition
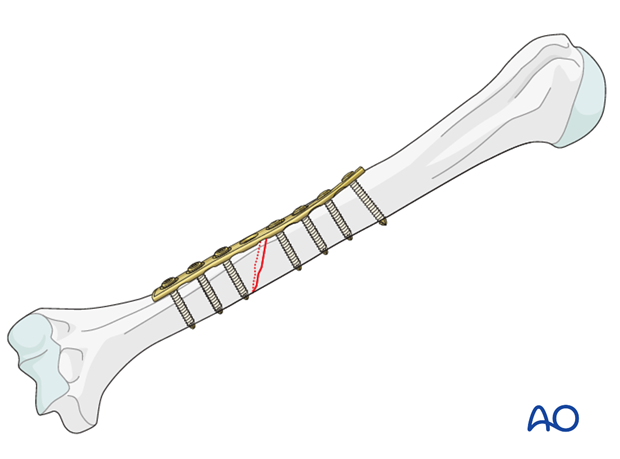
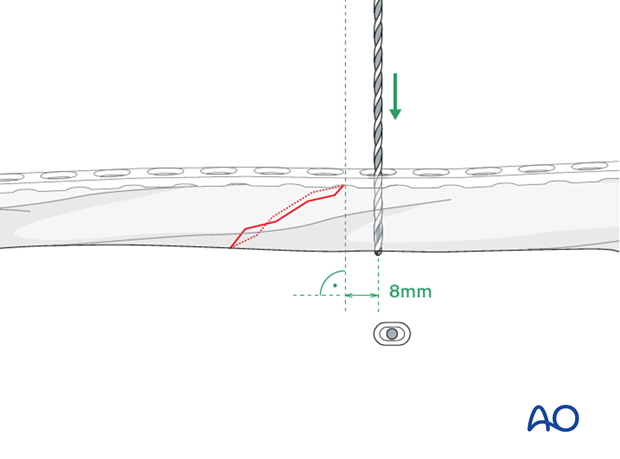
Insert a lag screw through the plate as perpendicular as possible to the fracture plane. Aim to pass it through the center of the fracture plane.
The insertion follows the principles of lag screw fixation:
- Drilling a pilot hole through both cortices
- Overdrilling the near cortex for gliding hole
- Tapping the far cortex for non-self-tapping screws
Before tightening the lag screw fully, release the axial compression slightly to allow additional interfragmentary compression.
Retighten the loosened screw after tightening of the lag screw.
9. Finalizing the fixation
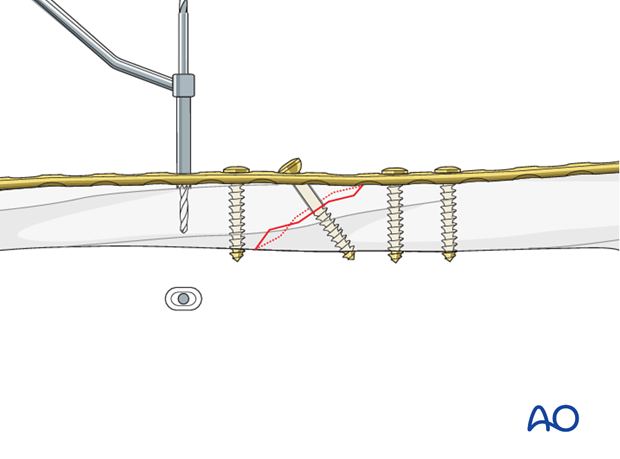
Insertion of remaining screws
Finally insert the remaining screws, first with the ones closest to the fracture site.
10. Final radiological assessment
Check for proper reduction and implant positions with image intensification in AP and lateral views.
Confirm also a proper torsional alignment of the humerus.
11. Aftercare
Principles
The aim of any surgical fixation of humeral shaft fractures is a stable osteosynthesis of the fracture allowing early passive and active motion. This is crucial to prevent elbow stiffness.
The rehabilitation regimen should take account of any damage to soft tissues, either as a result of the injury or due to the surgery. It also needs to take account of the security of the fixation.
Immediate postoperative care
Carefully examine the patient for neurological deficits and pulses.
Early treatment
In the beginning lymph drainage and elastocompressive bandages may be helpful.
Consider a sling for pain relief within the first days.
Treatment for refixation of deltoid detachment
If the deltoid was detached and reattached, active deltoid contraction should be delayed for the first six weeks.
Mobilization
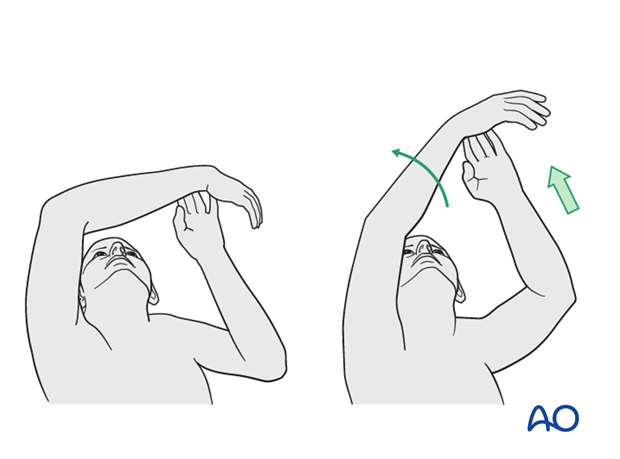
In the early phase the rehabilitation consists of classic maneuvers eg overhead motion exercises.
Rehabilitation should address the entire upper limb.
Exercise against resistance
Depending on the bone quality and compliance of the patient, exercise against resistance might be limited.
Follow-up
Clinical and radiological follow-up should be scheduled at least 6 weeks, 12 weeks and 6 months after surgery and continued until a bony healing is confirmed.
Hardware removal
Typically, humeral plates are left in situ indefinitely.
If removal is considered, bony healing should be confirmed. Plates are not normally removed for at least one year after surgery.
Be aware of the risk to the various nerves when dissecting the soft tissues to gain access to the distal humerus for removing anterior or anterolateral plates.
As the radial nerve runs over a posterior plate, removing this plate should only be considered with great caution, and the patient must be well informed about the risks. The original operation note should describe the relation of the nerve to the plate and should be reviewed before plate removal.













